The Involvement of Trace Amine-Associated Receptor 1 and Thyroid Hormone Transporters in Non-Classical Pathways of the Thyroid Gland Auto-Regulation
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Downloaded for Further Analysis
bioRxiv preprint doi: https://doi.org/10.1101/2020.09.10.288951; this version posted September 11, 2020. The copyright holder for this preprint (which was not certified by peer review) is the author/funder. All rights reserved. No reuse allowed without permission. Coordination of two enhancers drives expression of olfactory trace amine- associated receptors Aimei Fei1,8, Wanqing Wu1,8, Longzhi Tan3,8, Cheng Tang4,8, Zhengrong Xu1, Xiaona Huo4, Hongqiang Bao1, Mark Johnson5, Griffin Hartmann5, Mustafa Talay5, Cheng Yang1, Clemens Riegler6, Kristian Joseph6, Florian Engert6, X. Sunney Xie3, Gilad Barnea5, Stephen D. Liberles7, Hui Yang4, and Qian Li1,2,* 1Center for Brain Science, Shanghai Children's Medical Center, Department of Anatomy and Physiology, Shanghai Jiao Tong University School of Medicine, Shanghai 200025, China; 2Shanghai Research Center for Brain Science and Brain-Inspired Intelligence, Shanghai 201210, China; 3Department of Chemistry and Chemical Biology, Harvard University, Cambridge, MA 02138, USA; 4Institute of Neuroscience, State Key Laboratory of Neuroscience, Key Laboratory of Primate Neurobiology, CAS Center for Excellence in Brain Science and Intelligence Technology, Shanghai Research Center for Brain Science and Brian-Inspired Intelligence, Shanghai Institutes for Biological Sciences, Chinese Academy of Sciences, Shanghai 200031, China; 5Department of Neuroscience, Division of Biology and Medicine, Brown University, Providence, RI 02912, USA; 6Department of Molecular and Cellular Biology and Center for Brain Science, Harvard University, Cambridge, MA 02138, USA; 7Howard Hughes Medical Institute, Department of Cell Biology, Harvard Medical School, Boston, MA 02115, USA; 8These authors contributed equally to this work. *Correspondence to [email protected], phone: +86-21-63846590 ext. 776985 1 bioRxiv preprint doi: https://doi.org/10.1101/2020.09.10.288951; this version posted September 11, 2020. -

Novel Neuroprotective Compunds for Use in Parkinson's Disease
Novel neuroprotective compounds for use in Parkinson’s disease A thesis submitted to Kent State University in partial Fulfillment of the requirements for the Degree of Master of Science By Ahmed Shubbar December, 2013 Thesis written by Ahmed Shubbar B.S., University of Kufa, 2009 M.S., Kent State University, 2013 Approved by ______________________Werner Geldenhuys ____, Chair, Master’s Thesis Committee __________________________,Altaf Darvesh Member, Master’s Thesis Committee __________________________,Richard Carroll Member, Master’s Thesis Committee ___Eric_______________________ Mintz , Director, School of Biomedical Sciences ___Janis_______________________ Crowther , Dean, College of Arts and Sciences ii Table of Contents List of figures…………………………………………………………………………………..v List of tables……………………………………………………………………………………vi Acknowledgments.…………………………………………………………………………….vii Chapter 1: Introduction ..................................................................................... 1 1.1 Parkinson’s disease .............................................................................................. 1 1.2 Monoamine Oxidases ........................................................................................... 3 1.3 Monoamine Oxidase-B structure ........................................................................... 8 1.4 Structural differences between MAO-B and MAO-A .............................................13 1.5 Mechanism of oxidative deamination catalyzed by Monoamine Oxidases ............15 1 .6 Neuroprotective effects -

Is TAAR1 a Potential Therapeutic Target for Immune Dysregulation In
Graduate Physical and Life Sciences PhD Pharmacology Abstract ID# 1081 Is TAAR1 a Potential Therapeutic Target for Immune Dysregulation in Drug Abuse? Fleischer, Lisa M; Tamashunas, Nina and Miller, Gregory M Addiction Sciences Laboratory, Northeastern University, Boston MA 02115 Abstract Discovered in 2001, Trace Amine Associated Receptor 1 (TAAR1) is a direct target of Data and Results amphetamine, methamphetamine and MDMA. It is expressed in the brain reward circuity and modulates dopamine transporter function and dopamine neuron firing rates. Newly-developed compounds that specifically target TAAR1 have recently been investigated in animal models In addition to brain, TAAR1 is expressed in immune cells METH promotes PKA and PKC Phosphorylation through TAAR1 as candidate therapeutics for methamphetamine, cocaine and alcohol abuse. These studies • We treated HEK/TAAR1 cells and HEK293 involving classic behavioral measures of drug response, as well as drug self-administration, Rhesus and Human cells with vehicle or METH, with and without strongly implicate TAAR1 as a potential therapeutic target for the treatment of addiction. In activators and inhibitors of PKA and PKC. addition to its central actions, we demonstrated that TAAR1 is upregulated in peripheral blood Cells Lines mononuclear cells (PBMC) and B cells following immune activation, and that subsequent • We performed Western blotting experiments to activation of TAAR1 by methamphetamine stimulates cAMP, similar to the function of measure levels of phospho-PKA and phospho- adenosine A2 receptors which are also present in immune cells and play a critical role in the PKC. immune response. Here, we are investigating the relationship between TAAR1 and the • We found that specific activators of PKA and adenosine A2 receptor at the level of cellular signaling and receptor dimerization. -

Trace Amine-Associated Receptor 1 Activation Regulates Glucose-Dependent
Trace amine-associated receptor 1 activation regulates glucose-dependent insulin secretion in pancreatic beta cells in vitro by ©Arun Kumar A thesis submitted to the School of Graduate Studies in partial fulfillment of the requirements for the degree of Master of Science Department of Biochemistry, Faculty of Science Memorial University of Newfoundland FEBRUARY 2021 St. John’s, Newfoundland and Labrador i Abstract Trace amines are a group of endogenous monoamines which exert their action through a family of G protein-coupled receptors known as trace amine-associated receptors (TAARs). TAAR1 has been reported to regulate insulin secretion from pancreatic beta cells in vitro and in vivo. This study investigates the mechanism(s) by which TAAR1 regulates insulin secretion. The insulin secreting rat INS-1E -cell line was used for the study. Cells were pre-starved (30 minutes) and then incubated with varying concentrations of glucose (2.5 – 20 mM) or KCl (3.6 – 60 mM) for 2 hours in the absence or presence of various concentrations of the selective TAAR1 agonist RO5256390. Secreted insulin per well was quantified using ELISA and normalized to the total protein content of individual cultures. RO5256390 significantly (P < 0.0001) increased glucose- stimulated insulin secretion in a dose-dependent manner, with no effect on KCl-stimulated insulin secretion. Affymetrix-microarray data analysis identified genes (Gnas, Gng7, Gngt1, Gria2, Cacna1e, Kcnj8, and Kcnj11) whose expression was associated with changes in TAAR1 in response to changes in insulin secretion in pancreatic beta cell function. The identified potential links to TAAR1 supports the regulation of glucose-stimulated insulin secretion through KATP ion channels. -
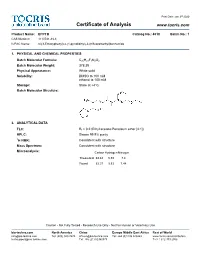
Certificate of Analysis
Print Date: Jan 3rd 2020 Certificate of Analysis www.tocris.com Product Name: EPPTB Catalog No.: 4518 Batch No.: 1 CAS Number: 1110781-88-8 IUPAC Name: N-(3-Ethoxyphenyl)-4-(1-pyrrolidinyl)-3-(trifluoromethyl)benzamide 1. PHYSICAL AND CHEMICAL PROPERTIES Batch Molecular Formula: C20H21F3N2O2 Batch Molecular Weight: 378.39 Physical Appearance: White solid Solubility: DMSO to 100 mM ethanol to 100 mM Storage: Store at +4°C Batch Molecular Structure: 2. ANALYTICAL DATA TLC: Rf = 0.2 (Ethyl acetate:Petroleum ether [4:1]) HPLC: Shows 99.9% purity 1H NMR: Consistent with structure Mass Spectrum: Consistent with structure Microanalysis: Carbon Hydrogen Nitrogen Theoretical 63.48 5.59 7.4 Found 63.37 5.53 7.44 Caution - Not Fully Tested • Research Use Only • Not For Human or Veterinary Use bio-techne.com North America China Europe Middle East Africa Rest of World [email protected] Tel: (800) 343 7475 [email protected] Tel: +44 (0)1235 529449 www.tocris.com/distributors [email protected] Tel: +86 (21) 52380373 Tel:+1 612 379 2956 Print Date: Jan 3rd 2020 Product Information www.tocris.com Product Name: EPPTB Catalog No.: 4518 Batch No.: 1 CAS Number: 1110781-88-8 IUPAC Name: N-(3-Ethoxyphenyl)-4-(1-pyrrolidinyl)-3-(trifluoromethyl)benzamide Description: Storage: Store at +4°C Trace amine 1 (TA ) receptor antagonist/inverse agonist; 1 Solubility & Usage Info: exhibits a higher potency at the mouse TA1 receptor than the rat DMSO to 100 mM and human TA150 receptors (IC values are 27.5, 4539 and 7487 ethanol to 100 mM nM, respectively). -

S41598-021-90243-1.Pdf
www.nature.com/scientificreports OPEN Metabolomics and computational analysis of the role of monoamine oxidase activity in delirium and SARS‑COV‑2 infection Miroslava Cuperlovic‑Culf1,2*, Emma L. Cunningham3, Hossen Teimoorinia4, Anuradha Surendra1, Xiaobei Pan5, Stefany A. L. Bennett2,6, Mijin Jung5, Bernadette McGuiness3, Anthony Peter Passmore3, David Beverland7 & Brian D. Green5* Delirium is an acute change in attention and cognition occurring in ~ 65% of severe SARS‑CoV‑2 cases. It is also common following surgery and an indicator of brain vulnerability and risk for the development of dementia. In this work we analyzed the underlying role of metabolism in delirium‑ susceptibility in the postoperative setting using metabolomic profling of cerebrospinal fuid and blood taken from the same patients prior to planned orthopaedic surgery. Distance correlation analysis and Random Forest (RF) feature selection were used to determine changes in metabolic networks. We found signifcant concentration diferences in several amino acids, acylcarnitines and polyamines linking delirium‑prone patients to known factors in Alzheimer’s disease such as monoamine oxidase B (MAOB) protein. Subsequent computational structural comparison between MAOB and angiotensin converting enzyme 2 as well as protein–protein docking analysis showed that there potentially is strong binding of SARS‑CoV‑2 spike protein to MAOB. The possibility that SARS‑CoV‑2 infuences MAOB activity leading to the observed neurological and platelet‑based complications of SARS‑CoV‑2 infection requires further investigation. COVID-19 is an ongoing major global health emergency caused by severe acute respiratory syndrome coro- navirus SARS-CoV-2. Patients admitted to hospital with COVID-19 show a range of features including fever, anosmia, acute respiratory failure, kidney failure and gastrointestinal issues and the death rate of infected patients is estimated at 2.2%1. -

Modulation by Trace Amine-Associated Receptor 1 of Experimental Parkinsonism, L-DOPA Responsivity, and Glutamatergic Neurotransmission
The Journal of Neuroscience, October 14, 2015 • 35(41):14057–14069 • 14057 Neurobiology of Disease Modulation by Trace Amine-Associated Receptor 1 of Experimental Parkinsonism, L-DOPA Responsivity, and Glutamatergic Neurotransmission Alexandra Alvarsson,1* Xiaoqun Zhang,1* Tiberiu L Stan,1 Nicoletta Schintu,1 Banafsheh Kadkhodaei,2 Mark J. Millan,3 Thomas Perlmann,2,4 and Per Svenningsson1 1Department of Clinical Neuroscience, Center for Molecular Medicine, Karolinska Institutet, SE-17176 Stockholm, Sweden, 2Ludwig Institute for Cancer Research, SE-17177 Stockholm, Sweden, 3Pole of Innovation in Neuropsychiatry, Institut de Recherches Servier, Centre de Recherches de Croissy, Paris 87290, France, and 4Department of Cell and Molecular Biology, Karolinska Institutet, SE-17177 Stockholm, Sweden Parkinson’s disease (PD) is a movement disorder characterized by a progressive loss of nigrostriatal dopaminergic neurons. Restoration of dopamine transmission by L-DOPA relieves symptoms of PD but causes dyskinesia. Trace Amine-Associated Receptor 1 (TAAR1) modulates dopaminergic transmission, but its role in experimental Parkinsonism and L-DOPA responses has been neglected. Here, we report that TAAR1 knock-out (KO) mice show a reduced loss of dopaminergic markers in response to intrastriatal 6-OHDA administra- tion compared with wild-type (WT) littermates. In contrast, the TAAR1 agonist RO5166017 aggravated degeneration induced by intra- striatal6-OHDAinWTmice.Subchronic L-DOPAtreatmentofTAAR1KOmiceunilaterallylesionedwith6-OHDAinthemedialforebrain bundle resulted in more pronounced rotational behavior and dyskinesia than in their WT counterparts. The enhanced behavioral sensitization to L-DOPA in TAAR1 KO mice was paralleled by increased phosphorylation of striatal GluA1 subunits of AMPA receptors. Conversely, RO5166017 counteracted both L-DOPA-induced rotation and dyskinesia as well as AMPA receptor phosphorylation. -

TRAR4 (TAAR6) (NM 175067) Human Tagged ORF Clone Lentiviral Particle Product Data
OriGene Technologies, Inc. 9620 Medical Center Drive, Ste 200 Rockville, MD 20850, US Phone: +1-888-267-4436 [email protected] EU: [email protected] CN: [email protected] Product datasheet for RC220756L3V TRAR4 (TAAR6) (NM_175067) Human Tagged ORF Clone Lentiviral Particle Product data: Product Type: Lentiviral Particles Product Name: TRAR4 (TAAR6) (NM_175067) Human Tagged ORF Clone Lentiviral Particle Symbol: TAAR6 Synonyms: TA4; taR-4; taR-6; TAR4; TAR6; TRAR4 Vector: pLenti-C-Myc-DDK-P2A-Puro (PS100092) ACCN: NM_175067 ORF Size: 1035 bp ORF Nucleotide The ORF insert of this clone is exactly the same as(RC220756). Sequence: OTI Disclaimer: The molecular sequence of this clone aligns with the gene accession number as a point of reference only. However, individual transcript sequences of the same gene can differ through naturally occurring variations (e.g. polymorphisms), each with its own valid existence. This clone is substantially in agreement with the reference, but a complete review of all prevailing variants is recommended prior to use. More info OTI Annotation: This clone was engineered to express the complete ORF with an expression tag. Expression varies depending on the nature of the gene. RefSeq: NM_175067.1, NP_778237.1 RefSeq Size: 1038 bp RefSeq ORF: 1038 bp Locus ID: 319100 UniProt ID: Q96RI8 Protein Families: Druggable Genome, GPCR, Transmembrane Protein Pathways: Neuroactive ligand-receptor interaction MW: 38.3 kDa Gene Summary: This gene encodes a seven-transmembrane G-protein-coupled receptor that likely functions as a receptor for endogenous trace amines. Mutations in this gene may be associated with schizophrenia.[provided by RefSeq, Feb 2010] This product is to be used for laboratory only. -

Decarboxylation What Is Decarboxylation?
Decarboxylation What is decarboxylation? Decarboxylation is the removal of a carboxyl group when a compound is exposed to light or heat. A carboxyl group is a grouping of carbon, oxygen, and hydrogen atoms in the form of COOH. When a compound is decarboxylated, this group is released in the form of carbon dioxide. Decarboxylation of cannabinoids When considering the decarboxylation of cannabinoids, it is important to note that this reaction is what causes the neutral acidic cannabinoids to turn into the active cannabinoids found in most products on the market. Both the neutral and acidic cannabinoids are naturally found in the cannabis plant. The active cannabinoids that have psychoactive properties are what occur after decarboxylation. Below is the mechanism for the conversion of THCA to THC. https://www.leafscience.com/2017/04/13/what-is-thca/ Heating THCA converts it to THC by kicking off the carboxyl group seen on the right side of the THCA molecule. Once the carboxyl group is released from the THCA it forms carbon dioxide and the THC compound. The THC is now ready for use in different products and will provide the psychoactive effects that popularized this compound. This simple reaction is all it takes to convert the acidic cannabinoids to their active counterparts. Cannabinolic acid (CBDA) and CBD are both another example of this process. Decarboxylation process Light can start the decarboxylation process after a period of time, but heat is the more common element used. There are different methods to decarboxylate cannabis depending on user preference. In the industry, dabs, vapes and joints decarboxylate instantly when heat is applied to the product. -

Jenna K. Caines, Sherri L. Christian, Mark D. Berry Department of Biochemistry, Memorial University of Newfoundland, St. John'
Trace Amine-Associated Receptors in Monocytes: A Constant Low-Level Expression Jenna K. Caines, Sherri L. Christian, Mark D. Berry Department of Biochemistry, Memorial University of Newfoundland, St. John’s NL Trace amine-associated receptors (TAARs) Is TAAR1 differentially expressed in response to Pro- and Are any TAARs differentially expressed between § G protein-coupled receptors anti-inflammatory stimuli? monocyte and macrophage lineages? § Established throughout the body in vertebrates Table 1: Datasets with n ≥ 3 examining human and mice macrophages Table 2: Datasets with n ≥ 3 containing several monocyte and § Humans have 6 functional isoforms: TAAR1, TAAR2, TAAR5, TAAR6, TAAR8, and TAAR9 treated with pro- and anti-inflammatory stimuli macrophage lineages from mice TAARs and the immune system Dataset Treatment Time TAAR1 p-value Dataset Cell type Number of lineages Treatment § Found in leukocyte populations1 GSE53986 Untreated (control) 0h examined INFγ 24h 0.8 GSE15907 Lung Macrophage 2 NA 1 § TAAR1 suspected of regulating immune response GSE60290 Untreated (control) 0h Peritoneal Macrophage 6 NA § Potential target for pharmacological treatment of immune disorders2 INFγ 18h 0.3 Spleen Macrophage NA GSE43075 Untreated (control) 0h Blood Monocyte 2 NA Hypothesis LPS 4h 0.45 Mesenteric LN monocyte 1 NA GSE121646 Untreated (control) 0h Oral Salmonella § TAAR1 will show differential expression upon activation and LPS 8h 0.7 Small intestine macrophage 2 Typhimurium(72 h) GSE19315 Untreated (control) 0h between leukocyte populations -

Optimization of the Decarboxylation Reaction in Cannabis
APPLICATION NOTE FT-IR Spectroscopy Authors: Dr. Markus Roggen1 Antonio M. Marelli1 Doug Townsend2 Ariel Bohman2 1Outco SanDiego, CA 2PerkinElmer, Inc. Shelton, CT. Optimization of the Decarboxylation Reaction Introduction The production of cannabis in Cannabis Extract extracts and oils for medicinal and recreational products has increased significantly in North America. This growth has been driven by both market demand in newly legalized states and patient demand for a greater diversity in cannabis products.1,2,3 Most cannabis extraction processes, independent of solvent or instrument choice, undergo a decarboxylation step whereby the carboxylic acid functional group is removed from the cannabinoids. The decarboxylation reaction converts the naturally occurring acid forms of the cannabinoids, e.g. tetrahydrocannabinolic acid (THCA) and cannabidiolic acid (CBDA), to their more potent neutral forms, e.g. tetrahydrocannabinol (THC) and cannabidiol (CBD). Because the carboxylic acid group is thermally labile, the industry typically applies a heat source, and at times a catalyst, to decarboxylate the cannabinoids. The heat-promoted decarboxylation reaction has been Decarboxylation Reaction discussed at length within the industry, but an extensive Decarboxylation was achieved by heating the cannabis extract in 4, 5, 6 literature search reveals very few papers on the process. a oil bath with a programmable hot plate. An overhead stirrer The data available represents a large spectrum of reaction was utilized to promote even heat distribution throughout the conditions, including a range in reaction temperature, time experiment. Oil bath and extract temperatures were recorded and instrumental setup. As such, there is a lack of universal every five minutes throughout the 80-minute heating process. -

Citric Acid Cycle
CHEM464 / Medh, J.D. The Citric Acid Cycle Citric Acid Cycle: Central Role in Catabolism • Stage II of catabolism involves the conversion of carbohydrates, fats and aminoacids into acetylCoA • In aerobic organisms, citric acid cycle makes up the final stage of catabolism when acetyl CoA is completely oxidized to CO2. • Also called Krebs cycle or tricarboxylic acid (TCA) cycle. • It is a central integrative pathway that harvests chemical energy from biological fuel in the form of electrons in NADH and FADH2 (oxidation is loss of electrons). • NADH and FADH2 transfer electrons via the electron transport chain to final electron acceptor, O2, to form H2O. Entry of Pyruvate into the TCA cycle • Pyruvate is formed in the cytosol as a product of glycolysis • For entry into the TCA cycle, it has to be converted to Acetyl CoA. • Oxidation of pyruvate to acetyl CoA is catalyzed by the pyruvate dehydrogenase complex in the mitochondria • Mitochondria consist of inner and outer membranes and the matrix • Enzymes of the PDH complex and the TCA cycle (except succinate dehydrogenase) are in the matrix • Pyruvate translocase is an antiporter present in the inner mitochondrial membrane that allows entry of a molecule of pyruvate in exchange for a hydroxide ion. 1 CHEM464 / Medh, J.D. The Citric Acid Cycle The Pyruvate Dehydrogenase (PDH) complex • The PDH complex consists of 3 enzymes. They are: pyruvate dehydrogenase (E1), Dihydrolipoyl transacetylase (E2) and dihydrolipoyl dehydrogenase (E3). • It has 5 cofactors: CoASH, NAD+, lipoamide, TPP and FAD. CoASH and NAD+ participate stoichiometrically in the reaction, the other 3 cofactors have catalytic functions.