Parasitic Diseases with Cutaneous Manifestations
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Trichinosis (Trichinellosis) Case Reporting and Investigation Protocol
Wisconsin Department of Health Services Division of Public Health P-01912 (Rev 08/2017) Communicable Disease Case Reporting and Investigation Protocol TRICHINOSIS (TRICHINELLOSIS) I. IDENTIFICATION AND DEFINITION OF CASES A. Clinical Description: A parasitic disease caused by ingestion of Trichinella species larvae. The disease causes a variety of clinical manifestations. Common signs and symptoms among symptomatic persons include eosinophilia, fever, myalgia, and periorbital edema. B. Laboratory Criteria: Confirmatory laboratory evidence: • Demonstration of Trichinella larvae on muscle biopsy, OR • A positive serology for Trichinella. C. Wisconsin Surveillance Case Definition: A clinically compatible illness that is laboratory confirmed. NOTE: In an outbreak setting, at least one case must be laboratory confirmed. Associated cases are considered confirmed if the patient shared an epidemiologically implicated meal or ate an epidemiologically implicated meat product and has either a positive serology for trichinosis or a clinically compatible illness. II. REPORTING A. Wisconsin Disease Surveillance Category II – Methods for Reporting: This disease shall be reported to the patient’s local health officer or to the local health officer’s designee within 72 hours of recognition of a case or suspected case, per Wis. Admin. Code § DHS 145.04 (3) (b). Report electronically through the Wisconsin Electronic Disease Surveillance System (WEDSS), or mail or fax a completed Acute and Communicable Disease Case Report (F-44151) to the address on the form. B. Responsibility for Reporting: According to Wis. Admin. Code § DHS 145.04(1), persons licensed under Wis. Stat. ch. 441 or 448, laboratories, health care facilities, teachers, principals, or nurses serving a school or day care center, and any person who knows or suspects that a person has a communicable disease identified in Appendix A. -

Bulletin Leading the Fight Against Heartworm Disease
BULLETIN LEADING THE FIGHT AGAINST HEARTWORM DISEASE SEPTEMBER HEARTWORM 2017 Q&A VOLUME 44 No. 3 Heartworm History: In What Year Was Heartworm First INSIDE THIS ISSUE Treated? Page 4 From the President Page 8 Research Update Abstracts from the Literature Page 14 Heartworm Hotline: Role of Heat Treatment in Diagnostics Page 19 NEW! Best Practices: Minimizing Heartworm Transmission in Relocated Dogs uestions from members, prac- published in the 1998 AHS Symposium 1 titioners, technicians, and the Proceedings. Dr. Roncalli wrote, “The Page 21 Qgeneral public are often submit- first trial to assess the efficacy of a Welcome Our New AHS ted to the American Heartworm Society microfilaricide (natrium antimonyl tar- Student Liaisons (AHS) via our website. Two of our AHS trate) was conducted some 70 years Board members, Dr. John W.McCall and ago (1927) in Japan by S. Itagaki and R. Page 25 Dr. Tom Nelson, provided the resources Makino.2 Fuadin (stibophen), a trivalent In the News: Surgeons to answer this question: In What Year antimony compound, was tested, intra- Remove a Heartworm from Was Heartworm First Treated? venously, as a microfilaricide by Popescu the Femoral Artery of a Cat The first efforts to treat canine heart- in 1933 in Romania and by W.H. Wright worm disease date back to the 1920s. Dr. and P.C. Underwood in 1934 in the USA. Page 26 Nelson referenced a review article by Dr. In 1949, I.C. Mark evaluated its use Quarterly Update Raffaele Roncalli, “Tracing the History of intraperitoneally.” What’s New From AHS? Heartworms: A 400 Year Perspective,” Continues on page 7 American Heartworm Society / PO Box 8266, Wilmington, DE 19803-8266 Become an American Heartworm Society www.heartwormsociety.org / [email protected] fan on Facebook! Follow us on Twitter! OUR GENEROUS SPONSORS PLATINUM LEVEL PO Box 8266 Wilmington, DE 19803-8266 [email protected] www.heartwormsociety.org Mission Statement The mission of the American Heartworm Society is to lead the vet- erinary profession and the public in the understanding of heartworm disease. -

Effectiveness of Neem Oil Upon Pediculosis
EFFECTIVENESS OF NEEM OIL UPON PEDICULOSIS By LINCY ISSAC A DISSERTATION SUBMITTED TO THE TAMILNADU DR.M.G.R.MEDICAL UNIVERSITY, CHENNAI, IN PARTIAL FULFILMENT OF THE REQUIREMENTS FOR THE DEGREE OF MASTER OF SCIENCE IN NURSING MARCH 2011 EFFECTIVENESS OF NEEM OIL UPON PEDICULOSIS Approved by the dissertation committee on :__________________________ Research Guide : __________________________ Dr. Latha Venkatesan M.Sc., (N), M.Phil., Ph.D., Principal and Professor in Nursing Apollo College of Nursing, Chennai -600 095 Clinical Guide : __________________________ Mrs. Shobana Gangadharan M.Sc., (N), Professor Community Health Nursing Apollo College of Nursing, Chennai -600 095. Medical Guide : __________________________ Dr.Mathrubootham Sridhar M.R.C.P.C.H.(Paed)., Consultant –Paediatrician, Apollo Childrens Hospitals, Chennai -600 006 A DISSERTATION SUBMITTED TO THE TAMILNADU DR.M.G.R.MEDICAL UNIVERSITY, CHENNAI, IN PARTIAL FULFILMENT OF THE REQUIREMENTS FOR THE DEGREE OF MASTER OF SCIENCE IN NURSING MARCH 2011 DECLARATION I hereby declare that the present dissertation entitled “Effectiveness Of Neem Oil Upon Pediculosis” is the outcome of the original research work undertaken and carried out by me, under the guidance of Dr.Latha Venkatesan., M.Sc (N)., M.Phil., Ph.D., Principal and Mrs.Shobana G, M.Sc (N)., Professor, Community Health Nursing, Apollo College Of Nursing, Chennai. I also declare that the material of this has not formed in anyway, the basis for the award of any degree or diploma in this University or any other Universities. ACKNOWLEDGEMENT I thank God Almighty for being with me and guiding me throughout my Endeavour and showering His profuse blessings in each and every step to complete the dissertation. -

First Case of Furuncular Myiasis Due to Cordylobia Anthropophaga in A
braz j infect dis 2 0 1 8;2 2(1):70–73 The Brazilian Journal of INFECTIOUS DISEASES www.elsevi er.com/locate/bjid Case report First case of Furuncular Myiasis due to Cordylobia anthropophaga in a Latin American resident returning from Central African Republic a b a c a,∗ Jóse A. Suárez , Argentina Ying , Luis A. Orillac , Israel Cedeno˜ , Néstor Sosa a Gorgas Memorial Institute, City of Panama, Panama b Universidad de Panama, Departamento de Parasitología, City of Panama, Panama c Ministry of Health of Panama, International Health Regulations, Epidemiological Surveillance Points of Entry, City of Panama, Panama a r t i c l e i n f o a b s t r a c t 1 Article history: Myiasis is a temporary infection of the skin or other organs with fly larvae. The lar- Received 7 November 2017 vae develop into boil-like lesions. Creeping sensations and pain are usually described by Accepted 22 December 2017 patients. Following the maturation of the larvae, spontaneous exiting and healing is expe- Available online 2 February 2018 rienced. Herein we present a case of a traveler returning from Central African Republic. She does not recall insect bites. She never took off her clothing for recreational bathing, nor did Keywords: she visit any rural areas. The lesions appeared on unexposed skin. The specific diagnosis was performed by morphologic characterization of the larvae, resulting in Cordylobia anthro- Cordylobia anthropophaga Furuncular myiasis pophaga, the dominant form of myiasis in Africa. To our knowledge, this is the first reported Tumbu-fly case of C. -
Computational Studies of Drug Repurposing Targeting P-Glycoprotein Mediated Multidrug-Resistance Phenotypes in Agents of Neglect
bioRxiv preprint doi: https://doi.org/10.1101/2020.06.12.147926; this version posted June 12, 2020. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY 4.0 International license. Computational studies of drug repurposing targeting P- glycoprotein mediated multidrug-resistance phenotypes in agents of neglected tropical diseases Nivedita Jaishankar 1, Sangeetha Muthamilselvan 2, Ashok Palaniappan 1,2* 1 Department of Biotechnology, Sri Venkateswara College of Engineering, Post Bag No. 1, Pennalur, Sriperumbudur Tk 602117. India 2 Department of Bioinformatics, School of Chemical and BioTechnology, SASTRA Deemed University, Thanjavur 613401. India * Corresponding author: [email protected] ABSTRACT Mammalian ABCB1 P-glycoprotein is an ATP- dependent efflux pump with broad substrate specificity associated with cellular drug resistance. Homologous to this role in mammalian biology, the P-glycoprotein of agents of neglected tropical diseases (NTDs) mediates the emergence of multidrug- resistance phenotypes. The clinical and socioeconomic implications of NTDs are exacerbated by the lack of research interest among Big Pharma for treating such conditions. This work aims to characterise P-gp homologues in certain agents of key NTDs, namely (1) Protozoa: Leishmania major, Trypanosoma cruzi; (2) Helminths: Onchocerca volvulus, Schistosoma mansoni. PSI-BLAST searches against the genome of each of these organisms confirmed the presence of P-gp homologues. Each homologue was aligned against five P- gp sequences of known structure, to identify the most suitable template based on sequence homology, phylogenetic nearest neighbor, and query coverage. -

Onchocerciasis
11 ONCHOCERCIASIS ADRIAN HOPKINS AND BOAKYE A. BOATIN 11.1 INTRODUCTION the infection is actually much reduced and elimination of transmission in some areas has been achieved. Differences Onchocerciasis (or river blindness) is a parasitic disease in the vectors in different regions of Africa, and differences in cause by the filarial worm, Onchocerca volvulus. Man is the the parasite between its savannah and forest forms led to only known animal reservoir. The vector is a small black fly different presentations of the disease in different areas. of the Simulium species. The black fly breeds in well- It is probable that the disease in the Americas was brought oxygenated water and is therefore mostly associated with across from Africa by infected people during the slave trade rivers where there is fast-flowing water, broken up by catar- and found different Simulium flies, but ones still able to acts or vegetation. All populations are exposed if they live transmit the disease (3). Around 500,000 people were at risk near the breeding sites and the clinical signs of the disease in the Americas in 13 different foci, although the disease has are related to the amount of exposure and the length of time recently been eliminated from some of these foci, and there is the population is exposed. In areas of high prevalence first an ambitious target of eliminating the transmission of the signs are in the skin, with chronic itching leading to infection disease in the Americas by 2012. and chronic skin changes. Blindness begins slowly with Host factors may also play a major role in the severe skin increasingly impaired vision often leading to total loss of form of the disease called Sowda, which is found mostly in vision in young adults, in their early thirties, when they northern Sudan and in Yemen. -

Artrópodos Como Agentes De Enfermedad
DEPARTAMENTO DE PARASITOLOGIA Y MICOLOGIA INVERTEBRADOS, CELOMADOS, CON SEGMENTACIÓN EXTERNA, PATAS Y APÉNDICES ARTICULADOS EXOESQUELETO QUITINOSO TUBO DIGESTIVO COMPLETO, APARATO CIRCULATORIO Y EXCRETOR ABIERTO. RESPIRACIÓN TRAQUEAL EL TIPO INTEGRA LAS CLASES DE IMPORTANCIA MÉDICA COMO AGENTES: ARACHNIDA, INSECTA CHILOPODA DIOCOS, CON FRECUENTE DIMORFISMO SEXUAL CICLOS EVOLUTIVOS DE VARIABLE COMPLEJIDAD (HUEVOS, LARVAS, NINFAS, ADULTOS). INSECTA. CARACTERES GENERALES. LA CLASE INTEGRA CON IMPORTANCIA MEDICA COMO AGENTES: PARÁSITOS, MICROPREDADORES E INOCULADORES DE PONZOÑA. CUERPO DIVIDIDO EN CABEZA, TÓRAX Y ABDOMEN APARATO BUCAL DE DIFERENTE TIPO. RESPIRACIÓN TRAQUEAL TRES PARES DE PATAS PRESENCIA DE ALAS Y ANTENAS METAMORFOSIS DE COMPLEJIDAD VARIABLE ARACHNIDA. CARACTERES GENERALES. LA CLASE INTEGRA CON IMPORTANCIA MEDICA COMO AGENTES ARAÑAS, ESCORPIONES, GARRAPATAS Y ÁCAROS. CUERPO DIVIDIDO EN CEFALOTÓRAX Y ABDOMEN. DIFERENTES TIPOS DE APÉNDICES PREORALES RESPIRACIÓN TRAQUEAL EN LA MAYORÍA CUATRO PARES DE PATAS PRESENCIA DE GLÁNDULA VENENOSAS EN MUCHOS. SIN ALAS Y SIN ANTENAS AGENTE CAUSA O ETIOLOGÍA DIRECTA DE UNA AFECCIÓN. ARTRÓPODOS COMO AGENTES DE ENFERMEDAD: *ARÁCNIDOS (ÁCAROS, ARAÑAS, ESCORPIONES) *MIRIÁPODOS (CIEMPIÉS, ESCOLOPENDRAS) *INSECTOS (PIOJOS, LARVAS DE MOSCAS, ABEJAS, ETC.) TIPOS DE AGENTES NOSOLÓGICOS : - PARÁSITOS (LARVAS O ADULTOS) - MICROPREDADORES - PONZOÑOSOS - ALERGENOS DESARROLLO DE PARASITISMO: - ECTOPARÁSITOS - MIASIS INOCULACIÓN O CONTAMINACIÓN CON PONZOÑAS (TÓXICOS ELABORADOS POR SERES VIVOS). -

Arthropod Parasites in Domestic Animals
ARTHROPOD PARASITES IN DOMESTIC ANIMALS Abbreviations KINGDOM PHYLUM CLASS ORDER CODE Metazoa Arthropoda Insecta Siphonaptera INS:Sip Mallophaga INS:Mal Anoplura INS:Ano Diptera INS:Dip Arachnida Ixodida ARA:Ixo Mesostigmata ARA:Mes Prostigmata ARA:Pro Astigmata ARA:Ast Crustacea Pentastomata CRU:Pen References Ashford, R.W. & Crewe, W. 2003. The parasites of Homo sapiens: an annotated checklist of the protozoa, helminths and arthropods for which we are home. Taylor & Francis. Taylor, M.A., Coop, R.L. & Wall, R.L. 2007. Veterinary Parasitology. 3rd edition, Blackwell Pub. HOST-PARASITE CHECKLIST Class: MAMMALIA [mammals] Subclass: EUTHERIA [placental mammals] Order: PRIMATES [prosimians and simians] Suborder: SIMIAE [monkeys, apes, man] Family: HOMINIDAE [man] Homo sapiens Linnaeus, 1758 [man] ARA:Ast Sarcoptes bovis, ectoparasite (‘milker’s itch’)(mange mite) ARA:Ast Sarcoptes equi, ectoparasite (‘cavalryman’s itch’)(mange mite) ARA:Ast Sarcoptes scabiei, skin (mange mite) ARA:Ixo Ixodes cornuatus, ectoparasite (scrub tick) ARA:Ixo Ixodes holocyclus, ectoparasite (scrub tick, paralysis tick) ARA:Ixo Ornithodoros gurneyi, ectoparasite (kangaroo tick) ARA:Pro Cheyletiella blakei, ectoparasite (mite) ARA:Pro Cheyletiella parasitivorax, ectoparasite (rabbit fur mite) ARA:Pro Demodex brevis, sebacceous glands (mange mite) ARA:Pro Demodex folliculorum, hair follicles (mange mite) ARA:Pro Trombicula sarcina, ectoparasite (black soil itch mite) INS:Ano Pediculus capitis, ectoparasite (head louse) INS:Ano Pediculus humanus, ectoparasite (body -

Coinfection of Schistosoma (Trematoda) with Bacteria, Protozoa and Helminths
CHAPTER 1 Coinfection of Schistosoma (Trematoda) with Bacteria, Protozoa and Helminths ,† ‡ Amy Abruzzi* and Bernard Fried Contents 1.1. Introduction 3 1.2. Coinfection of Species of Schistosoma and Plasmodium 4 1.2.1. Animal studies 21 1.2.2. Human studies 23 1.3. Coinfection of Schistosoma Species with Protozoans other than in the Genus Plasmodium 24 1.3.1. Leishmania 32 1.3.2. Toxoplasma 32 1.3.3. Entamoeba 34 1.3.4. Trypanosoma 35 1.4. Coinfection of Schistosoma Species with Salmonella 36 1.4.1. Animal studies 36 1.4.2. Human studies 42 1.5. Coinfection of Schistosoma Species with Bacteria other than Salmonella 43 1.5.1. Mycobacterium 43 1.5.2. Helicobacter pylori 49 1.5.3. Staphylococcus aureus 50 1.6. Coinfection of Schistosoma and Fasciola Species 50 1.6.1. Animal studies 57 1.6.2. Human studies 58 * Skillman Library, Lafayette College, Easton, Pennsylvania, USA { Epidemiology, University of Medicine and Dentistry of New Jersey (UMDNJ), Piscataway, New Jersey, USA { Department of Biology, Lafayette College, Easton, Pennsylvania, USA Advances in Parasitology, Volume 77 # 2011 Elsevier Ltd. ISSN 0065-308X, DOI: 10.1016/B978-0-12-391429-3.00005-8 All rights reserved. 1 2 Amy Abruzzi and Bernard Fried 1.7. Coinfection of Schistosoma Species and Helminths other than the Genus Fasciola 59 1.7.1. Echinostoma 59 1.7.2. Hookworm 70 1.7.3. Trichuris 70 1.7.4. Ascaris 71 1.7.5. Strongyloides and Trichostrongyloides 72 1.7.6. Filarids 73 1.8. Concluding Remarks 74 References 75 Abstract This review examines coinfection of selected species of Schisto- soma with bacteria, protozoa and helminths and focuses on the effects of the coinfection on the hosts. -

Lecture 5: Emerging Parasitic Helminths Part 2: Tissue Nematodes
Readings-Nematodes • Ch. 11 (pp. 290, 291-93, 295 [box 11.1], 304 [box 11.2]) • Lecture 5: Emerging Parasitic Ch.14 (p. 375, 367 [table 14.1]) Helminths part 2: Tissue Nematodes Matt Tucker, M.S., MSPH [email protected] HSC4933 Emerging Infectious Diseases HSC4933. Emerging Infectious Diseases 2 Monsters Inside Me Learning Objectives • Toxocariasis, larva migrans (Toxocara canis, dog hookworm): • Understand how visceral larval migrans, cutaneous larval migrans, and ocular larval migrans can occur Background: • Know basic attributes of tissue nematodes and be able to distinguish http://animal.discovery.com/invertebrates/monsters-inside- these nematodes from each other and also from other types of me/toxocariasis-toxocara-roundworm/ nematodes • Understand life cycles of tissue nematodes, noting similarities and Videos: http://animal.discovery.com/videos/monsters-inside- significant difference me-toxocariasis.html • Know infective stages, various hosts involved in a particular cycle • Be familiar with diagnostic criteria, epidemiology, pathogenicity, http://animal.discovery.com/videos/monsters-inside-me- &treatment toxocara-parasite.html • Identify locations in world where certain parasites exist • Note drugs (always available) that are used to treat parasites • Describe factors of tissue nematodes that can make them emerging infectious diseases • Be familiar with Dracunculiasis and status of eradication HSC4933. Emerging Infectious Diseases 3 HSC4933. Emerging Infectious Diseases 4 Lecture 5: On the Menu Problems with other hookworms • Cutaneous larva migrans or Visceral Tissue Nematodes larva migrans • Hookworms of other animals • Cutaneous Larva Migrans frequently fail to penetrate the human dermis (and beyond). • Visceral Larva Migrans – Ancylostoma braziliense (most common- in Gulf Coast and tropics), • Gnathostoma spp. Ancylostoma caninum, Ancylostoma “creeping eruption” ceylanicum, • Trichinella spiralis • They migrate through the epidermis leaving typical tracks • Dracunculus medinensis • Eosinophilic enteritis-emerging problem in Australia HSC4933. -

Myiasis During Adventure Sports Race
DISPATCHES reexamined 1 day later and was found to be largely healed; Myiasis during the forming scar remained somewhat tender and itchy for 2 months. The maggot was sent to the Finnish Museum of Adventure Natural History, Helsinki, Finland, and identified as a third-stage larva of Cochliomyia hominivorax (Coquerel), Sports Race the New World screwworm fly. In addition to the New World screwworm fly, an important Old World species, Mikko Seppänen,* Anni Virolainen-Julkunen,*† Chrysoimya bezziana, is also found in tropical Africa and Iiro Kakko,‡ Pekka Vilkamaa,§ and Seppo Meri*† Asia. Travelers who have visited tropical areas may exhibit aggressive forms of obligatory myiases, in which the larvae Conclusions (maggots) invasively feed on living tissue. The risk of a Myiasis is the infestation of live humans and vertebrate traveler’s acquiring a screwworm infestation has been con- animals by fly larvae. These feed on a host’s dead or living sidered negligible, but with the increasing popularity of tissue and body fluids or on ingested food. In accidental or adventure sports and wildlife travel, this risk may need to facultative wound myiasis, the larvae feed on decaying tis- be reassessed. sue and do not generally invade the surrounding healthy tissue (1). Sterile facultative Lucilia larvae have even been used for wound debridement as “maggot therapy.” Myiasis Case Report is often perceived as harmless if no secondary infections In November 2001, a 41-year-old Finnish man, who are contracted. However, the obligatory myiases caused by was participating in an international adventure sports race more invasive species, like screwworms, may be fatal (2). -
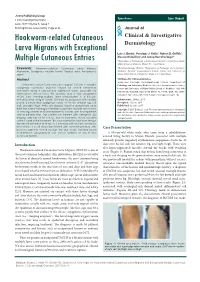
Hookworm-Related Cutaneous Larva Migrans with Exceptional Multiple Cutaneous Entries
Open Access Case Report J Clin Investigat Dermatol June 2017 Volume 5, Issue 1 © All rights are reserved by Vega et al. Journal of Hookworm-related Cutaneous Clinical & Investigative Larva Migrans with Exceptional Dermatology Luis J. Borda1, Penelope J. Kallis1, Robert D. Griffith1, Alessio Giubellino1 and Jeong Hee Cho-Vega2* Multiple Cutaneous Entries 1Department of Dermatology and Cutaneous Surgery, University of Miami Miller School of Medicine, Miami, FL, United States Keywords: Hookworm-related Cutaneous Larva Migrans; 2Dermatopathology Division, Department of Pathology and Laboratory Hookworm; Serpiginous multiple tracks; Tropical area; Anti-parasite Medicine, Sylvester Comprehensive Cancer Center and University of agent Miami Miller School of Medicine, Miami, FL, United States Abstract *Address for Correspondence Jeong Hee Cho-Vega, Dermatopathology Division, Department of Hookworm-related Cutaneous Larva Migrans (HrCLM) is a pruritic Pathology and Laboratory Medicine Sylvester Comprehensive Cancer serpiginous cutaneous eruption caused by animal hookworms Center and University of Miami Miller School of Medicine 1120 NW commonly found in tropical and subtropical areas, especially the 14th Street, Holtz ET, Suite 2146 Miami, FL 33136, USA, Tel: (305)- Southeastern United States. We describe here a very exceptional 243-6433; Fax: (305)-243-1624; E-mail: [email protected] HrCLM case showing multiple larva entries/lesions in a 63-year- old white male living in Miami. Clinically he presented with multiple Submission: 25 May, 2017 pruritic erythematous serpiginous tracks on his left anterior leg, left Accepted: 15 June, 2017 calf, and right thigh. While skin biopsies failed to demonstrate larva Published: 22 June, 2017 itself, the overall histological features supported multiple larva tracks Copyright: © 2017 Borda LJ, et al.