New EU Criteria for Endocrine Disrupters Consequences for the Food Chain
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Evaluation of Tebuconazole, Triclosan, Methylparaben and Ethylparaben According to the Danish Proposal for Criteria for Endocrine Disrupters
Downloaded from orbit.dtu.dk on: Sep 26, 2021 Evaluation of tebuconazole, triclosan, methylparaben and ethylparaben according to the Danish proposal for criteria for endocrine disrupters Hass, Ulla; Christiansen, Sofie; Petersen, Marta Axelstad; Boberg, Julie; Andersson, Anna-Maria ; Skakkebæk, Niels Erik ; Bay, Katrine ; Holbech, Henrik ; Lund Kinnberg, Karin ; Bjerregaard, Poul Publication date: 2012 Document Version Publisher's PDF, also known as Version of record Link back to DTU Orbit Citation (APA): Hass, U., Christiansen, S., Petersen, M. A., Boberg, J., Andersson, A-M., Skakkebæk, N. E., Bay, K., Holbech, H., Lund Kinnberg, K., & Bjerregaard, P. (2012). Evaluation of tebuconazole, triclosan, methylparaben and ethylparaben according to the Danish proposal for criteria for endocrine disrupters. Danish Centre on Endocrine Disrupters. General rights Copyright and moral rights for the publications made accessible in the public portal are retained by the authors and/or other copyright owners and it is a condition of accessing publications that users recognise and abide by the legal requirements associated with these rights. Users may download and print one copy of any publication from the public portal for the purpose of private study or research. You may not further distribute the material or use it for any profit-making activity or commercial gain You may freely distribute the URL identifying the publication in the public portal If you believe that this document breaches copyright please contact us providing details, and we will -
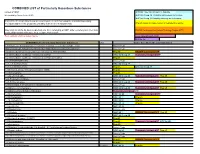
COMBINED LIST of Particularly Hazardous Substances
COMBINED LIST of Particularly Hazardous Substances revised 2/4/2021 IARC list 1 are Carcinogenic to humans list compiled by Hector Acuna, UCSB IARC list Group 2A Probably carcinogenic to humans IARC list Group 2B Possibly carcinogenic to humans If any of the chemicals listed below are used in your research then complete a Standard Operating Procedure (SOP) for the product as described in the Chemical Hygiene Plan. Prop 65 known to cause cancer or reproductive toxicity Material(s) not on the list does not preclude one from completing an SOP. Other extremely toxic chemicals KNOWN Carcinogens from National Toxicology Program (NTP) or other high hazards will require the development of an SOP. Red= added in 2020 or status change Reasonably Anticipated NTP EPA Haz list COMBINED LIST of Particularly Hazardous Substances CAS Source from where the material is listed. 6,9-Methano-2,4,3-benzodioxathiepin, 6,7,8,9,10,10- hexachloro-1,5,5a,6,9,9a-hexahydro-, 3-oxide Acutely Toxic Methanimidamide, N,N-dimethyl-N'-[2-methyl-4-[[(methylamino)carbonyl]oxy]phenyl]- Acutely Toxic 1-(2-Chloroethyl)-3-(4-methylcyclohexyl)-1-nitrosourea (Methyl-CCNU) Prop 65 KNOWN Carcinogens NTP 1-(2-Chloroethyl)-3-cyclohexyl-1-nitrosourea (CCNU) IARC list Group 2A Reasonably Anticipated NTP 1-(2-Chloroethyl)-3-cyclohexyl-1-nitrosourea (CCNU) (Lomustine) Prop 65 1-(o-Chlorophenyl)thiourea Acutely Toxic 1,1,1,2-Tetrachloroethane IARC list Group 2B 1,1,2,2-Tetrachloroethane Prop 65 IARC list Group 2B 1,1-Dichloro-2,2-bis(p -chloropheny)ethylene (DDE) Prop 65 1,1-Dichloroethane -

The Obesogen Hypothesis: Current Status and Implications for Human Health
Curr Envir Health Rpt (2014) 1:333–340 DOI 10.1007/s40572-014-0026-8 MECHANISMS OF TOXICITY (CJ MATTINGLY, SECTION EDITOR) The Obesogen Hypothesis: Current Status and Implications for Human Health Jerrold J. Heindel & Thaddeus T. Schug Published online: 20 September 2014 # Springer International Publishing AG (outside the USA) 2014 Abstract Obesity and diabetes have overtaken smoking as agreed upon that this obesity epidemic is the product of poor the number 1 preventable health determinate in the United nutrition and lack of exercise. However, obesity is a complex States. In its basic form, obesity is due to disruptions of the endocrine disease caused by disruption of many control sys- endocrine systems that control food intake, satiety, and meta- tems involving interaction between genetic and environmental bolic rate. Recent studies have identified a subclass of endo- cues such as nutrition, exercise, drugs, behavior, alterations in crine disrupting chemicals that interfere with hormonally reg- the microbiome, and exposure to environmental chemicals. ulated metabolic processes, especially during early develop- Genome wide association studies using large populations ment. These chemicals, called “obesogens,” may predispose have uncovered some 40 novel single nucleotide polymor- individuals to gain weight despite efforts to limit caloric intake phisms that are associated with increased body mass index and increase physical activity. Evidence suggests that chemi- (BMI), but together these genetic identifiers account for less cal exposures early in life can predispose individuals to weight than 5 % of the incidence of obesity [2]. Indeed, there are no gain through programming changes, which may enhance dys- known genetic mechanisms that can explain the remarkable functional eating behaviors later in life. -

Ethnicity, Confession and Intercultural Dialogue at the European Union's
Munich Personal RePEc Archive Ethnicity, Confession and Intercultural Dialogue at the European Union’s East Border Brie, Mircea and Horga, Ioan and Şipoş, Sorin University of Oradea, Romania 2011 Online at https://mpra.ub.uni-muenchen.de/44082/ MPRA Paper No. 44082, posted 31 Jan 2013 05:28 UTC ETHNICITY, CONFESSION AND INTERCULTURAL DIALOGUE AT THE EUROPEAN UNION EASTERN BORDER ETHNICITY, CONFESSION AND INTERCULTURAL DIALOGUE AT THE EUROPEAN UNION EASTERN BORDER Mircea BRIE Ioan HORGA Sorin ŞIPOŞ (Coordinators) Debrecen/Oradea 2011 This present volume contains the papers of the international conference Ethnicity, Confession and Intercultural Dialogue at the European Union‟s East Border, held in Oradea between 2nd-5th of June 2011, organized by Institute for Euroregional Studies Oradea-Debrecen, University of Oradea and Department of International Relations and European Studies, with the support of the European Commission and Bihor County Council. CONTENTS INTRODUCTORY STUDIES Mircea BRIE Ethnicity, Religion and Intercultural Dialogue in the European Border Space.......11 Ioan HORGA Ethnicity, Religion and Intercultural Education in the Curricula of European Studies .......19 MINORITY AND MAJORITY IN THE EASTERN EUROPEAN AREA Victoria BEVZIUC Electoral Systems and Minorities Representations in the Eastern European Area........31 Sergiu CORNEA, Valentina CORNEA Administrative Tools in the Protection and Promotion of the Rights of Ethnic Minorities .............................................................................................................47 -

March 2007 Master Name Index List * Number in Front of Each
March 2007 Master Name Index List 2 Caas, 1 Cadenhead,Jim 3 Cady,Charlotte 1 Caas,Catherine 2 Cadieux, 1 Cady,Cornelius S. 2 Caas,Frank 1 Cadle, 1 Cady,Eliza L.(Everetts) 2 Caas,John 1 Cadle,Sarah 1 Cady,Frank W. 2 Caas,John F. 1 Cadogan,Catherine 1 Cady,Fred 1 Caas,John N. 1 Cadogan,Lavina(Bradshaw) 1 Cady,G.C. 1 Caas,N. 1 Cadogan,Nellie 1 Cady,H.N. 1 Caas,Nic 1 Cadogan,Walter 1 Cady,H.Olin 1 Caas,Nic. 1 Cadwallader, 1 Cady,Harriett(Bishop) 9 Caas,Nicholas 1 Cadwallader,John 1 Cady,Hattie(Yates) 1 Caas,Susie 1 Cadwallader,Mary A.(Collins) 1 Cady,Helen L.(Howard) 1 Caas,Theresa(Wolf) 1 Cadwallader,Morris 1 Cady,Louis 1 Caas,Vic 1 Cadwalter, 1 Cady,Louis N. 1 Caballero,Hector M. 1 Cadwalter,Dennis 1 Cady,M.E. 1 Cabel, 2 Cadwell, 3 Cady,Martin E. 3 Cable, 1 Cadwell,Addie M. 1 Cady,Mary L. 1 Cable,Betsey K. 1 Cadwell,B. 4 Cady,Nancy 1 Cable,C. 1 Cadwell,Badish 1 Cady,Oliver 2 Cable,Cornelia 2 Cadwell,Bradish 2 Cady,Palmer 1 Cable,F.S. 1 Cadwell,C. 1 Cady,Ruby M. 2 Cable,H.B. 1 Cadwell,Clara 1 Cady,Sarah M. 1 Cable,M.A. 5 Cadwell,Cordelia 1 Cady,Willia1m 1 Cable,M.C. 1 Cadwell,E. 1 Cady,William 2 Cable,M.H. 5 Cadwell,Edgar 4 Cady,Wm. 2 Cable,Marvin H. 1 Cadwell,Ernest 1 Cady,Wm.W. 1 Cable,Stella M. -

Endosulfan and Endocrine Disruption: Human Risk Characterization
ENDOSULFAN AND ENDOCRINE DISRUPTION: HUMAN RISK CHARACTERIZATION Prepared by Laura M. Plunkett, Ph.D., DABT Integrative Biostrategies, LLC Houston, Texas Prepared for Makhteshim-Agan of North America, Inc. Raleigh, North Carolina June 23, 2008 1 I. Overview of Endocrine Disruption as an Endpoint of Concern in Pesticide Risk Assessment The endocrine system is one of the basic systems in mammalian physiology that is involved in variety of body functions including such functions as growth, development, reproduction, and behavior. The activity of the endocrine system involves endocrine glands which are collections of specialized cells in various tissues of the body that synthesize, store and release substances into the bloodstream. These substances are known as hormones. Hormones act as chemical messengers, traveling through the bloodstream to distant organs and tissues where they can bind to receptors located on those tissues and organs and as a result of receptor binding trigger a physiological response. The major endocrine glands include the pituitary gland, the thyroid gland, the pancreas, the adrenal gland, the testes, and the ovary. “Endocrine disruption”1 is a term that has arisen in human health risk assessment and is defined as the action of an external agent, such as a chemical, to interfere with normal activity of circulating hormones. This “interference” would include altering the synthesis, storage, release, or degradation of hormones, as well as actions at hormone receptors such as stimulating receptor activity (receptor agonist activity) or inhibiting receptor activity (receptor antagonist activity). The potential effects of chemicals, including pesticides, as endocrine disruptors have been a focus of recent regulatory actions. -
Toxicological Profile for Bisphenol A
TT TOXICOLOGICAL PROFILE FOR BISPHENOL A September 2009 Integrated Risk Assessment Branch Office of Environmental Health Hazard Assessment California Environmental Protection Agency Toxicological Profile for Bisphenol A September 2009 Prepared by Office of Environmental Health Hazard Assessment Prepared for Ocean Protection Council Under an Interagency Agreement, Number 07-055, with the State Coastal Conservancy LIST OF CONTRIBUTORS Authors Jim Carlisle, D.V.M., Ph.D., Senior Toxicologist, Integrated Risk Assessment Branch Dave Chan, D. Env., Staff Toxicologist, Integrated Risk Assessment Branch Mari Golub, Ph.D., Staff Toxicologist, Reproductive and Cancer Hazard Assessment Branch Sarah Henkel, Ph.D., California Sea Grant Fellow, California Ocean Science Trust Page Painter, M.D., Ph.D., Senior Toxicologist, Integrated Risk Assessment Branch K. Lily Wu, Ph.D., Associate Toxicologist, Reproductive and Cancer Hazard Assessment Branch Reviewers David Siegel, Ph.D., Chief, Integrated Risk Assessment Branch i Table of Contents Executive Summary ................................................................................................................................ iv Use and Exposure ............................................................................................................................... iv Environmental Occurrence ................................................................................................................. iv Effects on Aquatic Life ...................................................................................................................... -

Indoor Dust Poses Significant Endocrine Disruptor Risk
9 October 2008 Indoor dust poses significant endocrine disruptor risk The risks from exposure to outdoor pollution or sources like tobacco smoke are well known, but indoor dust can also pose health risks, especially to young children. New evidence shows that indoor dust is highly contaminated by persistent and endocrine-disrupting chemicals, including some chemicals such as polychlorinated biphenyls (PCBs) which have been banned since the 1970s. Endocrine disruptors are substances which disrupt the body’s natural hormonal system. Some endocrine- disrupting chemicals can persist for many years. These include PCBs, polybrominated diphenyl ethers (PBDEs), pyrethroids, dichlorodiphenyltrichloroethane (DDT), chlorodanes and phthalates. These chemicals and others are found in indoor dust, which can be eaten or breathed in. Endocrine disrupters may be responsible for declining sperm counts, genital malformations, cancers and impaired neural development and sexual behaviour. Dust collected from vacuum cleaners used in apartments and a community hall was highly contaminated with endocrine disruptors, in particular phthalates and PBDEs. The levels of PCBs were high enough in some cases to be a health concern, illustrating that these chemicals continue to persist in the environment and pose risks. Although the use of some PBDEs is being phased out in some parts of the US and they have been banned in EU Member States since 2004, this trend may apply to PBDEs as well. PBDEs are flame retardants used on soft furnishings, and so as long as items such as mattresses, carpets and sofas treated with the chemical are used then exposure will continue. Because young children spend a lot of time indoors, often at floor level, and put objects in their mouths, they are particularly at risk from pollutants in indoor dust. -

Estrogen-Like Effect of Mitotane Explained by Its Agonist Activity on Estrogen Receptor-Α
biomedicines Article Estrogen-Like Effect of Mitotane Explained by Its Agonist Activity on Estrogen Receptor-α Elisa Rossini 1,†, Edoardo Giacopuzzi 2,3,† , Fabrizio Gangemi 4,† , Mariangela Tamburello 1, Deborah Cosentini 5, Andrea Abate 1, Marta Laganà 5, Alfredo Berruti 5 , Salvatore Grisanti 5,‡ and Sandra Sigala 1,*,‡ 1 Section of Pharmacology, Department of Molecular and Translational Medicine, University of Brescia, 25123 Brescia, Italy; [email protected] (E.R.); [email protected] (M.T.); [email protected] (A.A.) 2 Wellcome Centre for Human Genetics, University of Oxford, Oxford OX3 7BN, UK; [email protected] 3 National Institute for Health Research Oxford Biomedical Research Centre, Oxford OX4 2PG, UK 4 Unit of Physics, Department of Molecular and Translational Medicine, University of Brescia, 25123 Brescia, Italy; [email protected] 5 Medical Oncology Unit, Department of Medical and Surgical Specialties, Radiological Sciences, and Public Health, University of Brescia at A.S.S.T. Spedali Civili di Brescia, 25123 Brescia, Italy; [email protected] (D.C.); [email protected] (M.L.); [email protected] (A.B.); [email protected] (S.G.) * Correspondence: [email protected] † These Authors equally contributed to this paper. ‡ These authors are co-senior authors of this paper. Citation: Rossini, E.; Giacopuzzi, E.; Abstract: Mitotane is the cornerstone of medical treatment of adrenocortical carcinoma. Estrogenic- Gangemi, F.; Tamburello, M.; like side effects frequently occur in patients, and previous studies explored the chemical nature Cosentini, D.; Abate, A.; Laganà, M.; of the interaction between estrogen receptor-α (ER-α) and toxic compounds, including the DDD Berruti, A.; Grisanti, S.; Sigala, S. -

ROCZNIKI PAŃSTWOWEGO ZAKŁADU HIGIENY - 2019, Vol
ROCZNIKI PAŃSTWOWEGO ZAKŁADU HIGIENY ISSN 0035-7715 [ANNALS OF THE NATIONAL INSTITUTE OF HYGIENE] eISSN 2451-2311 Volume 70 2019 Number 3 Nutrition of vegetarians in Poland – a review of research. Paulina Skorek, Paweł Glibowski, Katarzyna Banach ..................................................................................................... 217 Mobile telephony and its effects on human health. ROCZNIKI Andrzej Magiera, Jolanta Solecka .................................................................................................................................... 225 Role of nutritional support provided by qualified dietitians in the prevention and treatment of non-communicable diseases. Barbara Bednarczuk, Anna Czekajło-Kozłowska ............................................................................................................. 235 PAŃSTWOWEGO Body composition and nutrition of female athletes. Karol Pilis, Krzysztof Stec, Anna Pilis, Agata Mroczek, Cezary Michalski, Wiesław Pilis .............................................. 243 ZAKŁADU HIGIENY Lower weight gain after vaping cessation than after smoking quitting. Ewelina Wawryk-Gawda, Michał K. Zarobkiewicz, Patrycja Chylińska-Wrzos, Barbara Jodłowska-Jędrych ............... 253 Assessment of selected food intake frequency in patients with type 1 diabetes treated with personal insulin pumps. Sabina Krzyżowska, Bartłomiej Matejko, Beata Kieć-Wilk, Magdalena Wilk, Maciej Małecki, Tomasz Klupa .............. 259 Obesity diagnosis and mortality risk based on a body shape -

HPD V2.2 Created Via HPDC Builder Page 1 of 17 VOLATILE ORGANIC COMPOUND (VOC) CONTENT CERTIFICATIONS and COMPLIANCE See Section 3 for Additional Listings
M2.1 Health Product by Humanscale Declaration v2.2 created via: HPDC Online Builder HPD UNIQUE IDENTIFIER: 21096 CLASSIFICATION: 12 51 00.00 Furnishings: Office Furniture PRODUCT DESCRIPTION: In today’s fast-paced, agile work environment, there’s no time for discomfort. M2.1, part of Humanscale’s revolutionary new monitor arm line, instantly improves the comfort, health and productivity of any workspace. Fully compatible with traditional desks and sit/stand workstations alike, M2.1 meets a variety of configuration needs for lighter monitors up to 15.5 lbs. Featuring innovations like Humanscale’s patented Weight-Compensating Spring Technology and Smart Stop functionality, M2.1 enables the personalization and flexibility needed for today’s evolving workplaces. Section 1: Summary Nested Method / Product Threshold CONTENT INVENTORY Inventory Reporting Format Threshold level Residuals/Impurities All Substances Above the Threshold Indicated Are: Nested Materials Method 100 ppm Residuals/Impurities Characterized Yes Ex/SC Yes No Basic Method 1,000 ppm Considered in 6 of 13 Materials % weight and role provided for all substances. Per GHS SDS Explanation(s) provided Threshold Disclosed Per Other for Residuals/Impurities? Screened Yes Ex/SC Yes No Material Yes No All substances screened using Priority Hazard Lists with Product results disclosed. Identified Yes Ex/SC Yes No One or more substances not disclosed by Name (Specific or Generic) and Identifier and/ or one or more Special Condition did not follow guidance. CONTENT IN DESCENDING ORDER OF QUANTITY Number of Greenscreen BM-4/BM3 contents ... 0 Summary of product contents and results from screening individual chemical Contents highest concern GreenScreen substances against HPD Priority Hazard Lists and the GreenScreen for Safer Benchmark or List translator Score .. -

Microbiota and Obesogens: Environmental Regulators of Fat Storage
Microbiota and obesogens: environmental regulators of fat storage John F. Rawls, Ph.D. Department of Molecular Genetics & Microbiology Center for Genomics of Microbial Systems Duke University School of Medicine Seminar outline 1. Introduction to the microbiota 2. Microbiota as environmental factors in obesity 3. Obesogens as environmental factors in obesity Seeing and understanding the unseen Antonie van Leewenhoek 1620’s: Described differences between microbes associated with teeth & feces during health & disease. Louis Pasteur 1850’s: Helps establish the “germ theory” of disease. 1885: Predicts that germ-free animals can not survive without “common microorganisms”. Culture-independent analysis of bacterial communities using 16S rRNA gene sequencing 16S rRNA 16S SSU rRNA 16S rRNA gene V1 V2 V3 V4 V5 V6 V7 V8 V9 Culture-independent analysis of bacterial communities using 16S rRNA gene sequencing plantbiology.siu.edu Phylogenetic analysis of 16S rRNA genes revealed 3 domains and a vast unappreciated diversity of microbial life You are here Carl Woese Glossary • Microbiota / microflora: the microorganisms of a particular site, habitat, or period of time. • Microbiome: the collective genomes of the microorganisms within a microbiota. • Germ-free / axenic: of a culture that is free from living organisms other than the host species. • Gnotobiotic: of an environment for rearing organisms in which all the microorganisms are either excluded or known. Current techniques for microbiome profiling Microbial community Morgan et al. (2012) Trends in