The Modulatory Role of Taar1 in Neurotoxicity of Substituted Amphetamines
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Novel Neuroprotective Compunds for Use in Parkinson's Disease
Novel neuroprotective compounds for use in Parkinson’s disease A thesis submitted to Kent State University in partial Fulfillment of the requirements for the Degree of Master of Science By Ahmed Shubbar December, 2013 Thesis written by Ahmed Shubbar B.S., University of Kufa, 2009 M.S., Kent State University, 2013 Approved by ______________________Werner Geldenhuys ____, Chair, Master’s Thesis Committee __________________________,Altaf Darvesh Member, Master’s Thesis Committee __________________________,Richard Carroll Member, Master’s Thesis Committee ___Eric_______________________ Mintz , Director, School of Biomedical Sciences ___Janis_______________________ Crowther , Dean, College of Arts and Sciences ii Table of Contents List of figures…………………………………………………………………………………..v List of tables……………………………………………………………………………………vi Acknowledgments.…………………………………………………………………………….vii Chapter 1: Introduction ..................................................................................... 1 1.1 Parkinson’s disease .............................................................................................. 1 1.2 Monoamine Oxidases ........................................................................................... 3 1.3 Monoamine Oxidase-B structure ........................................................................... 8 1.4 Structural differences between MAO-B and MAO-A .............................................13 1.5 Mechanism of oxidative deamination catalyzed by Monoamine Oxidases ............15 1 .6 Neuroprotective effects -

TABLE 1 Studies of Antagonist Activity in Constitutively Active
TABLE 1 Studies of antagonist activity in constitutively active receptors systems shown to demonstrate inverse agonism for at least one ligand Targets are natural Gs and constitutively active mutants (CAM) of GPCRs. Of 380 antagonists, 85% of the ligands demonstrate inverse agonism. Receptor Neutral Antagonist Inverse Agonist Reference Human β2-adrenergic Dichloroisoproterenol, pindolol, labetolol, timolol, Chidiac et al., 1996; Azzi et alprenolol, propranolol, ICI 118,551, cyanopindolol al., 2001 Turkey erythrocyte β-adrenergic Propranolol, pindolol Gotze et al., 1994 Human β2-adrenergic (CAM) Propranolol Betaxolol, ICI 118,551, sotalol, timolol Samama et al., 1994; Stevens and Milligan, 1998 Human/guinea pig β1-adrenergic Atenolol, propranolol Mewes et al., 1993 Human β1-adrenergic Carvedilol CGP20712A, metoprolol, bisoprolol Engelhardt et al., 2001 Rat α2D-adrenergic Rauwolscine, yohimbine, WB 4101, idazoxan, Tian et al., 1994 phentolamine, Human α2A-adrenergic Napthazoline, Rauwolscine, idazoxan, altipamezole, levomedetomidine, Jansson et al., 1998; Pauwels MPV-2088 (–)RX811059, RX 831003 et al., 2002 Human α2C-adrenergic RX821002, yohimbine Cayla et al., 1999 Human α2D-adrenergic Prazosin McCune et al., 2000 Rat α2-adrenoceptor MK912 RX821002 Murrin et al., 2000 Porcine α2A adrenoceptor (CAM- Idazoxan Rauwolscine, yohimbine, RX821002, MK912, Wade et al., 2001 T373K) phentolamine Human α2A-adrenoceptor (CAM) Dexefaroxan, (+)RX811059, (–)RX811059, RS15385, yohimbine, Pauwels et al., 2000 atipamezole fluparoxan, WB 4101 Hamster α1B-adrenergic -

Is TAAR1 a Potential Therapeutic Target for Immune Dysregulation In
Graduate Physical and Life Sciences PhD Pharmacology Abstract ID# 1081 Is TAAR1 a Potential Therapeutic Target for Immune Dysregulation in Drug Abuse? Fleischer, Lisa M; Tamashunas, Nina and Miller, Gregory M Addiction Sciences Laboratory, Northeastern University, Boston MA 02115 Abstract Discovered in 2001, Trace Amine Associated Receptor 1 (TAAR1) is a direct target of Data and Results amphetamine, methamphetamine and MDMA. It is expressed in the brain reward circuity and modulates dopamine transporter function and dopamine neuron firing rates. Newly-developed compounds that specifically target TAAR1 have recently been investigated in animal models In addition to brain, TAAR1 is expressed in immune cells METH promotes PKA and PKC Phosphorylation through TAAR1 as candidate therapeutics for methamphetamine, cocaine and alcohol abuse. These studies • We treated HEK/TAAR1 cells and HEK293 involving classic behavioral measures of drug response, as well as drug self-administration, Rhesus and Human cells with vehicle or METH, with and without strongly implicate TAAR1 as a potential therapeutic target for the treatment of addiction. In activators and inhibitors of PKA and PKC. addition to its central actions, we demonstrated that TAAR1 is upregulated in peripheral blood Cells Lines mononuclear cells (PBMC) and B cells following immune activation, and that subsequent • We performed Western blotting experiments to activation of TAAR1 by methamphetamine stimulates cAMP, similar to the function of measure levels of phospho-PKA and phospho- adenosine A2 receptors which are also present in immune cells and play a critical role in the PKC. immune response. Here, we are investigating the relationship between TAAR1 and the • We found that specific activators of PKA and adenosine A2 receptor at the level of cellular signaling and receptor dimerization. -

Trace Amine-Associated Receptor 1 Activation Regulates Glucose-Dependent
Trace amine-associated receptor 1 activation regulates glucose-dependent insulin secretion in pancreatic beta cells in vitro by ©Arun Kumar A thesis submitted to the School of Graduate Studies in partial fulfillment of the requirements for the degree of Master of Science Department of Biochemistry, Faculty of Science Memorial University of Newfoundland FEBRUARY 2021 St. John’s, Newfoundland and Labrador i Abstract Trace amines are a group of endogenous monoamines which exert their action through a family of G protein-coupled receptors known as trace amine-associated receptors (TAARs). TAAR1 has been reported to regulate insulin secretion from pancreatic beta cells in vitro and in vivo. This study investigates the mechanism(s) by which TAAR1 regulates insulin secretion. The insulin secreting rat INS-1E -cell line was used for the study. Cells were pre-starved (30 minutes) and then incubated with varying concentrations of glucose (2.5 – 20 mM) or KCl (3.6 – 60 mM) for 2 hours in the absence or presence of various concentrations of the selective TAAR1 agonist RO5256390. Secreted insulin per well was quantified using ELISA and normalized to the total protein content of individual cultures. RO5256390 significantly (P < 0.0001) increased glucose- stimulated insulin secretion in a dose-dependent manner, with no effect on KCl-stimulated insulin secretion. Affymetrix-microarray data analysis identified genes (Gnas, Gng7, Gngt1, Gria2, Cacna1e, Kcnj8, and Kcnj11) whose expression was associated with changes in TAAR1 in response to changes in insulin secretion in pancreatic beta cell function. The identified potential links to TAAR1 supports the regulation of glucose-stimulated insulin secretion through KATP ion channels. -
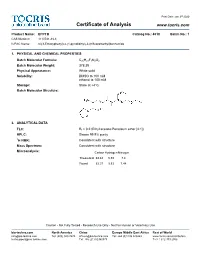
Certificate of Analysis
Print Date: Jan 3rd 2020 Certificate of Analysis www.tocris.com Product Name: EPPTB Catalog No.: 4518 Batch No.: 1 CAS Number: 1110781-88-8 IUPAC Name: N-(3-Ethoxyphenyl)-4-(1-pyrrolidinyl)-3-(trifluoromethyl)benzamide 1. PHYSICAL AND CHEMICAL PROPERTIES Batch Molecular Formula: C20H21F3N2O2 Batch Molecular Weight: 378.39 Physical Appearance: White solid Solubility: DMSO to 100 mM ethanol to 100 mM Storage: Store at +4°C Batch Molecular Structure: 2. ANALYTICAL DATA TLC: Rf = 0.2 (Ethyl acetate:Petroleum ether [4:1]) HPLC: Shows 99.9% purity 1H NMR: Consistent with structure Mass Spectrum: Consistent with structure Microanalysis: Carbon Hydrogen Nitrogen Theoretical 63.48 5.59 7.4 Found 63.37 5.53 7.44 Caution - Not Fully Tested • Research Use Only • Not For Human or Veterinary Use bio-techne.com North America China Europe Middle East Africa Rest of World [email protected] Tel: (800) 343 7475 [email protected] Tel: +44 (0)1235 529449 www.tocris.com/distributors [email protected] Tel: +86 (21) 52380373 Tel:+1 612 379 2956 Print Date: Jan 3rd 2020 Product Information www.tocris.com Product Name: EPPTB Catalog No.: 4518 Batch No.: 1 CAS Number: 1110781-88-8 IUPAC Name: N-(3-Ethoxyphenyl)-4-(1-pyrrolidinyl)-3-(trifluoromethyl)benzamide Description: Storage: Store at +4°C Trace amine 1 (TA ) receptor antagonist/inverse agonist; 1 Solubility & Usage Info: exhibits a higher potency at the mouse TA1 receptor than the rat DMSO to 100 mM and human TA150 receptors (IC values are 27.5, 4539 and 7487 ethanol to 100 mM nM, respectively). -

S41598-021-90243-1.Pdf
www.nature.com/scientificreports OPEN Metabolomics and computational analysis of the role of monoamine oxidase activity in delirium and SARS‑COV‑2 infection Miroslava Cuperlovic‑Culf1,2*, Emma L. Cunningham3, Hossen Teimoorinia4, Anuradha Surendra1, Xiaobei Pan5, Stefany A. L. Bennett2,6, Mijin Jung5, Bernadette McGuiness3, Anthony Peter Passmore3, David Beverland7 & Brian D. Green5* Delirium is an acute change in attention and cognition occurring in ~ 65% of severe SARS‑CoV‑2 cases. It is also common following surgery and an indicator of brain vulnerability and risk for the development of dementia. In this work we analyzed the underlying role of metabolism in delirium‑ susceptibility in the postoperative setting using metabolomic profling of cerebrospinal fuid and blood taken from the same patients prior to planned orthopaedic surgery. Distance correlation analysis and Random Forest (RF) feature selection were used to determine changes in metabolic networks. We found signifcant concentration diferences in several amino acids, acylcarnitines and polyamines linking delirium‑prone patients to known factors in Alzheimer’s disease such as monoamine oxidase B (MAOB) protein. Subsequent computational structural comparison between MAOB and angiotensin converting enzyme 2 as well as protein–protein docking analysis showed that there potentially is strong binding of SARS‑CoV‑2 spike protein to MAOB. The possibility that SARS‑CoV‑2 infuences MAOB activity leading to the observed neurological and platelet‑based complications of SARS‑CoV‑2 infection requires further investigation. COVID-19 is an ongoing major global health emergency caused by severe acute respiratory syndrome coro- navirus SARS-CoV-2. Patients admitted to hospital with COVID-19 show a range of features including fever, anosmia, acute respiratory failure, kidney failure and gastrointestinal issues and the death rate of infected patients is estimated at 2.2%1. -

Modulation by Trace Amine-Associated Receptor 1 of Experimental Parkinsonism, L-DOPA Responsivity, and Glutamatergic Neurotransmission
The Journal of Neuroscience, October 14, 2015 • 35(41):14057–14069 • 14057 Neurobiology of Disease Modulation by Trace Amine-Associated Receptor 1 of Experimental Parkinsonism, L-DOPA Responsivity, and Glutamatergic Neurotransmission Alexandra Alvarsson,1* Xiaoqun Zhang,1* Tiberiu L Stan,1 Nicoletta Schintu,1 Banafsheh Kadkhodaei,2 Mark J. Millan,3 Thomas Perlmann,2,4 and Per Svenningsson1 1Department of Clinical Neuroscience, Center for Molecular Medicine, Karolinska Institutet, SE-17176 Stockholm, Sweden, 2Ludwig Institute for Cancer Research, SE-17177 Stockholm, Sweden, 3Pole of Innovation in Neuropsychiatry, Institut de Recherches Servier, Centre de Recherches de Croissy, Paris 87290, France, and 4Department of Cell and Molecular Biology, Karolinska Institutet, SE-17177 Stockholm, Sweden Parkinson’s disease (PD) is a movement disorder characterized by a progressive loss of nigrostriatal dopaminergic neurons. Restoration of dopamine transmission by L-DOPA relieves symptoms of PD but causes dyskinesia. Trace Amine-Associated Receptor 1 (TAAR1) modulates dopaminergic transmission, but its role in experimental Parkinsonism and L-DOPA responses has been neglected. Here, we report that TAAR1 knock-out (KO) mice show a reduced loss of dopaminergic markers in response to intrastriatal 6-OHDA administra- tion compared with wild-type (WT) littermates. In contrast, the TAAR1 agonist RO5166017 aggravated degeneration induced by intra- striatal6-OHDAinWTmice.Subchronic L-DOPAtreatmentofTAAR1KOmiceunilaterallylesionedwith6-OHDAinthemedialforebrain bundle resulted in more pronounced rotational behavior and dyskinesia than in their WT counterparts. The enhanced behavioral sensitization to L-DOPA in TAAR1 KO mice was paralleled by increased phosphorylation of striatal GluA1 subunits of AMPA receptors. Conversely, RO5166017 counteracted both L-DOPA-induced rotation and dyskinesia as well as AMPA receptor phosphorylation. -

Acetylcholinesterase and Monoamine Oxidase-B Inhibitory Activities By
www.nature.com/scientificreports OPEN Acetylcholinesterase and monoamine oxidase‑B inhibitory activities by ellagic acid derivatives isolated from Castanopsis cuspidata var. sieboldii Jong Min Oh1, Hyun‑Jae Jang2, Myung‑Gyun Kang3, Soobin Song2, Doo‑Young Kim2, Jung‑Hee Kim2, Ji‑In Noh1, Jong Eun Park1, Daeui Park3, Sung‑Tae Yee1 & Hoon Kim1* Among 276 herbal extracts, a methanol extract of Castanopsis cuspidata var. sieboldii stems was selected as an experimental source for novel acetylcholinesterase (AChE) inhibitors. Five compounds were isolated from the extract by activity‑guided screening, and their inhibitory activities against butyrylcholinesterase (BChE), monoamine oxidases (MAOs), and β‑site amyloid precursor protein cleaving enzyme 1 (BACE‑1) were also evaluated. Of these compounds, 4′‑O‑(α‑l‑rhamnopyranosyl)‑ 3,3′,4‑tri‑O‑methylellagic acid (3) and 3,3′,4‑tri‑O‑methylellagic acid (4) efectively inhibited AChE with IC50 values of 10.1 and 10.7 µM, respectively. Ellagic acid (5) inhibited AChE (IC50 = 41.7 µM) less than 3 and 4. In addition, 3 efectively inhibited MAO‑B (IC50 = 7.27 µM) followed by 5 (IC50 = 9.21 µM). All fve compounds weakly inhibited BChE and BACE‑1. Compounds 3, 4, and 5 reversibly and competitively inhibited AChE, and were slightly or non‑toxic to MDCK cells. The binding energies of 3 and 4 (− 8.5 and − 9.2 kcal/mol, respectively) for AChE were greater than that of 5 (− 8.3 kcal/mol), and 3 and 4 formed a hydrogen bond with Tyr124 in AChE. These results suggest 3 is a dual‑targeting inhibitor of AChE and MAO‑B, and that these compounds should be viewed as potential therapeutics for the treatment of Alzheimer’s disease. -

Effects of an Anti-Inflammatory VAP-1/SSAO Inhibitor, PXS-4728A
Schilter et al. Respiratory Research (2015) 16:42 DOI 10.1186/s12931-015-0200-z RESEARCH Open Access Effects of an anti-inflammatory VAP-1/SSAO inhibitor, PXS-4728A, on pulmonary neutrophil migration Heidi C Schilter1*†, Adam Collison2†, Remo C Russo3,4†, Jonathan S Foot1, Tin T Yow1, Angelica T Vieira4, Livia D Tavares4, Joerg Mattes2, Mauro M Teixeira4 and Wolfgang Jarolimek1,5 Abstract Background and purpose: The persistent influx of neutrophils into the lung and subsequent tissue damage are characteristics of COPD, cystic fibrosis and acute lung inflammation. VAP-1/SSAO is an endothelial bound adhesion molecule with amine oxidase activity that is reported to be involved in neutrophil egress from the microvasculature during inflammation. This study explored the role of VAP-1/SSAO in neutrophilic lung mediated diseases and examined the therapeutic potential of the selective inhibitor PXS-4728A. Methods: Mice treated with PXS-4728A underwent intra-vital microscopy visualization of the cremaster muscle upon CXCL1/KC stimulation. LPS inflammation, Klebsiella pneumoniae infection, cecal ligation and puncture as well as rhinovirus exacerbated asthma models were also assessed using PXS-4728A. Results: Selective VAP-1/SSAO inhibition by PXS-4728A diminished leukocyte rolling and adherence induced by CXCL1/KC. Inhibition of VAP-1/SSAO also dampened the migration of neutrophils to the lungs in response to LPS, Klebsiella pneumoniae lung infection and CLP induced sepsis; whilst still allowing for normal neutrophil defense function, resulting in increased survival. The functional effects of this inhibition were demonstrated in the RV exacerbated asthma model, with a reduction in cellular infiltrate correlating with a reduction in airways hyperractivity. -

Effects of the Trace Amine Associated Receptor 1 Agonist RO5263397 On
International Journal of Neuropsychopharmacology, 2015, 1–7 doi:10.1093/ijnp/pyu060 Research Article research article Effects of the Trace Amine Associated Receptor 1 Agonist RO5263397 on Abuse-Related Behavioral Indices of Methamphetamine in Rats Li Jing, PhD; Yanan Zhang, PhD; Jun-Xu Li, PhD Department of Pharmacology and Toxicology, School of Medicine and Biomedical Sciences, University at Buffalo, Buffalo, NY (Drs Jing and Li); Department of Physiology and Pathophysiology, Tianjin Medical University, Tianjin, China (Dr Jing); Research Triangle Institute, Research Triangle Park, NC (Dr Zhang). Correspondence: Jun-Xu Li, PhD, Department of Pharmacology and Toxicology, School of Medicine and Biomedical Sciences, University at Buffalo, Buffalo, NY ([email protected]). Abstract Background: Methamphetamine is a major drug of abuse with no effective pharmacotherapy available. Trace amine associated receptor 1 is implicated in cocaine addiction and represents a potential therapeutic target. However, the effects of trace amine associated receptor 1 agonists on addiction-related behavioral effects of methamphetamine are unknown. Methods: This study examined the effects of a trace amine associated receptor 1 agonist RO5263397 on methamphetamine- induced behavioral sensitization, methamphetamine self-administration, cue- and methamphetamine-induced reinstatement of drug seeking, and cue-induced reinstatement of sucrose-seeking behaviors in rats. Male Sprague-Dawley rats were used to examine the effects of methamphetamine alone and in combination with the trace amine associated receptor 1 agonist RO5263397 (3.2–10 mg/kg). Results: RO5263397 dose-dependently attenuated the expression of behavioral sensitization to methamphetamine, reduced methamphetamine self-administration, and decreased both cue- and a priming dose of methamphetamine-induced reinstatement of drug-seeking behaviors. -

Zebrafish Behavioral Profiling Links Drugs to Biological Targets and Rest/Wake Regulation
www.sciencemag.org/cgi/content/full/327/5963/348/DC1 Supporting Online Material for Zebrafish Behavioral Profiling Links Drugs to Biological Targets and Rest/Wake Regulation Jason Rihel,* David A. Prober, Anthony Arvanites, Kelvin Lam, Steven Zimmerman, Sumin Jang, Stephen J. Haggarty, David Kokel, Lee L. Rubin, Randall T. Peterson, Alexander F. Schier* *To whom correspondence should be addressed. E-mail: [email protected] (A.F.S.); [email protected] (J.R.) Published 15 January 2010, Science 327, 348 (2010) DOI: 10.1126/science.1183090 This PDF file includes: Materials and Methods SOM Text Figs. S1 to S18 Table S1 References Supporting Online Material Table of Contents Materials and Methods, pages 2-4 Supplemental Text 1-7, pages 5-10 Text 1. Psychotropic Drug Discovery, page 5 Text 2. Dose, pages 5-6 Text 3. Therapeutic Classes of Drugs Induce Correlated Behaviors, page 6 Text 4. Polypharmacology, pages 6-7 Text 5. Pharmacological Conservation, pages 7-9 Text 6. Non-overlapping Regulation of Rest/Wake States, page 9 Text 7. High Throughput Behavioral Screening in Practice, page 10 Supplemental Figure Legends, pages 11-14 Figure S1. Expanded hierarchical clustering analysis, pages 15-18 Figure S2. Hierarchical and k-means clustering yield similar cluster architectures, page 19 Figure S3. Expanded k-means clustergram, pages 20-23 Figure S4. Behavioral fingerprints are stable across a range of doses, page 24 Figure S5. Compounds that share biological targets have highly correlated behavioral fingerprints, page 25 Figure S6. Examples of compounds that share biological targets and/or structural similarity that give similar behavioral profiles, page 26 Figure S7. -

)&F1y3x PHARMACEUTICAL APPENDIX to THE
)&f1y3X PHARMACEUTICAL APPENDIX TO THE HARMONIZED TARIFF SCHEDULE )&f1y3X PHARMACEUTICAL APPENDIX TO THE TARIFF SCHEDULE 3 Table 1. This table enumerates products described by International Non-proprietary Names (INN) which shall be entered free of duty under general note 13 to the tariff schedule. The Chemical Abstracts Service (CAS) registry numbers also set forth in this table are included to assist in the identification of the products concerned. For purposes of the tariff schedule, any references to a product enumerated in this table includes such product by whatever name known. Product CAS No. Product CAS No. ABAMECTIN 65195-55-3 ACTODIGIN 36983-69-4 ABANOQUIL 90402-40-7 ADAFENOXATE 82168-26-1 ABCIXIMAB 143653-53-6 ADAMEXINE 54785-02-3 ABECARNIL 111841-85-1 ADAPALENE 106685-40-9 ABITESARTAN 137882-98-5 ADAPROLOL 101479-70-3 ABLUKAST 96566-25-5 ADATANSERIN 127266-56-2 ABUNIDAZOLE 91017-58-2 ADEFOVIR 106941-25-7 ACADESINE 2627-69-2 ADELMIDROL 1675-66-7 ACAMPROSATE 77337-76-9 ADEMETIONINE 17176-17-9 ACAPRAZINE 55485-20-6 ADENOSINE PHOSPHATE 61-19-8 ACARBOSE 56180-94-0 ADIBENDAN 100510-33-6 ACEBROCHOL 514-50-1 ADICILLIN 525-94-0 ACEBURIC ACID 26976-72-7 ADIMOLOL 78459-19-5 ACEBUTOLOL 37517-30-9 ADINAZOLAM 37115-32-5 ACECAINIDE 32795-44-1 ADIPHENINE 64-95-9 ACECARBROMAL 77-66-7 ADIPIODONE 606-17-7 ACECLIDINE 827-61-2 ADITEREN 56066-19-4 ACECLOFENAC 89796-99-6 ADITOPRIM 56066-63-8 ACEDAPSONE 77-46-3 ADOSOPINE 88124-26-9 ACEDIASULFONE SODIUM 127-60-6 ADOZELESIN 110314-48-2 ACEDOBEN 556-08-1 ADRAFINIL 63547-13-7 ACEFLURANOL 80595-73-9 ADRENALONE