1 RESPIRATORY DRUGS Lois E Brenneman, MSN, ANP, FNP, C
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Central Valley Toxicology Drug List
Chloroform ~F~ Lithium ~A~ Chlorpheniramine Loratadine Famotidine Acebutolol Chlorpromazine Lorazepam Fenoprofen Acetaminophen Cimetidine Loxapine Fentanyl Acetone Citalopram LSD (Lysergide) Fexofenadine 6-mono- Clomipramine acetylmorphine Flecainide ~M~ Clonazepam a-Hydroxyalprazolam Fluconazole Maprotiline Clonidine a-Hydroxytriazolam Flunitrazepam MDA Clorazepate Albuterol Fluoxetine MDMA Clozapine Alprazolam Fluphenazine Medazepam Cocaethylene Amantadine Flurazepam Meperidine Cocaine 7-Aminoflunitrazepam Fluvoxamine Mephobarbital Codeine Amiodarone Fosinopril Meprobamate Conine Amitriptyline Furosemide Mesoridazine Cotinine Amlodipine Methadone Cyanide ~G~ Amobarbital Methanol Cyclobenzaprine Gabapentin Amoxapine d-Methamphetamine Cyclosporine GHB d-Amphetamine l-Methamphetamine Glutethamide l-Amphetamine ~D~ Methapyrilene Guaifenesin Aprobarbital Demoxepam Methaqualone Atenolol Desalkylfurazepam ~H~ Methocarbamol Atropine Desipramine Halazepam Methylphenidate ~B~ Desmethyldoxepin Haloperidol Methyprylon Dextromethoraphan Heroin Metoclopramide Baclofen Diazepam Hexobarbital Metoprolol Barbital Digoxin Hydrocodone Mexiletine Benzoylecgonine Dihydrocodein Hydromorphone Midazolam Benzphetamine Dihydrokevain Hydroxychloroquine Mirtazapine Benztropine Diltiazem Hydroxyzine Morphine (Total/Free) Brodificoum Dimenhydrinate Bromazepam ~N~ Diphenhydramine ~I~ Bupivacaine Nafcillin Disopyramide Ibuprofen Buprenorphine Naloxone Doxapram Imipramine Bupropion Naltrexone Doxazosin Indomethacin Buspirone NAPA Doxepin Isoniazid Butabarbital Naproxen -

The New Face of Drug Abuse: Impact on Your Children, Family, and Community
The New Face of Drug Abuse: Impact on your Children, Family, and Community Patrick J. Sammon, Ph.D . [email protected] Impact of Prescription Drug Abuse: Illegal use of these drugs is responsible for multiple overdoses and fatalities Opiate addiction is blamed for causing a surge in crime: Robberies and break-ins at pharmacies Drug shoppers scamming doctors Harassments, assaults, and robberies of patients leaving drugstores Shoplifting and burglaries to support addiction Domestic violence and abuse Who’s at risk, who are the most vulnerable?: Adolescents - Sharp increase in 12 to 17 yr. olds and the 18 to 25 yr. olds Women - Increase rate of use in younger women Older adults - 17% of 60 + yr. olds may be affected by prescription drug abuse Why are Prescription Drugs so Popular? Legal, Easy to Obtain, Cheap and Safe & Non-addictive Legal: Perception that there is less legal risk than illicit drugs − Federal law does not distinguish between CI & CII drugs Easily obtainable: - From users, diverters, clinics, hospitals, Emergency Departments and practitioners and easy to steal Cheap: Low or no co-pay cost; may motivate people to use or sell PD’s Safer and Non-addictive: - Easily identity and less stigma than street drugs - Higher purity and less risky - Less HIV or hepatitis risk - Easier to use, no IV injecting but what about tolerance…and addiction! Commonly Misused and Abused Prescription & OTC Drugs Substance misuse is use of a drug that varies from a socially or medically accepted use. Substance abuse - any use of drugs that cause physical, psychological, economic, legal or social harm to the individual user or to others affected by the drug use's behavior. -

Estonian Statistics on Medicines 2016 1/41
Estonian Statistics on Medicines 2016 ATC code ATC group / Active substance (rout of admin.) Quantity sold Unit DDD Unit DDD/1000/ day A ALIMENTARY TRACT AND METABOLISM 167,8985 A01 STOMATOLOGICAL PREPARATIONS 0,0738 A01A STOMATOLOGICAL PREPARATIONS 0,0738 A01AB Antiinfectives and antiseptics for local oral treatment 0,0738 A01AB09 Miconazole (O) 7088 g 0,2 g 0,0738 A01AB12 Hexetidine (O) 1951200 ml A01AB81 Neomycin+ Benzocaine (dental) 30200 pieces A01AB82 Demeclocycline+ Triamcinolone (dental) 680 g A01AC Corticosteroids for local oral treatment A01AC81 Dexamethasone+ Thymol (dental) 3094 ml A01AD Other agents for local oral treatment A01AD80 Lidocaine+ Cetylpyridinium chloride (gingival) 227150 g A01AD81 Lidocaine+ Cetrimide (O) 30900 g A01AD82 Choline salicylate (O) 864720 pieces A01AD83 Lidocaine+ Chamomille extract (O) 370080 g A01AD90 Lidocaine+ Paraformaldehyde (dental) 405 g A02 DRUGS FOR ACID RELATED DISORDERS 47,1312 A02A ANTACIDS 1,0133 Combinations and complexes of aluminium, calcium and A02AD 1,0133 magnesium compounds A02AD81 Aluminium hydroxide+ Magnesium hydroxide (O) 811120 pieces 10 pieces 0,1689 A02AD81 Aluminium hydroxide+ Magnesium hydroxide (O) 3101974 ml 50 ml 0,1292 A02AD83 Calcium carbonate+ Magnesium carbonate (O) 3434232 pieces 10 pieces 0,7152 DRUGS FOR PEPTIC ULCER AND GASTRO- A02B 46,1179 OESOPHAGEAL REFLUX DISEASE (GORD) A02BA H2-receptor antagonists 2,3855 A02BA02 Ranitidine (O) 340327,5 g 0,3 g 2,3624 A02BA02 Ranitidine (P) 3318,25 g 0,3 g 0,0230 A02BC Proton pump inhibitors 43,7324 A02BC01 Omeprazole -

Ied with Great Restlessness
excessive discharge from the bowels. Subsultus tendinum plete publicity lies with Ayer; whether correctly or not, the in the terminal stage of the disease is usually accompan- quantities are all given. AYER'S rECTORAL. PRUNI-HEEOIN. ied with for which in recent cases I CHERRY great restlessness; Each auid ounce1 represents Each fluid ounce represents have found Hoffman's as recommended Wild cherry .6 grains. Wild cherry bark. anodyne, by White pine .4 White bark. a grains. pine Hare, very useful remedy. Terpin hydrate. .. .4 grains. Terpin hydrate.4 grains. In the later of the feeble heart's Blood root .2 grains. Blood root. stage typhoid fever, Heroin ( !).1/6 grain. Heroin .1/6 grain. action calls for and one must instruct the Grindella rohusta. .4 grains. Ammon muriate. .16 grains. support; Senega .4 grains. Spikenard. nurse relative to the necessary stimulants to sustain the Rio Ipecac .2 grains. Glycerin. circulation. the urine is loaded Glycerin. Solvents. During convalescence Alcohol .80 m. etc. with the bacillus. in 5- Syrup. typhoid Hexamethylenamin Water. three times a well diluted with grain doses, repeated day, If Ayer's "shotgun" Pectoral ought "to be considered obso- and continued for a week or ten will water, days, destroy lete, what shall we say of Pruni-Heroin? If a pre- the bacillus in urine. physician the scribe Pruni-Heroin and condemn Ayer's to a patient who has taken Ayer's, what will the patient think of the advice if he learns the of composition Pruni-Heroin? _ Expectorants in the Pharmocopeia. THE PHYSICIAN AND THE PHARMACOPEIA. -

Pharmaceutical Preparations, Except Biologicals (Manufacturers)
CURRENT INDUSTRIAL REPORTS 2006 MA325G — PHARMACEUTICAL PREPARATIONS, EXCEPT BIOLOGICALS (MANUFACTURERS) DEFINITIONS AND SPECIAL INSTRUCTIONS 1. Scope of survey Products bought and resold without further manufacture should not be included in shipments. This survey covers manufacturers of pharmaceutical preparations, except biologicals, in the United States, Establishments shipping dosage forms, in bulk and and includes all preparations which can be dispensed requiring repackaging, to other establishments of the in measured portions to produce the therapeutic effect same company, should report in column (4) a transfer for which the preparation is most commonly employed value reflecting only services or operations performed (liquids, tablets, pills, capsules, lozenges, powders, including profit (or loss) normally assigned to the ointments, jellies, salves, inhaler tubes, etc.). Products manufacturing establishment. For plants shipping manufactured in Puerto Rico or other U.S. possessions similar products to other companies for repackaging should be excluded. report in column (4) dosage forms shipped in bulk at net sales value as defined above. 2. Figures to be reported Commercial shipments (packaged for consumer use) Companies with more than one establishment Report the value of each drug product produced manufacturing the products covered by this survey are in dosage form, packaged for consumer use and requested to complete a separate report form for each shipped from this establishment to sales branches, location. If you have not received a separate form for warehouses of your company, wholesale or retail each of your establishments, please call the contact stores, and other commercial customers such as listed on the report form or write to the U.S. Census hospitals, institutions, etc. -

National OTC Medicines List-2018
National OTC Medicines List – First Edition 2018 NATIONAL OTC MEDICINES LIST First Edition 2018 Foreword According to the French National Agency for Medicines and Health Products Safety (ANSM), Over‐the‐ counter (OTC) drugs are medicines that are accessible to patients in pharmacies, based on criteria set to safeguard patients’ safety. FDA’s Center for Drug Evaluation and Research (CDER) regulates over‐the‐counter (OTC) which are drugs that have been found to be safe and appropriate for use without the supervision of a health care professional such as a physician, and they can be purchased by consumers without a prescription. Due to their therapeutic class, these medicines could be dispensed without physician’s intervention for diagnostic, treatment initiation or maintenance purposes. According to Arcle 43 of the Law No.367 issued in 1994 related to the pharmacy practice, and the amendment of Arcles 46 and 47 by Law No.91 issued in 2010, pharmacists do not have the right to dispense any medicine that is not requested through a unified prescription, unless the medicine is mentioned in a list which is established by the Orders of Pharmacists and Physicians In this regards, the Ministry of Public Health (MoPH) developed the National OTC list, presented it in a scientific, objective, reliable and accessible listingand issued by a Ministerial decision. At this stage, no “convenience size packaging” nor “restriction to a maximum dose” or a “maximum dose per day” or “length of treatment” were considered for some molecules to allow them to be classified as OTC. The list covers medicines that are intended to relief patients from minor to moderate symptoms for a determined period, and procured with the pharmacist’s assistance without the physician’s intervention. -

1 Chapter 6800 Board of Pharmacy Pharmacies and Pharmacists
1 CHAPTER 6800 BOARD OF PHARMACY PHARMACIES AND PHARMACISTS 6800.0100 DEFINITIONS. 6800.0110 RESPONSIBILITY FOR ACTION BY A PHARMACY. LICENSING PHARMACIES 6800.0200 FORM OF APPLICATION AND LICENSE. 6800.0300 PHARMACY LICENSE AND FEE REQUIRED. 6800.0350 LICENSE CATEGORIES. 6800.0400 ANNUAL LICENSE RENEWAL DATE AND FEES. 6800.0500 SEPARATE LICENSE REQUIRED. 6800.0600 POSTING LICENSE. 6800.0700 PHARMACY, SPACE, AND SECURITY. 6800.0800 LOCATION, DIMENSION, OR SECURITY CHANGES. 6800.0910 PATIENT ACCESS TO PHARMACIST. 6800.0950 REQUIREMENT FOR A SUPERVISED PHARMACY AREA. 6800.1010 CLOSING A PHARMACY. 6800.1050 REQUIRED REFERENCE BOOKS AND EQUIPMENT. LICENSING PHARMACISTS 6800.1150 ANNUAL RENEWAL, FEES, AND POSTING. 6800.1210 INACTIVE STATUS AND EMERITUS LICENSE. 6800.1250 APPLICATIONS FOR LICENSURE. 6800.1300 LICENSURE TRANSFER (RECIPROCITY). LICENSING MANUFACTURERS AND WHOLESALERS 6800.1400 DRUG MANUFACTURER OR WHOLESALER LICENSE. 6800.1410 MINIMUM INFORMATION REQUIRED FOR LICENSURE. 6800.1420 MINIMUM QUALIFICATIONS. 6800.1430 PERSONNEL. 6800.1440 REQUIREMENTS FOR WHOLESALE DRUG DISTRIBUTORS. 6800.1460 MANUFACTURING PROCEDURES. CONTINUING EDUCATION 6800.1500 CONTINUING EDUCATION. 6800.1600 CONTINUING EDUCATION ADVISORY TASK FORCE. OPERATION OF PHARMACIES 6800.2150 PHARMACIST ON DUTY. 6800.2250 UNPROFESSIONAL CONDUCT. 6800.2300 SANITATION. 6800.2350 PHARMACEUTICAL WASTE. 6800.2400 PHARMACIST-IN-CHARGE. Copyright ©2013 by the Revisor of Statutes, State of Minnesota. All Rights Reserved. PHARMACIES AND PHARMACISTS 2 6800.2500 CHANGE OF BUSINESS OR RESIDENCE ADDRESS. 6800.2600 AUTOMATED COUNTING AND DISTRIBUTION. 6800.2700 RETURN OF DRUGS AND DEVICES. 6800.2900 PRESCRIPTION BLANKS. 6800.3000 PRESCRIPTIONS AND DISTRIBUTION OF DRUGS. 6800.3100 COMPOUNDING AND DISPENSING. 6800.3110 PATIENT MEDICATION PROFILES. 6800.3120 TRANSFER OF PRESCRIPTIONS BETWEEN PHARMACIES. -

ED227273.Pdf
DOCUMENT RESUft ED 227 273 y CE 035 300 ' TITLE APharmacy Spicialist, Militkry Curriculum Materials for Vocation47 andileChlaical Education. INSTITuTION Air Force Training Command, Sheppa* AFB, Tex.; Ohio State Univ., Columbus. Natfonal Center for Research in Vocational Education. SPONS AGENCY Office of Education (DHEW)x Washington, D.C. PUB DATE 18 Jul 75 NOTE 774p.; Some pages are marginally legible. ,PUB TYPE Guides - Classroom Use Guides (For Teachers) (052), , EDRS ?RICE 14P05/PC31 Plus Postage. ` DESCRIPTORS Behavioral Objectives; Course Descriptions; A Curriculum Guides; Drug Abuse; Drug,Therapy; 4Drug Use; Learning Activities; Lesson Plans; *Pharmaceutical Education; Pharmacists; *Pharmacology; *Pharmacy; Postsecondary Education; Programed Instructional Materials; Textbooks; Workbooks IDENTIFIERS. Military CuFr.iculum Project liBSTRACT These teacher and studdnt,materials for a . postsecondary-level course in pharmacy comprise one of a numberof military-developed curriculum packages selected for adaptation to voCational instruction 'and curriculum dei7elopment in acivilian setting. The purpose stated for the 256-hour course iS totrain students in the basic technical phases of pharmacy and theminimum essential knowledge and skills necessaryior.the compounding and - dispensing of drugs, the economical operation of a pharmacy,and the proper use of drugs, chemicals, andbiological products. The course consists of three blocks of instruction. Block I contains four, lessons: pharmaceutical calculations I and laboratory,inorganic chemistry, and organic chemistry. The five lessons in Block II cover anatomy ,and physiology, introduction topharmacoloe, toxicology, drug abuse, and pharmaceutical and medicinal agents. Block III provides five lessons: phdrmaceutical calculations\I and II, techniques"of pharmaceutical compounding, pharmaceutiCal dosage for s, and compounding laboratbry. Instructormaterials include a cb se chart, lesson plans, and aplan of instruction detailing instructional,bnits, criterion objectives, lesson duration,and support materials needed. -

Benefit/Risk Assessment of Prescription Opioid Antitussive Products for Treatment of Cough in Pediatric Patients
Background Document Pediatric Advisory Committee Meeting September 11, 2017 Benefit/Risk Assessment of Prescription Opioid Antitussive Products for Treatment of Cough in Pediatric Patients Table of Contents 1. Introduction ..........................................................................................................................................2 2. Regulatory History of Prescription Opioid Antitussive Products .......................................................... 3 Codeine ..................................................................................................................................................... 3 Hydrocodone............................................................................................................................................. 5 Pediatric Study Requirements for Prescription Opioid Antitussives ........................................................ 8 3. Safety of Opioid Antitussive Products among Children and Adolescents ............................................ 9 Codeine and Risk of Respiratory Depression and Death Due to Ultra‐rapid Metabolism........................9 Hydrocodone and Risk of Respiratory Depression and Death................................................................ 12 Risks of misuse, abuse, addiction, overdose and death with opioid antitussives .................................. 13 4. Utilization of Products to Treat Cough in Pediatric Patients .............................................................. 14 5. Treatment Alternatives for Cough -
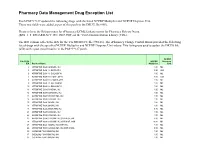
Pharmacy Data Management Drug Exception List
Pharmacy Data Management Drug Exception List Patch PSS*1*127 updated the following drugs with the listed NCPDP Multiplier and NCPDP Dispense Unit. These two fields were added as part of this patch to the DRUG file (#50). Please refer to the Release notes for ePharmacy/ECME Enhancements for Pharmacy Release Notes (BPS_1_5_EPHARMACY_RN_0907.PDF) on the VistA Documentation Library (VDL). The IEN column reflects the IEN for the VA PRODUCT file (#50.68). The ePharmacy Change Control Board provided the following list of drugs with the specified NCPDP Multiplier and NCPDP Dispense Unit values. This listing was used to update the DRUG file (#50) with a post install routine in the PSS*1*127 patch. NCPDP File 50.68 NCPDP Dispense IEN Product Name Multiplier Unit 2 ATROPINE SO4 0.4MG/ML INJ 1.00 ML 3 ATROPINE SO4 1% OINT,OPH 3.50 GM 6 ATROPINE SO4 1% SOLN,OPH 1.00 ML 7 ATROPINE SO4 0.5% OINT,OPH 3.50 GM 8 ATROPINE SO4 0.5% SOLN,OPH 1.00 ML 9 ATROPINE SO4 3% SOLN,OPH 1.00 ML 10 ATROPINE SO4 2% SOLN,OPH 1.00 ML 11 ATROPINE SO4 0.1MG/ML INJ 1.00 ML 12 ATROPINE SO4 0.05MG/ML INJ 1.00 ML 13 ATROPINE SO4 0.4MG/0.5ML INJ 1.00 ML 14 ATROPINE SO4 0.5MG/ML INJ 1.00 ML 15 ATROPINE SO4 1MG/ML INJ 1.00 ML 16 ATROPINE SO4 2MG/ML INJ 1.00 ML 18 ATROPINE SO4 2MG/0.7ML INJ 0.70 ML 21 ATROPINE SO4 0.3MG/ML INJ 1.00 ML 22 ATROPINE SO4 0.8MG/ML INJ 1.00 ML 23 ATROPINE SO4 0.1MG/ML INJ,SYRINGE,5ML 5.00 ML 24 ATROPINE SO4 0.1MG/ML INJ,SYRINGE,10ML 10.00 ML 25 ATROPINE SO4 1MG/ML INJ,AMP,1ML 1.00 ML 26 ATROPINE SO4 0.2MG/0.5ML INJ,AMP,0.5ML 0.50 ML 30 CODEINE PO4 30MG/ML -

Bulk Drug Substances Nominated for Use in Compounding Under Section 503B of the Federal Food, Drug, and Cosmetic Act
Updated June 07, 2021 Bulk Drug Substances Nominated for Use in Compounding Under Section 503B of the Federal Food, Drug, and Cosmetic Act Three categories of bulk drug substances: • Category 1: Bulk Drug Substances Under Evaluation • Category 2: Bulk Drug Substances that Raise Significant Safety Risks • Category 3: Bulk Drug Substances Nominated Without Adequate Support Updates to Categories of Substances Nominated for the 503B Bulk Drug Substances List1 • Add the following entry to category 2 due to serious safety concerns of mutagenicity, cytotoxicity, and possible carcinogenicity when quinacrine hydrochloride is used for intrauterine administration for non- surgical female sterilization: 2,3 o Quinacrine Hydrochloride for intrauterine administration • Revision to category 1 for clarity: o Modify the entry for “Quinacrine Hydrochloride” to “Quinacrine Hydrochloride (except for intrauterine administration).” • Revision to category 1 to correct a substance name error: o Correct the error in the substance name “DHEA (dehydroepiandosterone)” to “DHEA (dehydroepiandrosterone).” 1 For the purposes of the substance names in the categories, hydrated forms of the substance are included in the scope of the substance name. 2 Quinacrine HCl was previously reviewed in 2016 as part of FDA’s consideration of this bulk drug substance for inclusion on the 503A Bulks List. As part of this review, the Division of Bone, Reproductive and Urologic Products (DBRUP), now the Division of Urology, Obstetrics and Gynecology (DUOG), evaluated the nomination of quinacrine for intrauterine administration for non-surgical female sterilization and recommended that quinacrine should not be included on the 503A Bulks List for this use. This recommendation was based on the lack of information on efficacy comparable to other available methods of female sterilization and serious safety concerns of mutagenicity, cytotoxicity and possible carcinogenicity in use of quinacrine for this indication and route of administration. -

Estonian Statistics on Medicines 2013 1/44
Estonian Statistics on Medicines 2013 DDD/1000/ ATC code ATC group / INN (rout of admin.) Quantity sold Unit DDD Unit day A ALIMENTARY TRACT AND METABOLISM 146,8152 A01 STOMATOLOGICAL PREPARATIONS 0,0760 A01A STOMATOLOGICAL PREPARATIONS 0,0760 A01AB Antiinfectives and antiseptics for local oral treatment 0,0760 A01AB09 Miconazole(O) 7139,2 g 0,2 g 0,0760 A01AB12 Hexetidine(O) 1541120 ml A01AB81 Neomycin+Benzocaine(C) 23900 pieces A01AC Corticosteroids for local oral treatment A01AC81 Dexamethasone+Thymol(dental) 2639 ml A01AD Other agents for local oral treatment A01AD80 Lidocaine+Cetylpyridinium chloride(gingival) 179340 g A01AD81 Lidocaine+Cetrimide(O) 23565 g A01AD82 Choline salicylate(O) 824240 pieces A01AD83 Lidocaine+Chamomille extract(O) 317140 g A01AD86 Lidocaine+Eugenol(gingival) 1128 g A02 DRUGS FOR ACID RELATED DISORDERS 35,6598 A02A ANTACIDS 0,9596 Combinations and complexes of aluminium, calcium and A02AD 0,9596 magnesium compounds A02AD81 Aluminium hydroxide+Magnesium hydroxide(O) 591680 pieces 10 pieces 0,1261 A02AD81 Aluminium hydroxide+Magnesium hydroxide(O) 1998558 ml 50 ml 0,0852 A02AD82 Aluminium aminoacetate+Magnesium oxide(O) 463540 pieces 10 pieces 0,0988 A02AD83 Calcium carbonate+Magnesium carbonate(O) 3049560 pieces 10 pieces 0,6497 A02AF Antacids with antiflatulents Aluminium hydroxide+Magnesium A02AF80 1000790 ml hydroxide+Simeticone(O) DRUGS FOR PEPTIC ULCER AND GASTRO- A02B 34,7001 OESOPHAGEAL REFLUX DISEASE (GORD) A02BA H2-receptor antagonists 3,5364 A02BA02 Ranitidine(O) 494352,3 g 0,3 g 3,5106 A02BA02 Ranitidine(P)