Transgender Resiliency
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Resiliency Factors Among Transgender People of Color Maureen Grace White University of Wisconsin-Milwaukee
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by University of Wisconsin-Milwaukee University of Wisconsin Milwaukee UWM Digital Commons Theses and Dissertations May 2013 Resiliency Factors Among Transgender People of Color Maureen Grace White University of Wisconsin-Milwaukee Follow this and additional works at: https://dc.uwm.edu/etd Part of the Cognitive Psychology Commons, and the Educational Psychology Commons Recommended Citation White, Maureen Grace, "Resiliency Factors Among Transgender People of Color" (2013). Theses and Dissertations. 182. https://dc.uwm.edu/etd/182 This Dissertation is brought to you for free and open access by UWM Digital Commons. It has been accepted for inclusion in Theses and Dissertations by an authorized administrator of UWM Digital Commons. For more information, please contact [email protected]. RESILIENCY FACTORS AMONG TRANSGENDER PEOPLE OF COLOR by Maureen G. White A Dissertation Submitted in Partial Fulfillment of the Requirements for the Degree of Doctor of Philosophy in Educational Psychology at The University of Wisconsin-Milwaukee May 2013 ABSTRACT RESILIENCY FACTORS AMONG TRANSGENDER PEOPLE OF COLOR by Maureen G. White The University of Wisconsin-Milwaukee, 2013 Under the Supervision of Professor Dr. Shannon Chavez-Korell Much of the research on transgender individuals has been geared towards identifying risk factors including suicide, HIV, and poverty. Little to no research has been conducted on resiliency factors within the transgender community. The few research studies that have focused on transgender individuals have made little or no reference to transgender people of color. This study utilized the Consensual Qualitative Research (CQR) approach to examine resiliency factors among eleven transgender people of color. -

Opening the Door Transgender People National Center for Transgender Equality
opening the door the opening The National Center for Transgender Equality is a national social justice people transgender of inclusion the to organization devoted to ending discrimination and violence against transgender people through education and advocacy on national issues of importance to transgender people. www.nctequality.org opening the door NATIO to the inclusion of N transgender people AL GAY AL A GAY NATIO N N D The National Gay and Lesbian AL THE NINE KEYS TO MAKING LESBIAN, GAY, L Task Force Policy Institute ESBIA C BISEXUAL AND TRANSGENDER ORGANIZATIONS is a think tank dedicated to E N FULLY TRANSGENDER-INCLUSIVE research, policy analysis and TER N strategy development to advance T ASK FORCE F greater understanding and OR equality for lesbian, gay, bisexual T and transgender people. RA N by Lisa Mottet S G POLICY E and Justin Tanis N DER www.theTaskForce.org IN E QUALITY STITUTE NATIONAL GAY AND LESBIAN TASK FORCE POLICY INSTITUTE NATIONAL CENTER FOR TRANSGENDER EQUALITY this page intentionally left blank opening the door to the inclusion of transgender people THE NINE KEYS TO MAKING LESBIAN, GAY, BISEXUAL AND TRANSGENDER ORGANIZATIONS FULLY TRANSGENDER-INCLUSIVE by Lisa Mottet and Justin Tanis NATIONAL GAY AND LESBIAN TASK FORCE POLICY INSTITUTE National CENTER FOR TRANSGENDER EQUALITY OPENING THE DOOR The National Gay and Lesbian Task Force Policy Institute is a think tank dedicated to research, policy analysis and strategy development to advance greater understanding and equality for lesbian, gay, bisexual and transgender -
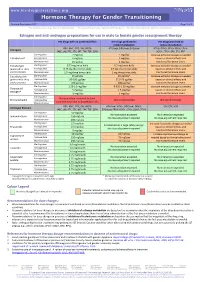
Hormone Therapy for Gender Transitioning Revised September 2017 Page 1 of 2 for Personal Use Only
www.hiv-druginteractions.org Hormone Therapy for Gender Transitioning Revised September 2017 Page 1 of 2 For personal use only. Not for distribution. For personal use only. Not for distribution. For personal use only. Not for distribution. Estrogen and anti-androgen preparations for use in male to female gender reassignment therapy HIV drugs with no predicted effect HIV drugs predicted to HIV drugs predicted to inhibit metabolism induce metabolism RPV, MVC, DTG, RAL, NRTIs ATV/cobi, DRV/cobi, EVG/cobi ATV/r, DRV/r, FPV/r, IDV/r, LPV/r, Estrogens (ABC, ddI, FTC, 3TC, d4T, TAF, TDF, ZDV) SQV/r, TPV/r, EFV, ETV, NVP Starting dose 2 mg/day 1 mg/day Increase estradiol dosage as needed Estradiol oral Average dose 4 mg/day 2 mg/day based on clinical effects and Maximum dose 8 mg/day 4 mg/day monitored hormone levels. Estradiol gel Starting dose 0.75 mg twice daily 0.5 mg twice daily Increase estradiol dosage as needed (preferred for >40 y Average dose 0.75 mg three times daily 0.5 mg three times daily based on clinical effects and and/or smokers) Maximum dose 1.5 mg three times daily 1 mg three times daily monitored hormone levels. Estradiol patch Starting dose 25 µg/day 25 µg/day* Increase estradiol dosage as needed (preferred for >40 y Average dose 50-100 µg/day 37.5-75 µg/day based on clinical effects and and/or smokers) Maximum dose 150 µg/day 100 µg/day monitored hormone levels. Starting dose 1.25-2.5 mg/day 0.625-1.25 mg/day Increase estradiol dosage as needed Conjugated Average dose 5 mg/day 2.5 mg/day based on clinical effects and estrogen† Maximum dose 10 mg/day 5 mg/day monitored hormone levels. -

Trans People, Transitioning, Mental Health, Life and Job Satisfaction
DISCUSSION PAPER SERIES IZA DP No. 12695 Trans People, Transitioning, Mental Health, Life and Job Satisfaction Nick Drydakis OCTOBER 2019 DISCUSSION PAPER SERIES IZA DP No. 12695 Trans People, Transitioning, Mental Health, Life and Job Satisfaction Nick Drydakis Anglia Ruskin University, University of Cambridge and IZA OCTOBER 2019 Any opinions expressed in this paper are those of the author(s) and not those of IZA. Research published in this series may include views on policy, but IZA takes no institutional policy positions. The IZA research network is committed to the IZA Guiding Principles of Research Integrity. The IZA Institute of Labor Economics is an independent economic research institute that conducts research in labor economics and offers evidence-based policy advice on labor market issues. Supported by the Deutsche Post Foundation, IZA runs the world’s largest network of economists, whose research aims to provide answers to the global labor market challenges of our time. Our key objective is to build bridges between academic research, policymakers and society. IZA Discussion Papers often represent preliminary work and are circulated to encourage discussion. Citation of such a paper should account for its provisional character. A revised version may be available directly from the author. ISSN: 2365-9793 IZA – Institute of Labor Economics Schaumburg-Lippe-Straße 5–9 Phone: +49-228-3894-0 53113 Bonn, Germany Email: [email protected] www.iza.org IZA DP No. 12695 OCTOBER 2019 ABSTRACT Trans People, Transitioning, Mental Health, Life and Job Satisfaction For trans people (i.e. people whose gender is not the same as the sex they were assigned at birth) evidence suggests that transitioning (i.e. -
Guidelines for Supporting Gender Transitioning Employees City and County of Denver, Office of Human Resources Revised July 22, 2020
Guidelines for Supporting Gender Transitioning Employees City and County of Denver, Office of Human Resources Revised July 22, 2020 Contents Contents ........................................................................................................................................................ 1 Purpose and Introduction ............................................................................................................................. 2 Terminology and Definitions ......................................................................................................................... 2 Applicable City and County of Denver Policies ............................................................................................. 3 Guidelines for Human Resources & Management ....................................................................................... 3 Guidelines for Co-Workers ............................................................................................................................ 4 Recommended Behaviors for LGBT Allies ................................................................................................ 4 Appearance, Names and Pronouns .......................................................................................................... 4 Benefits and Leave ........................................................................................................................................ 5 Sex-Segregated Facilities .............................................................................................................................. -

"Love Is Gender Blind": the Lived Experiences of Transgender Couples Who Navigate One Partner's Gender Transition Barry Lynn Motter
University of Northern Colorado Scholarship & Creative Works @ Digital UNC Dissertations Student Research 8-2017 "Love is Gender Blind": The Lived Experiences of Transgender Couples Who Navigate One Partner's Gender Transition Barry Lynn Motter Follow this and additional works at: https://digscholarship.unco.edu/dissertations Recommended Citation Motter, Barry Lynn, ""Love is Gender Blind": The Lived Experiences of Transgender Couples Who Navigate One Partner's Gender Transition" (2017). Dissertations. 428. https://digscholarship.unco.edu/dissertations/428 This Text is brought to you for free and open access by the Student Research at Scholarship & Creative Works @ Digital UNC. It has been accepted for inclusion in Dissertations by an authorized administrator of Scholarship & Creative Works @ Digital UNC. For more information, please contact [email protected]. © 2017 BARRY LYNN MOTTER ALL RIGHTS RESERVED UNIVERSITY OF NORTHERN COLORADO Greeley, Colorado The Graduate School “LOVE IS GENDER BLIND”: THE LIVED EXPERIENCES OF TRANSGENDER COUPLES WHO NAVIGATE ONE PARTNER’S GENDER TRANSITION A Dissertation Submitted in Partial Fulfillment of the Requirements for the Degree of Doctor of Philosophy Barry Lynn Motter College of Education and Behavioral Sciences Department of Applied Psychology and Counselor Education Program of Counseling Psychology August 2017 This Dissertation by: Barry Lynn Motter Entitled: “Love is Gender Blind:” The Lived Experiences of Transgender Couples Who Navigate One Partner’s Gender Transition has been approved as -

Experiences of Transgender Women/Transvestites with Access to Health Services: Progress, Limits, and Tensions
ESPAÇO TEMÁTICO: SAÚDE E DIREITOS DA POPULAÇÃO TRANS THEMATIC SECTION: TRANSGENDER HEALTH AND RIGHTS Experiências de acesso de mulheres trans/ travestis aos serviços de saúde: avanços, limites e tensões Experiences of transgender women/transvestites with access to health services: progress, limits, and tensions Experiencias de acceso de mujeres trans/travestis a servicios de salud: avances, límites y tensiones Simone Monteiro 1 Mauro Brigeiro 1 doi: 10.1590/0102-311X00111318 Resumo Correspondência S. Monteiro Laboratório de Educação em Ambiente e Saúde, Instituto Frente às mudanças e permanências nos costumes, normas e políticas sexuais Oswaldo Cruz, Fundação Oswaldo Cruz. no Brasil, o artigo analisa as experiências de acesso de mulheres trans/tra- Av. Brasil 4365, sala 49, Pavilhão Lauro Travassos, vestis aos serviços de saúde e discute a discriminação sexual/de gênero e as Rio de Janeiro, RJ 21045-900, Brasil. suas demandas aos serviços de transição de gênero e prevenção da aids. O [email protected] estudo envolveu entrevistas com nove mulheres trans/travestis, de 23-45 anos, 1 Instituto Oswaldo Cruz, Fundação Oswaldo Cruz, Rio de de das camadas populares da Baixada Fluminense, Rio de Janeiro, Brasil, rea- Janeiro, Brasil. lizadas em 2016, e observações de contextos de prostituição e sociabilidade. Comparando com as agressões vividas anos atrás, as narrativas das mulheres trans/travestis destacam avanços sociais. Relatam que os profissionais não as discriminam por sua condição, embora haja resistência ao uso do nome social. Esse constrangimento, somado aos problemas estruturais do Sistema Único de Saúde (SUS), são minimizados devido à agência das trans/travestis para obter atendimento, seja pelo recurso às redes de contatos, seja por sua consciência de direitos de cidadania. -

Gyn Care for the Transgender Patient
10/20/2017 Disclosures Gyn Care for the Transgender Patient I have consulted for Sage Therapeutics about post- Juno Obedin-Maliver, MD, MPH, MAS partum depression treatment and care pathways. University of California, San Francisco Assistant Professor (UCSF and SFVAMC) Co-Director, The PRIDE Study Founder, Stanford University LGBT Medical Education Research Group What the Evidence Tells Us San Francisco, CA 20 October 2017 Today’s Objectives Today’s Plan • Terminology • Why is this important? • Understand the difference between sex, gender, sexual • What do I need to know? orientation, gender identity, and gender expression. • Resources & Homework • Understand some of the reproductive health needs for transgender men & women Resources • Build a framework for providing sensitive and competent http://tinyurl.com/lwn6au5 gynecological care for transgender patients. 1 10/20/2017 Gender vs. Sex Are we talking, gender? Or A day in theSex? life of 5M prenatal… Terminology Right? Gender vs. Sex Gender vs. Sex Are we talking, gender? Are we talking, gender? Or Or A day in theSex? life of 5M A day in theSex? life of 5M prenatal… prenatal… Sex: But what if the The biological and physiological characteristics that define males and females. family gets Gender: The socially constructed roles, behaviors, activities, and attributes that a given Laverne instead society considers appropriate for men and women. of Jessie? “Male” and “female” are sex categories, while “man” and “woman” are gender categories. 2 10/20/2017 Gender vs. Sex Gender vs. Sex “Sex is what’s in your genes/jeans. “Gender identity is who you go to bed as. Gender identity is what’s between your ears.” Sexual orientation is who you go to bed with.” GenderThe Alphabet Identity Soupvs. -

Gender Transition, Expression and Identity Tool Kit Contents
GENDER TRANSITION, EXPRESSION AND IDENTITY TOOL KIT CONTENTS Gender Transition Page 1 Background 04 2 Gender identity and expression 05 3 Transition guidelines 07 3.1 Guidelines for transitioning individuals 08 3.1.1 Gender transition planning – considerations when preparing your plan 10 3.1.2 Sample FAQs to share with colleagues and clients 11 3.1.3 Example emails to communicate transition with colleagues 14 3.2 Guidelines for People representatives and line managers 16 3.2.1 Gender transition planning – practical steps for line managers and talent teams 18 Gender Identity 4 Gender identity and expression 20 5 An explanation of gender 22 6 Terminology 23 GENDER TRANSITION, EXPRESSION AND IDENTITY TOOL KIT | 03 1 2 BACKGROUND GENDER IDENTITY AND EXPRESSION At CBRE, we value diversity and inclusion and the creation of This document outlines some key terminology and language TRANS* AND TRANSGENDER A FEW FURTHER IMPORTANT POINTS a workplace that supports everyone. When an employee around gender variance and gender transition in particular, Gender identity and expression is a complex subject, and it’s Correct use of pronouns works in an inclusive workplace, they have the best and provides what we hope is useful general guidance for important to clarify what this tool kit is focused on. Trans* Using the correct pronouns (he, she, they, etc.) is opportunity to reach their full potential. We are committed to gender transition within the working environment, and how (with an asterisk) is an umbrella term for people whose extremely important. Simply ask the individual fairness and equality in the provision of working conditions, all colleagues can be supportive. -

Experiences with Formal and Informal Support: a Case Study of a Female-To-Male Transgender Individual
Pepperdine University Pepperdine Digital Commons Theses and Dissertations 2014 Experiences with formal and informal support: a case study of a female-to-male transgender individual Jessica Magallanes Follow this and additional works at: https://digitalcommons.pepperdine.edu/etd Recommended Citation Magallanes, Jessica, "Experiences with formal and informal support: a case study of a female-to-male transgender individual" (2014). Theses and Dissertations. 408. https://digitalcommons.pepperdine.edu/etd/408 This Dissertation is brought to you for free and open access by Pepperdine Digital Commons. It has been accepted for inclusion in Theses and Dissertations by an authorized administrator of Pepperdine Digital Commons. For more information, please contact [email protected], [email protected], [email protected]. Pepperdine University Graduate School of Education and Psychology EXPERIENCES WITH FORMAL AND INFORMAL SUPPORT: A CASE STUDY OF A FEMALE-TO-MALE TRANSGENDER INDIVIDUAL A clinical dissertation submitted in partial satisfaction of the requirements for the degree of Doctor of Psychology by Jessica Magallanes, M.A. February, 2014 Shelly Harrell, Ph.D. – Dissertation Chairperson This clinical dissertation, written by Jessica Magallanes, M.A. under the guidance of a Faculty Committee and approved by its members, has been submitted to and accepted by the Graduate Faculty in partial fulfillment of the requirements for the degree of DOCTOR OF PSYCHOLOGY Doctoral Committee: Shelly Harrell, Ph.D., Chairperson -

Gender Transition Guidelines for UPMC
Gender Transition Guidelines for UPMC 1.0 SCOPE 1.1 OBJECTIVE – UPMC is committed to creating a culture in which the unique attributes of each person are understood, valued, respected, and utilized. To that end, the encompassed Gender Transition Guidelines provides the UPMC workforce with information to support an employee through a gender transition. These guidelines provide a plan to support the transitioning employee, her/his manager, co-workers, and Human Resources of respective roles, responsibilities, and expectations in the process. The guidelines are meant to be flexible enough to customize a transition plan specific to the circumstances of a gender-transitioning employee, yet specific enough to provide a consistent framework to manage the transition process. UPMC employees are encouraged to follow the protocols in this guideline when a transgender employee is transitioning. If at any point one is unfamiliar with the terminology or process surrounding a gender transition, it may be helpful to first contact the Center for Engagement and Inclusion for the necessary support and guidance. 2.0 DEFINITIONS 2.1 Sex - The term “sex” refers to the classification of people as male or female. At birth, infants are assigned a sex based on a combination of biological characteristics including: chromosomes, hormones, and reproductive organs. 2.2 Gender - The term “gender,” while often used interchangeably with “sex,” can refer specifically to the behavioral, cultural, psychological, or social traits typically associated with one sex, rather than biological characteristics. Note: “Male” and “female” are sex categories, while “masculine” and “feminine” are gender categories. 2.3 Gender Identity - The term “gender identity” distinct from the term “sexual orientation” refers to a person’s innate, deeply felt psychological sense of gender, which may or may not correspond to the person’s body or designated sex at birth (the sex originally listed on a person’s birth certificate). -

A Qualitative Inquiry of Black Transgender Men's Experiences
SHIFTING IDENTITIES: A QUALITATIVE INQUIRY OF BLACK TRANSGENDER MEN’S EXPERIENCES Mickey E. White Dissertation Prepared for the Degree of DOCTOR OF PHILOSOPHY UNIVERSITY OF NORTH TEXAS August 2019 APPROVED: Angie D. Cartwright, Major Professor Caitlyn M. Bennett, Committee Member Anneliese A. Singh, Committee Member Natalya Lindo, Committee Member and Chair of the Department of Counseling and Higher Education Randy Bomer, Dean of the College of Education Victor Prybutok, Dean of the Toulouse Graduate School White, Mickey E. Shifting Identities: A Qualitative Inquiry of Black Transgender Men’s Experiences. Doctor of Philosophy (Counseling), August 2019, 256 pp., 1 table, 6 appendices, comprehensive reference list, 357 titles. The purpose of this transcendental phenomenological study was to explore Black transgender men’s experiences navigating systems of racism and transphobia. To this end, I utilized a critical race theory and intersectionality theory framework to answer the following question: What are Black transgender men’s experiences with power, privilege, and oppression? The ten Black transgender men and transmasculine people who participated in this study provided detailed and moving accounts of their experiences with systems of oppression. Six major themes were prominent throughout participant narratives: (1) developing an empowered view of self, (2) navigating double consciousness, (3) having a target on your back, (4) strategies of resilience, (5) culture of silence, and (6) finding quality care. Overall, participants offered insight and keen awareness of their intersecting racial and gender identities, as well as speaking intimately about how the shift from societal perceptions and identification as a Black woman to a Black man impacted their sense of self and views of the world.