Dose Reduction and Cardiopulmonary Effects of Anesthetic Induction with Propofol with Or Without Midazolam in Critical Canine Patients
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Handheld Devices and Informatics in Anesthesia Prasanna Vadhanan,MD1, Adinarayanan S., DNB2
COMMENTRY Handheld devices and informatics in anesthesia Prasanna Vadhanan,MD1, Adinarayanan S., DNB2 1Associate Professor, Department of Anaesthesiology, Vinayaka Missions Medical College & Hospital, Keezhakasakudimedu, Kottucherry Post, Karaikal, Puducherry 609609, (India) 2Associate Professor, Department of Anaesthesiology & Critical Care. The Jawaharlal Institute of Postgraduate Medical Education & Research, Dhanvantri Nagar, Gorimedu, Puducherry, 605006, (India) Correspondence: Dr. Prasanna Vadhanan, MD, No. 6, P&T Nagar, Mayiladuthurai 609001 (India); Phone: +919486489690; E-mail: [email protected] Received: 02 April 2016; Reviewed: 2 May 2016; Corrected: 02 June 2016; Accepted: 10 June 2016 ABSTRACT Handheld devices like smartphones, once viewed as a diversion and interference in the operating room have become an integral part of healthcare. In the era of evidence based medicine, the need to remain up to date with current practices is felt more than ever before. Medical informatics helps us by analysing complex data in making clinical decisions and knowing recent advances at the point of patient care. Handheld devices help in delivering such information at the point of care; however, too much reliance upon technology might be hazardous especially in an emergency situation. With the recent approval of robots to administer anesthesia, the question of whether technology can replace anesthesiologists from the operating room looms ahead. The anesthesia and critical care related applications of handheld devices and informatics -

Jebmh.Com Original Research Article
Jebmh.com Original Research Article A COMPARATIVE STUDY OF SMALL DOSE OF KETAMINE, MIDAZOLAM AND PROPOFOL AS COINDUCTION AGENT TO PROPOFOL Abhimanyu Kalita1, Abu Lais Mustaq Ahmed2 1Senior Resident, Department of Anaesthesiology, Assam Medical College, Dibrugarh. 2Associate Professor, Department of Anaesthesiology, Assam Medical College, Dibrugarh. ABSTRACT BACKGROUND The technique of “coinduction”, i.e. use of a small dose of sedative agent or another anaesthetic agent reduces the dose requirement as well as adverse effects of the main inducing agent. Ketamine, midazolam and propofol have been used as coinduction agents with propofol. MATERIALS AND METHODS This prospective, randomised clinical study compared to three methods of coinduction. One group received ketamine, one group received midazolam and one group received propofol as coinducing agent with propofol. RESULTS The study showed that the group receiving ketamine as coinduction agent required least amount of propofol for induction and was also associated with lesser side effects. CONCLUSION Use of ketamine as coinduction agent leads to maximum reduction of induction dose of propofol and also lesser side effects as compared to propofol and midazolam. KEYWORDS Coinduction, Propofol, Midazolam, Ketamine. HOW TO CITE THIS ARTICLE: Kalita A, Ahmed ALM. A comparative study of small dose of ketamine, midazolam and propofol as coinduction agent to propofol. J. Evid. Based Med. Healthc. 2017; 4(64), 3820-3825. DOI: 10.18410/jebmh/2017/763 BACKGROUND But, the major disadvantage of propofol induction are Propofol is the most frequently used IV anaesthetic agent impaired cardiovascular and respiratory function, which may used today with a desirable anaesthetic profile. It provides put the patients at a higher risk of bradycardia, hypotension faster onset of action, antiemesis, rapid recovery with and apnoea. -
Update on the Management of Pain, Agitation, and Delirium in the ICU
Update on the Management of Pain, Agitation, and Delirium in the ICU Kevin E. Anger, Pharm.D., BCPS Gilles Fraser, Pharm.D., MCCM Paul M. Szumita, Pharm.D., BCCCP, Manager Investigational Drug Clinical Pharmacist in Critical BCPS, FCCM Service Brigham and Women’s Care Clinical Pharmacy Practice Manager Hospital Maine Medical Center Brigham and Women’s Hospital Boston, Massachusetts Portland, Maine Boston, Massachusetts Disclosures • Faculty have nothing to disclose. Objectives • Describe recent literature on management of pain, agitation, and delirium (PAD) in the intensive care unit (ICU). • Apply key concepts in the selection of sedatives, analgesics, and antipsychotic agents in critically ill patients. • Recommend methods to overcome key barriers to optimizing pain, sedation, and delirium pharmacotherapy in critically ill patients. Case-Based Approach to Pain Management in the ICU Kevin E. Anger, Pharm.D., BCPS Manager Investigational Drug Service Brigham and Women’s Hospital Boston, Massachusetts Time for a Poll How to vote via the web or text messaging From any browser From a text message Pollev.com/ashp 22333 152964 How to vote via text message How to vote via the web Question #1 DT is a 70 yo male w/ COPD, S/P XRT for NSC lung CA, now admitted to the medical ICU for respiratory failure secondary to pneumonia meeting ARDS criteria. Significant home medications include oxycodone sustained release 40mg TID, oxycodone 10- 20mg Q4hrs PRN pain, Advair 500/50mcg BID, ASA 81mg QD, and albuterol neb Q4hrs PRN. DT is intubated is currently -

Pharmacists' Roles on the Pain Management Team, Fall 2014
Fall 2014, Volume 8, Issue 2 Canadian Pharmacy > Research > Health Policy > Practice > Better Health Pharmacists’ Roles on the Pain Management Team harmacists are an important resource for managing pain in their patients, in order to both optimize treatment and Pprevent the unintended consequences of potent analgesics. While the role of pharmacists in pain management was first addressed inthe Translator Summer 2012 edition1, this rapidly evolving area of pharmacy practice has generated a number of innovative models that highlight the unique role of the pharmacist. As Canadian pharmacists embrace expanded scopes of practice, there is an opportunity to specifically leverage their services to assist patients in managing their pain. This issue of the Translator highlights four different approaches to enhanced involvement of pharmacists in the management of chronic pain: n Pharmacist-led management of chronic pain: a randomized controlled exploratory trial from the UK n A pharmacist-initiated intervention trial in osteoarthritis n A pharmacist-led pain consultation for patients with concomitant substance use disorders n The impact of pharmacists in translating evidence to patients with low back pain 1 The Translator, Summer 2012, 6:3 Pharmacist-led management of chronic pain in primary care: results from a randomized controlled exploratory trial Bruhn H, Bond CM, Elliott AM, et al. Pharmacist-led management of chronic pain in primary care; results from a randomized controlled exploratory trial. BMJ Open 2013;3:e002361. Issue: In the UK, an estimated 80% of medication review of each patient’s medical chronic pain sufferers still report pain after Pharmacist prescribing and records, followed by a face-to-face consul- four years of follow-up.1 Most patients refer reviewing pain medication may tation. -

Pain Management in People Who Have OUD; Acute Vs. Chronic Pain
Pain Management in People Who Have OUD; Acute vs. Chronic Pain Developer: Stephen A. Wyatt, DO Medical Director, Addiction Medicine Carolinas HealthCare System Reviewer/Editor: Miriam Komaromy, MD, The ECHO Institute™ This project is supported by the Health Resources and Services Administration (HRSA) of the U.S. Department of Health and Human Services (HHS) under contract number HHSH250201600015C. This information or content and conclusions are those of the author and should not be construed as the official position or policy of, nor should any endorsements be inferred by HRSA, HHS or the U.S. Government. Disclosures Stephen Wyatt has nothing to disclose Objectives • Understand the complexities of treating acute and chronic pain in patients with opioid use disorder (OUD). • Understand the various approaches to treating the OUD patient on an agonist medication for acute or chronic pain. • Understand how acute and chronic pain can be treated when the OUD patient is on an antagonist medication. Speaker Notes: The general Outline of the module is to first address the difficulties surrounding treating pain in the opioid dependent patient. Then to address the ways that patients with pain can be approached on either an agonist of antagonist opioid use disorder treatment. Pain and Substance Use Disorder • Potential for mutual mistrust: – Provider • drug seeking • dependency/intolerance • fear – Patient • lack of empathy • avoidance • fear Speaker Notes: It is the provider that needs to be well educated and skillful in working with this population. Through a better understanding of opioid use disorders as a disease, the prejudice surrounding the encounter with the patient may be reduced. -

A Novel Checklist for Anesthesia in Neurosurgical Cases Ramsis F
www.surgicalneurologyint.com Surgical Neurology International Editor-in-Chief: Nancy E. Epstein, MD, Clinical Professor of Neurological Surgery, School of Medicine, State U. of NY at Stony Brook. SNI: Neuroanesthesia and Critical Care Editor Ramsis Ghaly, MD Haly Neurosurgical Associates, Aurora, Illinois, USA Open Access Editorial A novel checklist for anesthesia in neurosurgical cases Ramsis F. Ghaly, Mikhail Kushnarev, Iulia Pirvulescu, Zinaida Perciuleac, Kenneth D. Candido, Nebojsa Nick Knezevic Department of Anesthesiology, Advocate Illinois Masonic Medical Center, Chicago, Illinois, United States. E-mail: *Ramsis F. Ghaly - [email protected], Mikhail Kushnarev - [email protected], Iulia Pirvulescu - [email protected], Zinaida Perciuleac - [email protected], Kenneth D. Candido - [email protected], Nebojsa Nick Knezevic - [email protected] ABSTRACT roughout their training, anesthesiology residents are exposed to a variety of surgical subspecialties, many of which have specific anesthetic considerations. According to the Accreditation Council for Graduate Medical Education requirements, each anesthesiology resident must provide anesthesia for at least twenty intracerebral cases. ere are several studies that demonstrate that checklists may reduce deficiencies in pre-induction room setup. We are introducing a novel checklist for neuroanesthesia, which we believe to be helpful for residents *Corresponding author: during their neuroanesthesiology rotations. Our checklist provides a quick and succinct review of neuroanesthetic Ramsis F. Ghaly, challenges prior to case setup by junior residents, covering noteworthy aspects of equipment setup, airway Ghaly Neurosurgical management, induction period, intraoperative concerns, and postoperative considerations. We recommend Associates,, 4260 Westbrook displaying this checklist on the operating room wall for quick reference. Dr., Suite 227, Aurora, Illinois, United States. -

A Comprehensive Guide Ram Roth Elizabeth A.M. Frost Clifford Gevirtz
The Role of Anesthesiology in Global Health A Comprehensive Guide Ram Roth Elizabeth A.M. Frost Cli ord Gevirtz Editors Carrie L.H. Atcheson Associate Editor 123 The Role of Anesthesiology in Global Health Ram Roth • Elizabeth A.M. Frost Clifford Gevirtz Editors Carrie L.H. Atcheson Associate Editor The Role of Anesthesiology in Global Health A Comprehensive Guide Editors Ram Roth Elizabeth A.M. Frost Department of Anesthesiology Department of Anesthesiology Icahn School of Medicine at Mount Sinai Icahn School of Medicine at Mount Sinai New York , NY , USA New York , NY , USA Clifford Gevirtz Department of Anesthesiology LSU Health Sciences Center New Orleans , LA , USA Associate Editor Carrie L.H. Atcheson Oregon Anesthesiology Group Department of Anesthesiology Adventist Medical Center Portland , OR , USA ISBN 978-3-319-09422-9 ISBN 978-3-319-09423-6 (eBook) DOI 10.1007/978-3-319-09423-6 Springer Cham Heidelberg New York Dordrecht London Library of Congress Control Number: 2014956567 © Springer International Publishing Switzerland 2015 This work is subject to copyright. All rights are reserved by the Publisher, whether the whole or part of the material is concerned, specifi cally the rights of translation, reprinting, reuse of illustrations, recitation, broadcasting, reproduction on microfi lms or in any other physical way, and transmission or information storage and retrieval, electronic adaptation, computer software, or by similar or dissimilar methodology now known or hereafter developed. Exempted from this legal reservation are brief excerpts in connection with reviews or scholarly analysis or material supplied specifi cally for the purpose of being entered and executed on a computer system, for exclusive use by the purchaser of the work. -

Perioperative Pain Management for the Chronic Pain Patient with Long-Term Opioid Use
1.5 ANCC Contact Hours Perioperative Pain Management for the Chronic Pain Patient With Long-Term Opioid Use Carina Jackman In the United States nearly one in four patients present- patterns of preoperative opioid use. Approximately one ing for surgery reports current opioid use. Many of these in four patients undergoing surgery in the study re- patients suffer from chronic pain disorders and opioid ported preoperative opioid use (23.1% of the 34,186-pa- tolerance or dependence. Opioid tolerance and preexisting tient study population). Opioid use was most common chronic pain disorders present unique challenges in regard in patients undergoing orthopaedic spinal surgery to postoperative pain management. These patients benefi t (65%). This was followed by neurosurgical spinal sur- geries (55.1%). Hydrocodone bitartrate was the most from providers who are not only familiar with multimodal prevalent medication. Tramadol and oxycodone hydro- pain management and skilled in the assessment of acute pain, chloride were also common ( Hilliard et al., 2018 ). but also empathetic to their specifi c struggles. Chronic pain Given this signifi cant population of surgical patients patients often face stigmas surrounding their opioid use, with established opioid use, it is imperative for both and this may lead to underestimation and undertreatment nurses and all other providers to gain an understanding of their pain. This article aims to review the challenges of the complex challenges chronic pain patients intro- presented by these complex patients and provide strate- duce to the postoperative setting. gies for treating acute postoperative pain in opioid-tolerant patients. Defi nitions Common pain terminology as defined by the Chronic Pain and Long-Term International Association for the Study of Pain, a joint Opioid Use consensus statement by the American Society of Addiction Medicine, the American Academy of Pain The burden of chronic pain in the United States is stag- Medicine and the American Pain Society (2001 ), and the gering. -

Anaesthesia Associate
Published on Health Careers (https://www.healthcareers.nhs.uk) Home > Explore roles > Medical associate professions (MAPs) > Roles in the medical associate professions > Anaesthesia associate Anaesthesia associate Anaesthesia associates (previously known as physicians’ assistants (anaesthesia)) are part of the multi-disciplinary anaesthesia team, led by a consultant anaesthetist [1], that looks after patients undergoing many aspects of critical care. You’ll be trained to provide anaesthetic services, under supervision, in a variety of environments. As an anaesthesia associate, you’ll provide anaesthetic services to patients requiring anaesthesia, respiratory [2] care, cardiopulmonary resuscitation and/or other emergency, life sustaining services within the anaesthesia and wider theatre and critical care environments. You will deputise for anaesthetists in a variety of situations Although they have very similar names, the role of the anaesthesia associate and the physician associate [3] are very different. Working life As an anaesthesia associate, your work will be closely supervised by a consultant anaesthetist and there will be clear boundaries about what you can and cannot do. Typically, the range of duties will include: preoperative interviewing and physiological and psychological assessment of patients collecting patient information from the patients, taking a history, physical examination, laboratory, radiographic and other diagnostic data and identifying relevant problems implementing the anaesthesia care plan administering and/or -

Menu of Pain Management Clinic Regulation
Menu of Pain Management Clinic Regulation The United States is in the midst of an unprecedented epidemic of prescription drug overdose deaths.1 More than 38,000 people died of drug overdoses in 2010, and most of these deaths (22,134) were caused by overdoses involving prescription drugs.2 Three-quarters of prescription drug overdose deaths in 2010 (16,651) involved a prescription opioid pain reliever (OPR), which is a drug derived from the opium poppy or synthetic versions of it such as oxycodone, hydrocodone, or methadone.3 The prescription drug overdose epidemic has not affected all states equally, and overdose death rates vary widely between states. States have the primary responsibility to regulate and enforce prescription drug practice. Although state laws are commonly used to prevent injuries and their benefits have been demonstrated for a variety of injury types,4 there is little information on the effectiveness of state statutes and regulations designed to prevent prescription drug abuse and diversion. This menu is a first step in assessing pain management clinic laws by creating an inventory of state legal strategies in this domain. Introduction One type of law aimed at preventing inappropriate prescribing is regulation of pain management clinics, often called “pill mills” when they are sources of large quantities of prescriptions. Pill mills have become an increasing problem in the prescription drug epidemic, and laws have been enacted to prevent these facilities from prescribing controlled substances inappropriately. A law was included in this resource as a pain management clinic regulation if it requires state oversight and contains other requirements concerning ownership and operation of pain management clinics, facilities, or practice locations. -
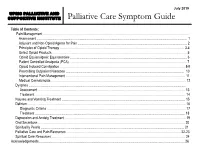
Palliative Care Symptom Guide
July 2019 UPMC PALLIATIVE AND SUPPORTIVE INSTITUTE Palliative Care Symptom Guide Table of Contents: Pain Management ……………………………………………………………………………………………………………………….. Assessment …………………………………………………………………………………………………………………………… 1 Adjuvant and Non-Opioid Agents for Pain ……………………………………………………………………………………….... 2 Principles of Opioid Therapy ……………………………………………………………………………………………….….…. 3-4 Select Opioid Products ……………………………………………………………………………………………………………… 5 Opioid Equianalgesic Equivalencies ………………………………………………………………………...…………………..… 6 Patient Controlled Analgesia (PCA) ……………………………………………………………………………………………….. 7 Opioid Induced Constipation ……………………………………………………………………………………………………… 8-9 Prescribing Outpatient Naloxone ………………………………………………………………………………………………… 10 Interventional Pain Management …………………………………………………………………………………………………. 11 Medical Cannabinoids ……………………………………………………………………………………………………………… 12 Dyspnea ………………………………………………………………………………………………………………………………… Assessment ………………………………………………………………………………………………………………………… 13 Treatment …………………………………………………………………………………………………………………………… 14 Nausea and Vomiting Treatment ……………………………………………………………………………………………..……… 15 Delirium …………………………………………………………………………………………………………………………………. 16 Diagnostic Criteria ……………………………………………………………………………….……………………….………... 17 Treatment ………………………………………………………………………………..…………………………………………. 18 Depression and Anxiety Treatment ……………………………………………………..…………..…………………………….…. 19 Oral Secretions ……………………………………………………..…………………………………………………………………. 20 Spirituality Pearls ……………………………………………………..………………………………………………………………. 21 Palliative -

Neurosurgical Anesthesia Does the Choice of Anesthetic Agents Matter?
medigraphic Artemisaen línea E A NO D NEST A ES Mexicana de IC IO EX L M O G O I ÍA G A E L . C C O . C Revista A N A T Í E Anestesiología S G S O O L C IO I S ED TE A ES D M AN EXICANA DE CONFERENCIAS MAGISTRALES Vol. 30. Supl. 1, Abril-Junio 2007 pp S126-S132 Neurosurgical anesthesia Does the choice of anesthetic agents matter? Piyush Patel, MD, FRCPC* * Professor of Anesthesiology. Department of Anesthesiology University of California, San Diego. Staff Anesthesiologist VA Medical Center San Diego INTRODUCTION 1) Moderate to severe intracranial hypertension 2) Inadequate brain relaxation during surgery The anesthetic management of neurosurgical patients is, by 3) Evoked potential monitoring necessity, based upon our understanding of the physiology 4) Intraoperative electrocorticography and pathophysiology of the central nervous system (CNS) 5) Cerebral protection and the effect of anesthetic agents on the CNS. Consequent- ly, a great deal of investigative effort has been expended to CNS EFFECTS OF ANESTHETIC AGENTS elucidate the influence of anesthetics on CNS physiology and pathophysiology. The current practice of neuroanes- It is now generally accepted that N2O is a cerebral vasodila- thesia is based upon findings of these investigations. How- tor and can increase CBF when administered alone. This ever, it should be noted that most studies in this field have vasodilation can result in an increase in ICP. In addition, been conducted in laboratory animals and the applicability N2O can also increase CMR to a small extent. The simulta- of the findings to the human patient is debatable at best.