LUCENTIS (Ranibizumab Injection) for Intravitreal Injection
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Intravenous Therapy Procedure Manual
INTRAVENOUS THERAPY PROCEDURE MANUAL - 1 - LETTER OF ACCEPTANCE __________________________________________ hereby approves (Facility) the attached Reference Manual as of _____________________. (Date) The Intravenous Therapy Procedure Manual will be reviewed at least annually or more often when deemed appropriate. Revisions will be reviewed as they occur. Current copies of the Intravenous Therapy Procedure Manual shall be maintained at each appropriate nursing station. I have reviewed this manual and agree to its approval. __________________________ (Administrator) __________________________ (Director of Nursing) __________________________ (Medical Director) - 2 - TABLE OF CONTENTS TABLE OF CONTENTS INTRODUCTION A. Purpose 1 B. Local Standard of Practice 1 RESPONSIBILITIES A. Responsibilities: M Chest Pharmacy 1 B. Responsibilities: Administrator 1 C. Responsibilities: Director of Nursing Services (DON/DNS) 1 D. Skills Validation 2 AMENDMENTS GUIDELINES A. Resident Candidacy for IV Therapy 1 B. Excluded IV Medications and Therapies 1 C. Processing the IV Order 1 D. IV Solutions/Medications: Storage 2 E. IV Solutions/Medications: Handling 3 F. IV Solutions and Supplies: Destroying and Returning 4 G. IV Tubing 5 H. Peripheral IV Catheters and Needles 6 I. Central Venous Devices 7 J. Documentation and Monitoring 8 K. IV Medication Administration Times 9 L. Emergency IV Supplies 10 I TABLE OF CONTENTS PROTOCOLS A. IV Antibiotic 1 1. Purpose 2. Guidelines 3. Nursing Responsibilities B. IV Push 2 1. Purpose 2. Guidelines C. Anaphylaxis Allergic Reaction 4 1. Purpose 2. Guidelines 3. Nursing Responsibilities and Interventions 4. Signs and Symptoms of Anaphylaxis 5. Drugs Used to Treat Anaphylaxis 6. Physician Protocol PRACTICE GUIDELINES A. Purpose 1 B. Personnel 1 C. Competencies 1 D. -

DRUGS REQUIRING PRIOR AUTHORIZATION in the MEDICAL BENEFIT Page 1
Effective Date: 08/01/2021 DRUGS REQUIRING PRIOR AUTHORIZATION IN THE MEDICAL BENEFIT Page 1 Therapeutic Category Drug Class Trade Name Generic Name HCPCS Procedure Code HCPCS Procedure Code Description Anti-infectives Antiretrovirals, HIV CABENUVA cabotegravir-rilpivirine C9077 Injection, cabotegravir and rilpivirine, 2mg/3mg Antithrombotic Agents von Willebrand Factor-Directed Antibody CABLIVI caplacizumab-yhdp C9047 Injection, caplacizumab-yhdp, 1 mg Cardiology Antilipemic EVKEEZA evinacumab-dgnb C9079 Injection, evinacumab-dgnb, 5 mg Cardiology Hemostatic Agent BERINERT c1 esterase J0597 Injection, C1 esterase inhibitor (human), Berinert, 10 units Cardiology Hemostatic Agent CINRYZE c1 esterase J0598 Injection, C1 esterase inhibitor (human), Cinryze, 10 units Cardiology Hemostatic Agent FIRAZYR icatibant J1744 Injection, icatibant, 1 mg Cardiology Hemostatic Agent HAEGARDA c1 esterase J0599 Injection, C1 esterase inhibitor (human), (Haegarda), 10 units Cardiology Hemostatic Agent ICATIBANT (generic) icatibant J1744 Injection, icatibant, 1 mg Cardiology Hemostatic Agent KALBITOR ecallantide J1290 Injection, ecallantide, 1 mg Cardiology Hemostatic Agent RUCONEST c1 esterase J0596 Injection, C1 esterase inhibitor (recombinant), Ruconest, 10 units Injection, lanadelumab-flyo, 1 mg (code may be used for Medicare when drug administered under Cardiology Hemostatic Agent TAKHZYRO lanadelumab-flyo J0593 direct supervision of a physician, not for use when drug is self-administered) Cardiology Pulmonary Arterial Hypertension EPOPROSTENOL (generic) -

Incidence and Management of Acute Endophthalmitis After Intravitreal
Eye (2009) 23, 2187–2193 & 2009 Macmillan Publishers Limited All rights reserved 0950-222X/09 $32.00 www.nature.com/eye Incidence and O Artunay, E Yuzbasioglu, R Rasier, A Sengu¨l CLINICAL STUDY and H Bahcecioglu management of acute endophthalmitis after intravitreal bevacizumab (Avastin) injection Abstract recognition and treatment are key in maximizing outcomes in patients who Introduction The aim of this study was to developed endophthalmitis after intravitreal report the incidence and management of acute injection of bevacizumab. endophthalmitis after intravitreal injection of Eye (2009) 23, 2187–2193; doi:10.1038/eye.2009.7; Avastin (bevacizumab), and visual acuity published online 13 February 2009 outcomes of three eyes of three patients who developed acute endophthalmitis following Keywords: intravitreal injection; bevacizumab; intravitreal injection of Avastin. endophthalmitis Methods This clinical retrospective, non-comparative study included 3022 Introduction intravitreal injections of 1.25 mg bevacizumab consecutively performed for 1822 eyes with Intravitreal injection of medications is becoming exudative age-related macular degeneration increasingly accepted for treatment of various and other retinal diseases. Of 3022 injections, retinal disorders, with effective intravitreal 1200 were reinjections. After clinical therapies being commonly administered in the appearance of post-injection endophthalmitis, vitreoretinal clinical or surgical environment. Department of immediate intervention was performed, With the increase in -

Injection Technique 1: Administering Drugs Via the Intramuscular Route
Copyright EMAP Publishing 2018 This article is not for distribution except for journal club use Clinical Practice Keywords Intramuscular injection/ Medicine administration/Absorption Practical procedures This article has been Injection technique double-blind peer reviewed Injection technique 1: administering drugs via the intramuscular route rugs administered by the intra- concerns that nurses are still performing Author Eileen Shepherd is clinical editor muscular (IM) route are depos- outdated and ritualistic practice relating to at Nursing Times. ited into vascular muscle site selection, aspirating back on the syringe Dtissue, which allows for rapid (Greenway, 2014) and skin cleansing. Abstract The intramuscular route allows absorption into the circulation (Dough- for rapid absorption of drugs into the erty and Lister, 2015; Ogston-Tuck, 2014). Site selection circulation. Using the correct injection Complications of poorly performed IM Four muscle sites are recommended for IM technique and selecting the correct site injection include: administration: will minimise the risk of complications. l Pain – strategies to reduce this are l Vastus lateris; outlined in Box 1; l Rectus femoris Citation Shepherd E (2018) Injection l Bleeding; l Deltoid; technique 1: administering drugs via l Abscess formation; l Ventrogluteal (Fig 1, Table 1). the intramuscular route. Nursing Times l Cellulitis; Traditionally the dorsogluteal (DG) [online]; 114: 8, 23-25. l Muscle fibrosis; muscle was used for IM injections but this l Injuries to nerves and blood vessels muscle is in close proximity to a major (Small, 2004); blood vessel and nerves, with sciatic nerve l Inadvertent intravenous (IV) access. injury a recognised complication (Small, These complications can be avoided if 2004). -

Endophthalmitis After Intravitreal Injections in Patients with Self-Reported Iodine Allergy
Endophthalmitis After Intravitreal Injections in Patients With Self-reported Iodine Allergy BOBECK S. MODJTAHEDI, TAVE´ VAN ZYL, HEMANG K. PANDYA, ROBERT E. LEONARD, II, AND DEAN ELIOTT PURPOSE: To present cases of endophthalmitis IMITING THE RISK OF POSTINJECTION ENDOPHTHAL- following intravitreal injections where povidone-iodine mitis is an area of considerable practical and aca- (PI) was not used as part of the surgical preparation. demic interest, especially in the era of regular L DESIGN: Retrospective case series. intravitreal injections. Although the incidence of postin- METHODS: All cases of presumed injection-related jection endophthalmitis is low (0.056% per injection in a endophthalmitis presenting to the Massachusetts Eye recent meta-analysis),1 the risk to an individual patient is and Ear Infirmary between June 2008 and November magnified by the recurrent nature of the procedure. Using 2014 and Dean McGee Eye Institute between January povidone-iodine (PI) for surgical antisepsis is well estab- 2010 and January 2015 were identified. Patients who lished and is the only preoperative measure shown to did not receive PI preparation owing to documented reduce the risk of endophthalmitis in patients undergoing self-reported allergy to iodine, iodine-containing contrast intraocular surgery.2 The importance of PI application material, or shellfish were identified and their injection prior to intravitreal injection has been observed by histories and clinical courses reviewed. Nentwich and associates,3 Bhavsar and Sandler,4 and Bryn- 5 RESULTS: The combined rate of postinjection endoph- skov and associates, the latter of whom described no cases thalmitis at these 2 centers was 0.019%. Among 42 of endophthalmitis after 20 293 injections. -

22428 Moxifloxacin Statisical PREA
U.S. Department of Health and Human Services Food and Drug Administration Center for Drug Evaluation and Research Office of Translational Science Office of Biostatistics S TATISTICAL R EVIEW AND E VALUATION CLINICAL STUDIES NDA/Serial Number: 22,428 Drug Name: Moxifloxacin AF (moxifloxacin hydrochloride ophthalmic solution) 0.5% Indication(s): Treatment of bacterial conjunctivitis Applicant: Alcon Pharmaceuticals, Ltd. Date(s): Letter date:21 May 2010; Filing date: 18 June, 2010; PDUFA goal date: 19 November 2010 Review Priority: Priority Biometrics Division: Anti-infective and Ophthalmology Products Statistical Reviewer: Mark. A. Gamalo, Ph.D. Concurring Reviewers: Yan Wang, Ph.D. Medical Division: Anti-infective and Ophthalmology Products Clinical Reviewer: Lucious Lim, M.D. Project Manager: Lori Gorski Keywords: superiority, Moxifloxacin hydrochloride ophthalmic solution, bacterial conjunctivitis, bulbar conjunctival injection, conjunctival discharge/exudate TABLE OF CONTENTS TABLE OF CONTENTS................................................................................................................ 2 LIST OF TABLES.......................................................................................................................... 3 1. EXECUTIVE SUMMARY ...................................................................................................... 4 1. 1 Conclusions and Recommendations..................................................................................... 4 1. 2 Brief Overview of Clinical Studies ..................................................................................... -

Intravitreal Angiogenesis Inhibitors for Retinal Vascular Conditions
MEDICAL COVERAGE GUIDELINES ORIGINAL EFFECTIVE DATE: 06/01/19 SECTION: DRUGS LAST REVIEW DATE: 04/16/19 LAST CRITERIA REVISION DATE: ARCHIVE DATE: LUCENTIS® (ranibizumab) for intravitreal injection Non-Discrimination Statement and Multi-Language Interpreter Services information are located at the end of this document. Coverage for services, procedures, medical devices and drugs are dependent upon benefit eligibility as outlined in the member's specific benefit plan. This Medical Coverage Guideline must be read in its entirety to determine coverage eligibility, if any. This Medical Coverage Guideline provides information related to coverage determinations only and does not imply that a service or treatment is clinically appropriate or inappropriate. The provider and the member are responsible for all decisions regarding the appropriateness of care. Providers should provide BCBSAZ complete medical rationale when requesting any exceptions to these guidelines. The section identified as “Description” defines or describes a service, procedure, medical device or drug and is in no way intended as a statement of medical necessity and/or coverage. The section identified as “Criteria” defines criteria to determine whether a service, procedure, medical device or drug is considered medically necessary or experimental or investigational. State or federal mandates, e.g., FEP program, may dictate that any drug, device or biological product approved by the U.S. Food and Drug Administration (FDA) may not be considered experimental or investigational and thus the drug, device or biological product may be assessed only on the basis of medical necessity. Medical Coverage Guidelines are subject to change as new information becomes available. For purposes of this Medical Coverage Guideline, the terms "experimental" and "investigational" are considered to be interchangeable. -
Intravitreal Injection Procedure Instructional Outline
Intravitreal Injection Procedure Instructional Outline Anh-Danh T. Phan, M.D. Indiana University School of Medicine Department of Ophthalmology Intravitreal Injection Procedure Instructional Outline Anh-Danh T. Phan, M.D. Assistant Professor of Ophthalmology Retina and Vitreous Service Indiana University School of Medicine Department of Ophthalmology / Glick Eye Institute Indianapolis, IN Email: [email protected] Background Statement: Intravitreal injection is the most common procedure in ophthalmology, yet carries associated risks. Mastery of the procedure particularly during residency training is critical to address the staggering patient treatment needs. Objectives: To transfer, along with accompanying instructional video, useful knowledge and skills for performing the intravitreal injection during ophthalmology training, enabling residents to understand: (1) the precautions before, during, and after the procedure, including risk of endophthalmitis; (2) the technique performed at a major university medical center; and (3) a method to standardize the procedure across multiple clinical settings. Residents are encouraged to gather instructional input from their supervising retinal specialists during training to develop their own procedural approach most comfortable, while observing the underlying principles and concepts outlined herein. Conflict of Interest The author has no propriety interest in either the outline or its subject matter. Legal Disclaimer The author provides this material for educational purposes only. It is not intended -
Informed Consent for Medication, Zyprexa
DEPARTMENT OF HEALTH SERVICES STATE OF WISCONSIN Division of Care and Treatment Services 42 CFR483.420(a)(2) F-24277 (09/2016) DHS 134.31(3)(o) DHS 94.03 & 94.09 §§ 51.61(1)(g) & (h) INFORMED CONSENT FOR MEDICATION Dosage and / or Side Effect information last revised on 04/16/2021 Completion of this form is voluntary. If not completed, the medication cannot be administered without a court order unless in an emergency. This consent is maintained in the client’s record and is accessible to authorized users. Name – Patient / Client (Last, First MI) ID Number Living Unit Date of Birth , Name – Individual Preparing This Form Name – Staff Contact Name / Telephone Number – Institution ANTICIPATED RECOMMENDED MEDICATION CATEGORY MEDICATION DOSAGE DAILY TOTAL DOSAGE RANGE RANGE Antipsychotic / Bipolar Agent Zyprexa oral tablet; Oral: 2.5 mg-50 mg with most doses in Zyprexa Zydis oral the 2.5 mg-20 mg range disintegrating tablet; IM: 5 mg-10 mg per dose, up to 3 doses Zyprexa Intramuscular 24 hours Injection; Long Acting Injectable: 150 mg-300 mg Zyprexa Relprevv IM every 2 weeks, Intramuscluar Injection 300 mg-405 mg IM every 4 weeks (olanzapine) The anticipated dosage range is to be individualized, may be above or below the recommended range but no medication will be administered without your informed and written consent. Recommended daily total dosage range of manufacturer, as stated in Physician’s Desk Reference (PDR) or another standard reference. This medication will be administered Orally Injection Other – Specify: 1. Reason for Use of Psychotropic Medication and Benefits Expected (note if this is ‘Off-Label’ Use) Include DSM-5 diagnosis or the diagnostic “working hypothesis.” 2. -

Product Monograph
PRODUCT MONOGRAPH Pr SANDOZ ONDANSETRON ODT Ondansetron Orally Disintegrating Tablets 4 mg and 8 mg ondansetron Manufacturer Standard Pr SANDOZ ONDANSETRON Ondansetron Tablets 4 mg and 8 mg ondansetron (as ondansetron hydrochloride dihydrate) Manufacturer Standard PrONDANSETRON INJECTION USP (ondansetron hydrochloride dihydrate) 2 mg/mL PrONDANSETRON HYDROCHLORIDE DIHYDRATE INJECTION Ondansetron Injection Manufacturer Standard 2 mg/mL Ondansetron (as ondansetron hydrochloride dihydrate) for injection Antiemetic (5-HT3-receptor antagonist) Sandoz Canada Inc. Date of Preparation: 145 Jules-Léger September 26, 2016 Boucherville, Québec, Canada J4B 7K8 Control No.: 198381 Ondansetron by Sandoz Page 1 of 43 Table of Contents PART I: HEALTH PROFESSIONAL INFORMATION .......................................................... 3 SUMMARY PRODUCT INFORMATION ................................................................................. 3 INDICATIONS AND CLINICAL USE ....................................................................................... 4 CONTRAINDICATIONS ............................................................................................................ 4 WARNINGS AND PRECAUTIONS .......................................................................................... 5 ADVERSE REACTIONS ............................................................................................................ 7 DRUG INTERACTIONS ............................................................................................................ -

July 1, 2020 RE: Physician Administered Drugs (J Codes)
July 1, 2020 RE: Physician Administered Drugs (J Codes) Included in Prior Authorization Matrix for Molina Healthcare of New York, Inc. Dear Participating Provider: Molina Healthcare of New York, Inc. requires prior authorization for these HCPCS codes for all participating providers. Prior authorization is required before services are rendered for the codes listed. Prior authorization requests should include the most up to date patient information including office notes, consultations, labs, scans, previous treatments tried, and any other patient specific information to support the request. Please fax a completed prior authorization form along with all supporting clinical documentation to fax number: 1-844- 823-5479. Our prior authorization form and most up to date formulary can be found on our website: MolinaHealthcare.com. C9061 INJECTION, TEPROTUMUMAB-TRBW, 10 mg C9063 INJECTION, EPTINEZUMAB-JJMR, 1 mg C9122 MOMETASONE FUROATE SINUS IMPLANT, 10 micrograms (sinuva) J0122 INJECTION, ERAVACYCLINE, 1 mg J0129 Injection, abatacept 10 mg J0178 Injection, aflibercept 1 mg J0179 INJECTION, BROLUCIZUMAB-DBLL, 1MG J0185 Injection, aprepitant 1 mg J0223 INJECTION, GIVOSIRAN, 0.5 mg J0285 INJECTION, AMPHOTERICIN B, 50 mg J0490 Injection, belimumab 10 mg J0517 Injection, benralizumab 1 mg J0567 Injection, cerliponase alfa 1 mg J0584 Injection, burosumab-twza 1 mg J0585 Injection, onabotulinumtoxina, 1 unit J0587 Injection, rimabotulinumtoxinb 100 units J0599 Injection, c-1 esterase inhibitor 10 units J0641 Injection, levoleucovorin, not otherwise -
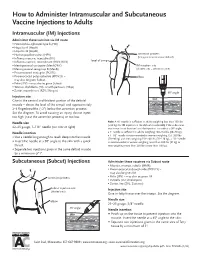
How to Administer Intramuscular and Subcutaneous Vaccines to Adults
How to Administer Intramuscular and Subcutaneous Vaccine Injections to Adults Intramuscular (IM) Injections Administer these vaccines via IM route • Haemophilus influenzae type b (Hib) • Hepatitis A (HepA) • Hepatitis B (HepB) • Human papillomavirus (HPV) acromion process (bony prominence above deltoid) • Influenza vaccine, injectable (IIV) • level of armpit • Influenza vaccine, recombinant (RIV3; RIV4) • Meningococcal conjugate (MenACWY) IM injection site • Meningococcal serogroup B (MenB) (shaded area = deltoid muscle) • Pneumococcal conjugate (PCV13) • Pneumococcal polysaccharide (PPSV23) – elbow may also be given Subcut • Polio (IPV) – may also be given Subcut • Tetanus, diphtheria (Td), or with pertussis (Tdap) • Zoster, recombinant (RZV; Shingrix) 90° angle Injection site skin Give in the central and thickest portion of the deltoid muscle – above the level of the armpit and approximately subcutaneous tissue 2–3 fingerbreadths (~2") below the acromion process. See the diagram. To avoid causing an injury, do not inject muscle too high (near the acromion process) or too low. Needle size Note: A ⅝" needle is sufficient in adults weighing less than 130 lbs (<60 kg) for IM injection in the deltoid muscle only if the subcutane- 22–25 gauge, 1–1½" needle (see note at right) ous tissue is not bunched and the injection is made at a 90° angle; Needle insertion a 1" needle is sufficient in adults weighing 130–152 lbs (60–70 kg); a 1–1½" needle is recommended in women weighing 153–200 lbs • Use a needle long enough to reach deep into the muscle. (70–90 kg) and men weighing 153–260 lbs (70–118 kg); a 1½" needle • Insert the needle at a 90° angle to the skin with a quick is recommended in women weighing more than 200 lbs (91 kg) or thrust.