Exogenous 3‐Iodothyronamine Rescues the Entorhinal Cortex from Β‐Amyloid
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Is TAAR1 a Potential Therapeutic Target for Immune Dysregulation In
Graduate Physical and Life Sciences PhD Pharmacology Abstract ID# 1081 Is TAAR1 a Potential Therapeutic Target for Immune Dysregulation in Drug Abuse? Fleischer, Lisa M; Tamashunas, Nina and Miller, Gregory M Addiction Sciences Laboratory, Northeastern University, Boston MA 02115 Abstract Discovered in 2001, Trace Amine Associated Receptor 1 (TAAR1) is a direct target of Data and Results amphetamine, methamphetamine and MDMA. It is expressed in the brain reward circuity and modulates dopamine transporter function and dopamine neuron firing rates. Newly-developed compounds that specifically target TAAR1 have recently been investigated in animal models In addition to brain, TAAR1 is expressed in immune cells METH promotes PKA and PKC Phosphorylation through TAAR1 as candidate therapeutics for methamphetamine, cocaine and alcohol abuse. These studies • We treated HEK/TAAR1 cells and HEK293 involving classic behavioral measures of drug response, as well as drug self-administration, Rhesus and Human cells with vehicle or METH, with and without strongly implicate TAAR1 as a potential therapeutic target for the treatment of addiction. In activators and inhibitors of PKA and PKC. addition to its central actions, we demonstrated that TAAR1 is upregulated in peripheral blood Cells Lines mononuclear cells (PBMC) and B cells following immune activation, and that subsequent • We performed Western blotting experiments to activation of TAAR1 by methamphetamine stimulates cAMP, similar to the function of measure levels of phospho-PKA and phospho- adenosine A2 receptors which are also present in immune cells and play a critical role in the PKC. immune response. Here, we are investigating the relationship between TAAR1 and the • We found that specific activators of PKA and adenosine A2 receptor at the level of cellular signaling and receptor dimerization. -
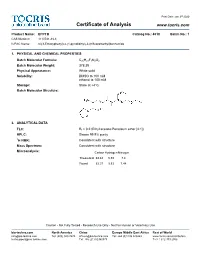
Certificate of Analysis
Print Date: Jan 3rd 2020 Certificate of Analysis www.tocris.com Product Name: EPPTB Catalog No.: 4518 Batch No.: 1 CAS Number: 1110781-88-8 IUPAC Name: N-(3-Ethoxyphenyl)-4-(1-pyrrolidinyl)-3-(trifluoromethyl)benzamide 1. PHYSICAL AND CHEMICAL PROPERTIES Batch Molecular Formula: C20H21F3N2O2 Batch Molecular Weight: 378.39 Physical Appearance: White solid Solubility: DMSO to 100 mM ethanol to 100 mM Storage: Store at +4°C Batch Molecular Structure: 2. ANALYTICAL DATA TLC: Rf = 0.2 (Ethyl acetate:Petroleum ether [4:1]) HPLC: Shows 99.9% purity 1H NMR: Consistent with structure Mass Spectrum: Consistent with structure Microanalysis: Carbon Hydrogen Nitrogen Theoretical 63.48 5.59 7.4 Found 63.37 5.53 7.44 Caution - Not Fully Tested • Research Use Only • Not For Human or Veterinary Use bio-techne.com North America China Europe Middle East Africa Rest of World [email protected] Tel: (800) 343 7475 [email protected] Tel: +44 (0)1235 529449 www.tocris.com/distributors [email protected] Tel: +86 (21) 52380373 Tel:+1 612 379 2956 Print Date: Jan 3rd 2020 Product Information www.tocris.com Product Name: EPPTB Catalog No.: 4518 Batch No.: 1 CAS Number: 1110781-88-8 IUPAC Name: N-(3-Ethoxyphenyl)-4-(1-pyrrolidinyl)-3-(trifluoromethyl)benzamide Description: Storage: Store at +4°C Trace amine 1 (TA ) receptor antagonist/inverse agonist; 1 Solubility & Usage Info: exhibits a higher potency at the mouse TA1 receptor than the rat DMSO to 100 mM and human TA150 receptors (IC values are 27.5, 4539 and 7487 ethanol to 100 mM nM, respectively). -

Modulation by Trace Amine-Associated Receptor 1 of Experimental Parkinsonism, L-DOPA Responsivity, and Glutamatergic Neurotransmission
The Journal of Neuroscience, October 14, 2015 • 35(41):14057–14069 • 14057 Neurobiology of Disease Modulation by Trace Amine-Associated Receptor 1 of Experimental Parkinsonism, L-DOPA Responsivity, and Glutamatergic Neurotransmission Alexandra Alvarsson,1* Xiaoqun Zhang,1* Tiberiu L Stan,1 Nicoletta Schintu,1 Banafsheh Kadkhodaei,2 Mark J. Millan,3 Thomas Perlmann,2,4 and Per Svenningsson1 1Department of Clinical Neuroscience, Center for Molecular Medicine, Karolinska Institutet, SE-17176 Stockholm, Sweden, 2Ludwig Institute for Cancer Research, SE-17177 Stockholm, Sweden, 3Pole of Innovation in Neuropsychiatry, Institut de Recherches Servier, Centre de Recherches de Croissy, Paris 87290, France, and 4Department of Cell and Molecular Biology, Karolinska Institutet, SE-17177 Stockholm, Sweden Parkinson’s disease (PD) is a movement disorder characterized by a progressive loss of nigrostriatal dopaminergic neurons. Restoration of dopamine transmission by L-DOPA relieves symptoms of PD but causes dyskinesia. Trace Amine-Associated Receptor 1 (TAAR1) modulates dopaminergic transmission, but its role in experimental Parkinsonism and L-DOPA responses has been neglected. Here, we report that TAAR1 knock-out (KO) mice show a reduced loss of dopaminergic markers in response to intrastriatal 6-OHDA administra- tion compared with wild-type (WT) littermates. In contrast, the TAAR1 agonist RO5166017 aggravated degeneration induced by intra- striatal6-OHDAinWTmice.Subchronic L-DOPAtreatmentofTAAR1KOmiceunilaterallylesionedwith6-OHDAinthemedialforebrain bundle resulted in more pronounced rotational behavior and dyskinesia than in their WT counterparts. The enhanced behavioral sensitization to L-DOPA in TAAR1 KO mice was paralleled by increased phosphorylation of striatal GluA1 subunits of AMPA receptors. Conversely, RO5166017 counteracted both L-DOPA-induced rotation and dyskinesia as well as AMPA receptor phosphorylation. -

G Protein-Coupled Receptors
S.P.H. Alexander et al. The Concise Guide to PHARMACOLOGY 2015/16: G protein-coupled receptors. British Journal of Pharmacology (2015) 172, 5744–5869 THE CONCISE GUIDE TO PHARMACOLOGY 2015/16: G protein-coupled receptors Stephen PH Alexander1, Anthony P Davenport2, Eamonn Kelly3, Neil Marrion3, John A Peters4, Helen E Benson5, Elena Faccenda5, Adam J Pawson5, Joanna L Sharman5, Christopher Southan5, Jamie A Davies5 and CGTP Collaborators 1School of Biomedical Sciences, University of Nottingham Medical School, Nottingham, NG7 2UH, UK, 2Clinical Pharmacology Unit, University of Cambridge, Cambridge, CB2 0QQ, UK, 3School of Physiology and Pharmacology, University of Bristol, Bristol, BS8 1TD, UK, 4Neuroscience Division, Medical Education Institute, Ninewells Hospital and Medical School, University of Dundee, Dundee, DD1 9SY, UK, 5Centre for Integrative Physiology, University of Edinburgh, Edinburgh, EH8 9XD, UK Abstract The Concise Guide to PHARMACOLOGY 2015/16 provides concise overviews of the key properties of over 1750 human drug targets with their pharmacology, plus links to an open access knowledgebase of drug targets and their ligands (www.guidetopharmacology.org), which provides more detailed views of target and ligand properties. The full contents can be found at http://onlinelibrary.wiley.com/doi/ 10.1111/bph.13348/full. G protein-coupled receptors are one of the eight major pharmacological targets into which the Guide is divided, with the others being: ligand-gated ion channels, voltage-gated ion channels, other ion channels, nuclear hormone receptors, catalytic receptors, enzymes and transporters. These are presented with nomenclature guidance and summary information on the best available pharmacological tools, alongside key references and suggestions for further reading. -

Update on 3-Iodothyronamine and Its Neurological and Metabolic Actions
REVIEW ARTICLE published: 16 October 2014 doi: 10.3389/fphys.2014.00402 Update on 3-iodothyronamine and its neurological and metabolic actions Riccardo Zucchi*, Alice Accorroni and Grazia Chiellini Laboratory of Biochemistry, Department of Pathology, University of Pisa, Pisa, Italy Edited by: 3-iodothyronamine (T1AM) is an endogenous amine, that has been detected in many Maria Moreno, University of Sannio, rodent tissues, and in human blood. It has been hypothesized to derive from thyroid Italy hormone metabolism, but this hypothesis still requires validation. T1AM is not a Reviewed by: ligand for nuclear thyroid hormone receptors, but stimulates with nanomolar affinity Anna M. D. Watson, Baker IDI Heart and Diabetes Institute, Australia trace amine-associated receptor 1 (TAAR1), a G protein-coupled membrane receptor. Carolin Stephanie Hoefig, Karolinska With a lower affinity it interacts with alpha2A adrenergic receptors. Additional targets Institutet, Sweden are represented by apolipoprotein B100, mitochondrial ATP synthase, and membrane *Correspondence: monoamine transporters, but the functional relevance of these interactions is still Riccardo Zucchi, Laboratory of uncertain. Among the effects reported after administration of exogenous T1AM to Biochemistry, Department of Pathology, University of Pisa, Via experimental animals, metabolic and neurological responses deserve special attention, Roma 55, 56126 Pisa, Italy because they were obtained at low dosages, which increased endogenous tissue e-mail: [email protected] concentration by about one order of magnitude. Systemic T1AM administration favored fatty acid over glucose catabolism, increased ketogenesis and increased blood glucose. Similar responses were elicited by intracerebral infusion, which inhibited insulin secretion and stimulated glucagon secretion. However, T1AM administration increased ketogenesis and gluconeogenesis also in hepatic cell lines and in perfused liver preparations, providing evidence for a peripheral action, as well. -

Receptor Interaction Profiles of 4-Alkoxy-Substituted 2,5-Dimethoxyphenethylamines and Related Amphetamines
ORIGINAL RESEARCH published: 28 November 2019 doi: 10.3389/fphar.2019.01423 Receptor Interaction Profiles of 4-Alkoxy-Substituted 2,5-Dimethoxyphenethylamines and Related Amphetamines Karolina E. Kolaczynska 1, Dino Luethi 1,2, Daniel Trachsel 3, Marius C. Hoener 4 and Matthias E. Liechti 1* 1 Division of Clinical Pharmacology and Toxicology, Department of Biomedicine, University Hospital Basel and University of Basel, Basel, Switzerland, 2 Center for Physiology and Pharmacology, Institute of Pharmacology, Medical University of Vienna, Vienna, Austria, 3 ReseaChem GmbH, Burgdorf, Switzerland, 4 Neuroscience Research, pRED, Roche Innovation Center Basel, F. Hoffmann-La Roche Ltd, Basel, Switzerland Background: 2,4,5-Trimethoxyamphetamine (TMA-2) is a potent psychedelic compound. Structurally related 4-alkyloxy-substituted 2,5-dimethoxyamphetamines and phenethylamine congeners (2C-O derivatives) have been described but their pharmacology Edited by: is mostly undefined. Therefore, we examined receptor binding and activation profiles of M. Foster Olive, these derivatives at monoamine receptors and transporters. Arizona State University, United States Methods: Receptor binding affinities were determined at the serotonergic 5-HT1A, 5-HT2A, Reviewed by: Luc Maroteaux, and 5-HT2C receptors, trace amine-associated receptor 1 (TAAR1), adrenergic α1 and INSERM U839 Institut du Fer à α2 receptors, dopaminergic D2 receptor, and at monoamine transporters, using target- Moulin, France Simon D. Brandt, transfected cells. Additionally, activation of 5-HT2A and 5-HT2B receptors and TAAR1 was Liverpool John Moores University, determined. Furthermore, we assessed monoamine transporter inhibition. United Kingdom Results: Both the phenethylamine and amphetamine derivatives (Ki = 8–1700 nM and *Correspondence: Matthias E. Liechti 61–4400 nM, respectively) bound with moderate to high affinities to the 5-HT2A receptor [email protected] with preference over the 5-HT1A and 5-HT2C receptors (5-HT2A/5-HT1A = 1.4–333 and Specialty section: 5-HT2A/5-HT2C = 2.1–14, respectively). -

4-Fluoroamphetamine (4-FA) Critical Review Report Agenda Item 4.3
4-Fluoroamphetamine (4-FA) Critical Review Report Agenda Item 4.3 Expert Committee on Drug Dependence Thirty-ninth Meeting Geneva, 6-10 November 2017 39th ECDD (2017) Agenda item 4.3 4-FA Contents Acknowledgements.................................................................................................................................. 4 Summary...................................................................................................................................................... 5 1. Substance identification ....................................................................................................................... 6 A. International Nonproprietary Name (INN).......................................................................................................... 6 B. Chemical Abstract Service (CAS) Registry Number .......................................................................................... 6 C. Other Chemical Names ................................................................................................................................................... 6 D. Trade Names ....................................................................................................................................................................... 6 E. Street Names ....................................................................................................................................................................... 6 F. Physical Appearance ...................................................................................................................................................... -
The Involvement of Trace Amine-Associated Receptor 1 and Thyroid Hormone Transporters in Non-Classical Pathways of the Thyroid Gland Auto-Regulation
The Involvement of Trace Amine-Associated Receptor 1 and Thyroid Hormone Transporters in Non-Classical Pathways of the Thyroid Gland Auto-Regulation by Maria Qatato a Thesis submitted in partial fulfillment of the requirements for the degree of Doctor of Philosophy in Cell Biology Approved Dissertation Committee Prof. Dr. Klaudia Brix Jacobs University Bremen Prof. Sebastian Springer, DPhil Jacobs University Bremen Dr. Georg Homuth Ernst-Moritz-Arndt-Universität Greifswald Date of Defence: 16 January 2018 Department of Life Sciences and Chemistry Statutory Declaration Family Name, Given/First Name Qatato, Maria Matriculation number 20330110 What kind of thesis are you submitting: PhD Thesis English: Declaration of Authorship I hereby declare that the thesis submitted was created and written solely by myself without any external support. Any sources, direct or indirect, are marked as such. I am aware of the fact that the contents of the thesis in digital form may be revised with regard to usage of unauthorized aid as well as whether the whole or parts of it may be identified as plagiarism. I do agree my work to be entered into a database for it to be compared with existing sources, where it will remain in order to enable further comparisons with future theses. This does not grant any rights of reproduction and usage, however. This document was neither presented to any other examination board nor has it been published. German: Erklärung der Autorenschaft (Urheberschaft) Ich erkläre hiermit, dass die vorliegende Arbeit ohne fremde Hilfe ausschließlich von mir erstellt und geschrieben worden ist. Jedwede verwendeten Quellen, direkter oder indirekter Art, sind als solche kenntlich gemacht worden. -

The Selective Antagonist EPPTB Reveals TAAR1-Mediated Regulatory Mechanisms in Dopaminergic Neurons of the Mesolimbic System
The selective antagonist EPPTB reveals TAAR1-mediated regulatory mechanisms in dopaminergic neurons of the mesolimbic system Amyaouch Bradaiaa,b, Gerhard Trubec, Henri Stalderc, Roger D. Norcrossc, Laurence Ozmenc, Joseph G. Wettsteinc, Audre´ e Pinarda, Danie` le Buchyc, Martin Gassmanna, Marius C. Hoenerc, and Bernhard Bettlera,1 aDepartment of Biomedicine, Institute of Physiology, Pharmazentrum, University of Basel, CH-4056 Basel, Switzerland; bNeuroservice, 13593 Aix en Provence, Cedex 03, France; and cPharmaceuticals Division, Neuroscience Research, F. Hoffmann-La Roche Ltd., CH-4070 Basel, Switzerland Edited by Shigetada Nakanishi, Osaka Bioscience Institute, Osaka, Japan, and approved September 29, 2009 (received for review June 11, 2009) Trace amine-associated receptor 1 (TAAR1) is a G protein-coupled receptor-mediated pathway. The genetic absence of TAAR1 receptor (GPCR) that is nonselectively activated by endogenous clearly increased the spontaneous firing rate of DA neurons but metabolites of amino acids. TAAR1 is considered a promising drug the underlying signaling mechanism remained unclear (7). Taar1 target for the treatment of psychiatric and neurodegenerative knockout mice also display behavioral and neurochemical signs disorders. However, no selective ligand to identify TAAR1-specific of DA supersensitivity, a feature thought to relate to positive signaling mechanisms is available yet. Here we report a selective symptoms of schizophrenia (8). In addition, TAs were implicated TAAR1 antagonist, EPPTB, and characterize its physiological effects in the etiology of depression, addiction, attention-deficit/ at dopamine (DA) neurons of the ventral tegmental area (VTA). We hyperactivity disorder, and Parkinson’s disease (5, 9, 10). How- show that EPPTB prevents the reduction of the firing frequency of ever, validation of therapeutic concepts was hampered by the DA neurons induced by p-tyramine (p-tyr), a nonselective TAAR1 lack of a ligand that specifically regulates TAAR1 activity in agonist. -

TAAR1 Modulates Cortical Glutamate NMDA Receptor Function
Neuropsychopharmacology (2015) 40, 2217–2227 © 2015 American College of Neuropsychopharmacology. All rights reserved 0893-133X/15 www.neuropsychopharmacology.org TAAR1 Modulates Cortical Glutamate NMDA Receptor Function Stefano Espinoza1, Gabriele Lignani1, Lucia Caffino2, Silvia Maggi1, Ilya Sukhanov1,3, Damiana Leo1, Liudmila Mus1, Marco Emanuele1, Giuseppe Ronzitti1, Anja Harmeier4, Lucian Medrihan1, 1,5 1 4 1 1 Tatyana D Sotnikova , Evelina Chieregatti , Marius C Hoener , Fabio Benfenati , Valter Tucci , 2 *,1,5,6 Fabio Fumagalli and Raul R Gainetdinov 1Department of Neuroscience and Brain Technologies, Istituto Italiano di Tecnologia, Genova, Italy; 2Dipartimento di Scienze Farmacologiche e 3 Biomolecolari, Università degli Studi di Milano, Milan, Italy; Department of Pharmacology, St Petersburg State Medical University, Petersburg, 4 Russia; Neuroscience, Ophthalmology and Rare Diseases Discovery and Translational Area, pRED, Roche Innovation Center Basel, F. Hoffmann- 5 La Roche Ltd, Basel, Switzerland; Institute of Translational Biomedicine, Faculty of Biology, St Petersburg State University, St Petersburg, Russia; 6 Skolkovo Institute of Science and Technology (Skoltech) Skolkovo, Moscow region, Russia Trace Amine-Associated Receptor 1 (TAAR1) is a G protein-coupled receptor expressed in the mammalian brain and known to influence subcortical monoaminergic transmission. Monoamines, such as dopamine, also play an important role within the prefrontal cortex (PFC) circuitry, which is critically involved in high-o5rder cognitive processes. TAAR1-selective ligands have shown potential antipsychotic, antidepressant, and pro-cognitive effects in experimental animal models; however, it remains unclear whether TAAR1 can affect PFC- related processes and functions. In this study, we document a distinct pattern of expression of TAAR1 in the PFC, as well as altered subunit composition and deficient functionality of the glutamate N-methyl-D-aspartate (NMDA) receptors in the pyramidal neurons of layer V of PFC in mice lacking TAAR1. -

SEP-363856, a Novel Psychotropic Agent with a Unique, Non-D2 Receptor Mechanism of Action S
Supplemental material to this article can be found at: http://jpet.aspetjournals.org/content/suppl/2019/08/01/jpet.119.260281.DC1 1521-0103/371/1/1–14$35.00 https://doi.org/10.1124/jpet.119.260281 THE JOURNAL OF PHARMACOLOGY AND EXPERIMENTAL THERAPEUTICS J Pharmacol Exp Ther 371:1–14, October 2019 Copyright ª 2019 by The Author(s) This is an open access article distributed under the CC BY-NC Attribution 4.0 International license. SEP-363856, a Novel Psychotropic Agent with a Unique, Non-D2 Receptor Mechanism of Action s Nina Dedic,1 Philip G. Jones,1 Seth C. Hopkins, Robert Lew, Liming Shao, John E. Campbell, Kerry L. Spear, Thomas H. Large, Una C. Campbell, Taleen Hanania, Emer Leahy, and Kenneth S. Koblan Sunovion Pharmaceuticals, Marlborough, Massachusetts (N.D., P.G.J., S.C.H., R.L., L.S., J.E.C., K.L.S., T.H.L., U.C.C., K.S.K.); and PsychoGenics, Paramus, New Jersey (T.H., E.L.) Received May 24, 2019; accepted July 10, 2019 Downloaded from ABSTRACT For the past 50 years, the clinical efficacy of antipsychotic amine-associated receptor 1 and 5-HT1A receptors is integral to medications has relied on blockade of dopamine D2 receptors. its efficacy. Based on the preclinical data and its unique Drug development of non-D2 compounds, seeking to avoid mechanism of action, SEP-856 is a promising new agent for the limiting side effects of dopamine receptor blockade, has the treatment of schizophrenia and represents a new pharma- jpet.aspetjournals.org failed to date to yield new medicines for patients. -

Torpor: the Rise and Fall of 3-Monoiodothyronamine from Brain to Gut—From Gut to Brain?
REVIEW published: 31 May 2017 doi: 10.3389/fendo.2017.00118 Torpor: The Rise and Fall of 3-Monoiodothyronamine from Brain to Gut—From Gut to Brain? Hartmut H. Glossmann1* and Oliver M. D. Lutz2 1 Institut für Biochemische Pharmakologie, Innsbruck, Austria, 2 Austrian Drug Screening Institute, Innsbruck, Austria 3-Monoiodothyronamine (T1AM), first isolated from rat brain, is reported to be an endogenous, rapidly acting metabolite of thyroxine. One of its numerous effects is the induction of a “torpor-like” state in experimental animals. A critical analysis of T1AM, to serve as an endogenous cryogen, is given. The proposed biosynthetic pathway for formation of T1AM, which includes deiodinases and ornithine decarboxylase in the upper intestinum, is an unusual one. To reach the brain via systemic circulation, enterohepatic recycling and passage through the liver may occur. The possible role of gut microbiota is discussed. T1AM concentrations in human serum, measured by a specific monoclonal assay are up to three orders of magnitude higher compared to values obtained by MS/ MS technology. The difference is explained by the presence of a high-affinity binder for T1AM (Apolipoprotein B-100) in serum, which permits the immunoassay to measure Edited by: Johannes Wolfgang Dietrich, the total concentration of the analyte but limits MS/MS technology to detect only the Ruhr University Bochum, Germany unbound (free) analyte, a view, which is contested here. Reviewed by: Keywords: T1AM, thyroxine, monoiodothyronamine, apolipoprotein B-100, hibernation, immunoassay, torpor, Steven Swoap, mass spectrometry Williams College, United States Franz Hofmann, Technische Universität München, 1. INTRODUCTION Germany *Correspondence: Hibernation has fascinated scientists for centuries (1–3).