Resident and Family Handbook Personal Care Home
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
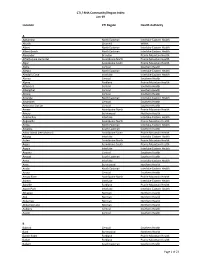
CTI / RHA Community/Region Index Jan-19
CTI / RHA Community/Region Index Jan-19 Location CTI Region Health Authority A Aghaming North Eastman Interlake-Eastern Health Akudik Churchill WRHA Albert North Eastman Interlake-Eastern Health Albert Beach North Eastman Interlake-Eastern Health Alexander Brandon Prairie Mountain Health Alfretta (see Hamiota) Assiniboine North Prairie Mountain Health Algar Assiniboine South Prairie Mountain Health Alpha Central Southern Health Allegra North Eastman Interlake-Eastern Health Almdal's Cove Interlake Interlake-Eastern Health Alonsa Central Southern Health Alpine Parkland Prairie Mountain Health Altamont Central Southern Health Albergthal Central Southern Health Altona Central Southern Health Amanda North Eastman Interlake-Eastern Health Amaranth Central Southern Health Ambroise Station Central Southern Health Ameer Assiniboine North Prairie Mountain Health Amery Burntwood Northern Health Anama Bay Interlake Interlake-Eastern Health Angusville Assiniboine North Prairie Mountain Health Anola North Eastman Interlake-Eastern Health Arbakka South Eastman Southern Health Arbor Island (see Morton) Assiniboine South Prairie Mountain Health Arborg Interlake Interlake-Eastern Health Arden Assiniboine North Prairie Mountain Health Argue Assiniboine South Prairie Mountain Health Argyle Interlake Interlake-Eastern Health Arizona Central Southern Health Amaud South Eastman Southern Health Ames Interlake Interlake-Eastern Health Amot Burntwood Northern Health Anola North Eastman Interlake-Eastern Health Arona Central Southern Health Arrow River Assiniboine -

Variations in Resource Use and Costs of Hospital Care in Manitoba
VARIATIONS IN RESOURCE USE AND COSTS OF HOSPITAL CARE IN MANITOBA Authors: Nathan Nickel, PhD Greg Finlayson, PhD Randy Fransoo, PhD Roxana Dragan, MA Charles Burchill, MSc Okechukwu Ekuma, MSc Tamara Thomson, MSc Leanne Rajotte, BComms(Hons) Joshua Ginter, MA Ruth-Ann Soodeen, MSc Susan Burchill, BMus Fall 2017 Manitoba Centre for Health Policy Max Rady College of Medicine Rady Faculty of Health Sciences University of Manitoba This report is produced and published by the Manitoba Centre for Health Policy (MCHP). It is also available in PDF format on our website at: http://mchp-appserv.cpe.umanitoba.ca/deliverablesList.html Information concerning this report or any other report produced by MCHP can be obtained by contacting: Manitoba Centre for Health Policy Rady Faculty of Health Sciences Max Rady College of Medicine, University of Manitoba 4th Floor, Room 408 727 McDermot Avenue Winnipeg, Manitoba, Canada R3E 3P5 Email: [email protected] Phone: (204) 789-3819 Fax: (204) 789-3910 How to cite this report: Nickel N, Finlayson G, Fransoo R, Dragan R, Burchill C, Ekuma O, Thomson T, Rajotte L, Ginter J, Soodeen RA, Burchill S. Variations in Resource Use and Costs of Hospital Care in Manitoba. Winnipeg, MB. Manitoba Centre for Health Policy, Fall 2017. Legal Deposit: Manitoba Legislative Library National Library of Canada ISBN 978-1-896489-86-5 ©Manitoba Health This report may be reproduced, in whole or in part, provided the source is cited. 1st printing (Fall 2017) This report was prepared at the request of Manitoba Health, Seniors and Active Living (MHSAL) as part of the contract between the University of Manitoba and MHSAL. -

Prairie Mountain Health
Manitoba Health, Seniors and Active Living Population Report - June 1, 2020 Population of Prairie Mountain Health June 1, 2020 Manitoba RHAs -- Prairie Mountain Health Prairie Mountain Health (c) Prov. of Manitoba, 2021 Cartography by: MHSAL, Information Management & Analytics Last update: April. 2021 Manitoba Health, Seniors, and Active Living Population Report, June 1, 2020 Prairie Mountain Health Region District Gender Under 1 1 - 4 5 - 9 10 - 14 15 - 19 20 - 24 25 - 29 30 - 34 35 - 39 40 - 44 45 - 49 50 - 54 55 - 59 60 - 64 65 - 69 70 - 74 75 + Total PMH Brandon Zone Brandon Downtown F 78 306 391 298 378 499 534 490 453 419 375 326 338 285 227 224 580 6,201 M 68 322 403 334 361 473 559 537 523 432 391 344 349 283 207 157 284 6,027 Brandon East End F 49 189 235 240 187 217 266 300 266 241 198 169 207 164 118 121 407 3,574 M 42 180 255 209 204 230 279 282 299 246 218 171 200 156 115 84 226 3,396 Brandon North Hill F 44 150 204 234 217 233 282 272 265 241 228 210 290 254 269 235 303 3,931 M 40 175 251 236 208 214 248 266 236 216 238 210 228 240 218 181 285 3,690 Brandon South End F 70 284 343 313 289 327 371 434 435 370 333 308 344 330 269 243 355 5,418 M 66 300 390 343 324 354 353 366 431 385 342 307 306 277 259 199 276 5,278 Brandon West End F 78 440 566 570 517 585 642 686 675 659 557 466 542 487 464 390 756 9,080 M 93 453 579 593 537 547 541 647 644 592 579 458 482 449 401 344 524 8,463 F 319 1,369 1,739 1,655 1,588 1,861 2,095 2,182 2,094 1,930 1,691 1,479 1,721 1,520 1,347 1,213 2,401 28,204 M 309 1,430 1,878 1,715 1,634 1,818 -

02:00 PM 2020-10-14 On
1 1 RETURN BIDS TO: Title - Sujet RETOURNER LES SOUMISSIONS À: Fire, Safety and Rescue Equi (RFSO) Bid Receiving - PWGSC / Réception des soumissions - Solicitation No. - N° de l'invitation Date TPSGC E60HN-20FSRE/B 2020-10-02 11 Laurier St. / 11, rue Laurier Client Reference No. - N° de référence du client Amendment No. - N° modif. Place du Portage, Phase III E60HN-20FSRE 003 Core 0B2 / Noyau 0B2 Gatineau, Québec K1A 0S5 File No. - N° de dossier CCC No./N° CCC - FMS No./N° VME Bid Fax: (819) 997-9776 hn336.E60HN-20FSRE GETS Reference No. - N° de référence de SEAG PW-$$HN-336-79041 Date of Original Request for Standing Offer 2020-08-31 Revision to a Request for a Standing Offer Date de la demande de l'offre à commandes originale Révision à une demande d'offre à commandes Solicitation Closes - L'invitation prend fin Time Zone Fuseau horaire National Master Standing Offer (NMSO) at - à 02:00 PM on - le 2020-10-14 Eastern Daylight Offre à commandes principale et nationale (OCPN) Saving Time EDT Address Enquiries to: - Adresser toutes questions à: Buyer Id - Id de l'acheteur Bisson(hn336), Phillipe hn336 The referenced document is hereby revised; unless otherwise indicated, all other terms and conditions of Telephone No. - N° de téléphone FAX No. - N° de FAX the Offer remain the same. (613) 295-8641 ( ) ( ) - Delivery Required - Livraison exigée Ce document est par la présente révisé; sauf indication contraire, les modalités de l'offre demeurent les mêmes. Destination - of Goods, Services, and Construction: Destination - des biens, services et construction: Comments - Commentaires 140 O'Connor St., Ottawa, ON Canada K1A 0R5 Vendor/Firm Name and Address Security - Sécurité Raison sociale et adresse du This revision does not change the security requirements of the Offer. -

Prairie Mountain Health CHA 2019 7-1-2020 Update
PRAIRIE MOUNTAIN HEALTH COMMUNITY HEALTH ASSESSMENT 2019 Acknowledgements Prairie Mountain Health acknowledges that it provides services in facilities and sites located on the original lands and traditional territories of the Cree, Dakota, Ojibway, Oji-Cree and homelands of the Métis. Prairie Mountain Health respects that the First Nation Treaties were made on these territories and we dedicate ourselves to continued collaboration in partnership with First Nation, Métis and Inuit people in the spirit of reconciliation. This report was prepared by the Prairie Mountain Health Community Health Assessment (CHA) team: Jody Allan, Angie Allen, Michelle Gaber, Nancy McPherson, Pamela McTavish, Amy Ostash, Nancy Tregunna, and Colin Williams. We could not have completed the CHA without the partners who provided us with the data, in particular Manitoba Health, Seniors and Active Living and Manitoba Centre for Health Policy. The team would like to express gratitude to those that have participated and contributed to the Community Health Assessment process. The 2019 CHA process has been a true collaboration. We would like to thank all Community Health Assessment Network members from across the province, staff at Manitoba Health, Seniors and Active Living and the Prairie Mountain Health Executive Management Team for their continued support and guidance. We are grateful to have such commitment and dedication in Manitoba. To provide feedback on the report, please email: [email protected]. This report is produced and published by the Prairie Mountain Health CHA team. It is available in PDF format on our website at: http://prairiemountainhealth.ca/cha-2019 If you would like more information about the Community Health Assessment, please contact Prairie Mountain Health at: Prairie Mountain Health Corporate Office 192-1st Avenue West Box 579 Souris, Manitoba R0K 2C0 Toll-free: 1-888-682-2253 Website: www.prairiemountainhealth.ca How to cite this report: McPherson N, Williams C, McTavish P, Allen A, Gaber M, Ostash A, Tregunna N, Allan J. -

District Profile Whitemud
DISTRICT PROFILE WHITEMUD LOCATION AND DEMOGRAPHICS LOCATION The Whitemud district is located in the South Zone on the east side of the PMH region. The district extends from the southeast corner of Riding Mountain National Park in the north to the Town of Carberry in the south. 1 2 2 DEMOGRAPHICS Population : 11,490 Land Area: 3,913 km Density: 2.94 persons/km FACILITIES Neepawa Health Centre, Neepawa PCH (Country Meadows), and Carberry Health Centre and PCH. COMMUNITY HEALTH Public Health, Home Care, Mental Health, Primary Health Care, Emergency SERVICES Medical Services DID YOU KNOW? Whitemud has the lowest prevalence of Total Respiratory Morbidity in Prairie Mountain Health Whitemud has the lowest prevalence of Substance Abuse in PMH ! Less than 50% of new depression patients in Whitemud had appropriate antidepressant follow-up care ! Whitemud has the second lowest rate of Appropriate Asthma Medication Use in the South Zone amongst those diagnosed with asthma Over 25% of Whitemud seniors (age 75+) living in the community (not in a personal care home) use Benzodiazepines SOCIAL AND ECONOMIC INDICATORS 5.5 dependents age LIFE DEPENDENCY 0-14 and 65+ for every 2 1 EXPECTANCY 83.2 years 78.0 years RATIO 10 of working age 15-64 Tenant: MEDIAN HOUSING 15.7% < 29.1% (PMH) HOUSEHOLD $53,867 > $50,888 3 3 AFFORDABILITY Owner: INCOME (PMH) 10.4% > 9.9% (PMH) 20% > 19% (PMH) EDUCATION population aged 25- UNEMPLOYMENT 3 3 LEVEL 64 without a High RATE 2.5% < 5.9% (PMH) School Diploma NOTES 1 Manitoba Health Population Reports, 2013 2 Manitoba Centre for Health Policy RHA Indicators Atlas, 2013 3 2011 Census. -
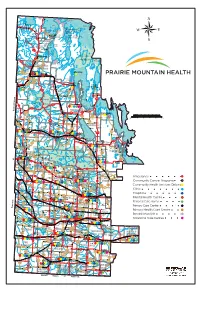
PMH Regional Map
Little Haider Goose Lake Putahow Nueltin Head River Ballantyne L Falloon Egg Lopuck Lake Commonwealth L Partridge Lake Todd Lake Nabel Is Lake Lake Strachan Putahow Blevins Coutts Veal L Lake Lake Lake Tice Lake Savage Lake Hutton Lake Lake Lake Dickins R Nahili Bulloch COLVIN LAKE Colvin L John Lake R Lake Koona Osborn Round Gronbeck Thuytowayasay NUELTIN LAKE L Jonasson Gillander Lake Bangle Inverarity Sand L Lake L Kasmere Lake Lake Lake Lake PROVINCIAL PARK McEwen Sucker Drake Ewing Kitchen CARIBOU RIVER Lake Sandy L Guick Ashey Lake Kirk L Lake L Lake Shannon Lake Gagnon Vinsky Secter L Hanna L River Turner Corbett Lake Nejanilini Lake Butterworth Lake Lemmerick Creba Lake Croll PARK RESERVE Ck Lake Lake PROVINCIAL PARK L Lake Kasmere Lake Falls Tatowaycho R Creek L Grevstad Thlewiaza Caribou HUDSON Bartko MacMillian Lake Hillhouse Booth Little Long Snyder L Lake Bambridge Lake Lake Duck Jethe Lake Lake L Baird Lake L Ibbott Alyward Lake Duck Lake Post River Lake Choquette L Caribou Gross Hubbart Point Lake Sandhill Wolverine Lake L Fort Hall Lake Topp L Maughan Clarke River Ouellet Lake L L Ferris Atemkameskak Big Van Der Vennet Mistahi Lake Palulak L L Brownstone Barr Quasso L L Colbeck Doig Munroe Oolduywas Lake Lake Lake L Blackfish Lake Lake Lake Spruce Lake Sothe Sothe Macleod L Endert Cangield L Whitmore Minuhik R Law Lake L Lake Cochrane R Lake Lake Warner Lake Adair Naelin Thuykay Tessassage Greening L Lake L Lake Weepaskow North Lake Duffin Egenolf Lake Hoguycho Numaykos L Copeland Spruce Point of the Woods Lake L River -

Career Opportunity
Career Opportunity PHYSICIAN ASSISTANT (PA) – Brandon Regional Health Centre Surgical Program Prairie Mountain Health is accepting applications for a full-time Physician Assistant at Brandon Regional Health Centre. The Physician Assistant will act as a collaborative team member with Surgeons, Nurses, Residents and other support members that make up the Surgical Team. Principle responsibilities will include having a strong theoretical knowledge base and advanced level of clinical experience / surgical assisting in caring for General Surgery patients. Duties will include surgical assisting, inpatient care and management, and emergency consults as required. The PA will be a leader in their field with strengths in quality improvement, research and team diagnosis and administrative responsibilities. Required qualifications: Must be a graduate of an accredited Physician Assistant educational program and eligible for national certification. Eligibility to be licensed by the College of Physicians and Surgeons or certification with an accrediting body of Physician Assistants. Flexible with superior organization skills and ability to work efficiently to prioritize multiple, competing tasks in a fast paced and dynamic environment. Ability to show sound judgment and discretion, make decision and take initiative while working with confidential patient information and patient inquiries. Superior work ethic, professionalism and reliability. Commitment to high standards in patient care including knowledge of safe work practices and patient care. Above average written/oral communication skills; excellent interpersonal skills; and the ability to effectively communicate factual information and detailed explanations. Satisfactory work performance and attendance record. Experience in an Operating Room environment. The General Surgery at Brandon Regional Health Centre includes a wide variety of procedures including Colorectal Surgery, Endocrine Surgery, Surgery of the Liver, Pancreas, and Biliary Tree, Head and Neck Surgery and Minimally-invasive surgery. -

MUNICIPALITY of Mccreary
MUNICIPALITY OF McCREARY Minutes of the Regular Council Meeting of the Municipality of McCreary held on March 18, 2020 in the Municipality of McCreary Council Chambers located at 432 First Avenue in McCreary, Manitoba. Head of Council Gawaziuk called this regular meeting to order at 5:57 p.m. PRESENT: Head of Council Mike Gawaziuk Deputy Head of Council Shawn Buchanan Councillor Donna Duggan Councillor John Graves Councillor Craig Terrick Chief Administrative Officer Wendy Turko Due to the COVID-19 Pandemic this meeting was held using Social Distancing practices. A member of the public attending was asked the screening questions and asked to use Social Distancing practices while attending. #116/2020 BE IT RESOLVED THAT the Agenda for the March 18, 2020 Regular Meeting be adopted as prepared by the Chief Administrative Officer and with the following addition(s): Petitions and Correspondence: Mar 17/2020 Prairie Mountain Health COVID-19 Preparedness and Guidelines from Prairie Mountain Health – COPIED; Mar 12/2020 Dauphin Regional Airport 2020 Funding Request–COPIED; Authority Inc. Mar 17/2020 McCreary Recreation Homecoming King or Queen Commission Sponsorship Request – COPIED; Mar 10/2020 Mountain View School 2020 Notice of Tax Requirements Division - COPIED. CARRIED. #117/2020 BE IT RESOLVED THAT the Minutes of the following meetings be approved as presented: - February 19, 2020 Regular Meeting; - February 24, 2020 Special Meeting; - February 26, 2020 Special Meeting; - March 2, 2020 Special Meeting; - March 10, 2020 Special Meeting. CARRIED. DELEGATIONS and REPORTS: 6:05 p.m. Public Works Report –Tyler McFadyen, Operations Foreman–COPIED: This report was not available at this time. -
Possible Public Exposures to COVID-19 in Prairie Mountain Health
Possible public exposures to COVID-19 in Prairie Mountain Health August 8 - December 27, 2020 Town/Municipality Location Dates/Times Ste. Rose du Lac Ste. Rose School (280 Gendreau St., Ste. December 17, 2020 Rose du Lac) December 27, 2020 - Letter to Parents/Guardians (pdf) Ste. Rose du Lac Ste. Rose School (280 Gendreau St., Ste. December 17, 2020 Rose du Lac) A confirmed case of COVID-19 was in the school on Dec. 17 when that individual may have been infectious. Based on the public health investigation, this exposure was assessed to be low risk. The infection was not believed to be acquired at school. Close contacts connected to the case have been identified and advised to self-isolate. Anyone who is a close contact has received a close contact letter or phone call from public health. Brandon Earl Oxford School (540 18th St., Brandon) December 15 to 18, 2020 A confirmed case of COVID-19 was in the school on Dec.15 to 18 when the individual may have been infectious. Based on the public health investigation, this exposure was assessed to be low risk. The infection was not believed to be acquired at school. Close contacts connected to the case have been identified and advised to self-isolate. Anyone who is a close contact has received a close contact letter or phone call from public health. Brandon Vincent Massey High School (715 December 15, 2020 McDiarmid Dr., Brandon) A confirmed case of COVID-19 was in the school on Dec. 15 when they may have been infectious. -

Health and Wellness for All Annual Report
Health and Wellness for All Annual Report 2014 - 2015 Table of Contents Letter of Transmittal/Accountability Page 1 Our Results: -Improved Service Delivery Page 14 Executive Management Team Message Page 2 -Improved Health Status and Reduced PMH Board of Directors Page 3 Health Disparities Page 15 Board Governance Page 4 Awards and Recognition Page 16 Organizational and Advisory Structure Page 5 Financial Position and Operations Page 17/18 Prairie Mountain Health at a Glance Page 6 Auditor’s Report Page 19 PMH feature: My Health Team - Brandon Page 7 Administrative Costs Page 20 PMH feature: Murray House Page 8 Accountability Provisions Page 20 Our Results: Public Interest Disclosure Page 21 -Capacity Building Page 9/10 -Health System Innovation Page 11 French Language Services Page 21 -Health System Sustainability Page 12 -Improved Access Page 13 Letter of Transmittal and Accountability e are pleased to present the annual report for Prairie Mountain Health for the fiscal year ended March 31, W 2015 as approved by the Board of Directors on September 22, 2015. The annual report was prepared under the Board's direction in accordance with the Regional Health Authorities Act and directions provided by the Minister of Health. All material, economic and fiscal implications known as of March 31, 2015 have been considered in preparing this annual report. This report reviews the actions and initiatives of Prairie Mountain Health from April 1, 2014 to March 31, 2015. As with all health care organizations, the years ahead will continue to present many challenges. However, with the assistance of our staff, our community partners and of course, Manitoba Health, Healthy Living and Seniors, we will continue to strive to meet the Vision and Mission we have articulated. -

Long Term Care Strategy –To Support
Long Term Care Strategy – To support “Aging In Place” Supports to Seniors in Group Living (SSGL) AN INTRODUCTION: • Manitoba Health’s Long Term Care Strategy is focused on creation community living options/alternatives to: – Modernize Care for Manitoban’s – More affordable choices – Affordable Housing with supports – Delay PCH placement – Help individuals “Age in Place” AGING IN PLACE, DEVELOPMENT AND ROLES • Aging in Place is a matter of preserving the ability for Manitobans from every culture to remain safely, as participants in their own community, to enjoy the familiar, social, cultural, spiritual interactions that enrich their lives even though their health may be compromised. AGING IN PLACE is a lifestyle that supports the following inherent values: • Safety and Security-living with reduced risks in the home. • Flexibility – adjusting services to meet changing needs. • Choice – freedom to choose among options. Con’t • Equity – equal access to all seniors • Dignity – Ability to maintain a sense of self worth and self esteem. Overall, work in partnership with existing community resources to best serve the client and help them to maintain their independence in the community AGING IN PLACE-Long Term Strategy • Mission Statement – For Manitobans of all ages – Supports aging and care in place – Services are accessible, affordable, flexible and integrated – Supports wellness in the environment of “home” – Prevents premature admission to PCH The Goals of the LTC Strategy are to: – Allow individuals to age in place as a viable member of their community and family – Prevent premature or inappropriate placement of light levels of care into PCH – Decrease admissions and length of stay for seniors and young disabled in acute care Supports to Seniors in Group Living: SSGL • Model provides a range of services in group living/elderly person housing.