The Temporospatial Dimension of Health in Zimbabwe Evans Chazireni Phd Geography University of South Africa
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Midlands Province Mobile Voter Registration Centres
Midlands Province Mobile Voter Registration Centres Chirumhanzu District Team 1 Ward Centre Dates 18 Mwire primary school 10/06/13-11/06/13 18 Tokwe 4 clinic 12/06/13-13/06/13 18 Chingegomo primary school 14/06/13-15/06/13 16 Chishuku Seondary school 16/06/13-18/06/13 9 Upfumba Secondary school 19/06/13-21/06/13 3 Mutya primary school 22/06/13-24/06/13 2 Gonawapotera secondary school 25/06/13-27/06/13 20 Wildegroove primary school 28/06/13-29/06/13 15 Kushinga primary school 30/06/13-02/07/13 12 Huchu compound 03/07/13-04/-07/13 12 Central estates HQ 5/7/13 20 Mtao/Fair Field compound 6/7/13 12 Chiudza homestead 07/07/13-08/06/13 14 Njerere primary school 9/7/13 Team 2 Ward Centre Dates 22 Hillview Secondary school 10/07/13-12/07/13 17 Lalapanzi Secondary school 13/07/13-15/07/13 16 Makuti homestead 16/06/13-17/06/13 1 Mapiravana Secondary school 18/06/13-19/06/13 9 Siyahukwe Secondary school 20/06/13-23/06/13 4 Chizvinire primary school 24/06/13-25/06/13 21 Mukomberana Seconadry school 26/06/13-29/06/13 20 Union primary school 30/06/13-01/07/13 15 Nyikavanhu primary school 02/07/13-03/07/13 19 Musens primary school 04/07/13-06/07/13 16 Utah primary school 07/7/13-09/07/13 Team 3 Ward Centre Dates 11 Faerdan primary school 10/07/13-11/07/13 11 Chamakanda Secondary school 12/07/13-14/07/13 11 Chamakanda primary school 15/07/13-16/07/13 5 Chizhou Secondary school 17/06/13-16/06/13 3 Chilimanzi primary school 21/06/13-23/06/13 25 Maponda primary school 24/06/13-25/06/13 6 Holy Cross seconadry school 26/06/13-28/06/13 20 New England Secondary -

Participation of Women in the Health
Ayaz et al. Hum Resour Health (2021) 19:94 https://doi.org/10.1186/s12960-021-00635-7 REVIEW Open Access Participation of women in the health workforce in the fragile and confict-afected countries: a scoping review Basnama Ayaz1* , Maria Athina Martimianakis2, Carles Muntaner1 and Sioban Nelson1 Abstract Introduction and background: The full participation of women as healthcare providers is recognized globally as critical to favorable outcomes at all levels, including the healthcare system, to achieving universal health coverage and sustainable development goals (SDGs) by 2030. However, systemic challenges, gender biases, and inequities exist for women in the global healthcare workforce. Fragile and confict-afected states/countries (FCASs) experience addi- tional pressures that require specifc attention to overcome challenges and disparities for sustainable development. FCASs account for 42% of global deaths due to communicable, maternal, perinatal, and nutritional conditions, requir- ing an appropriate health workforce. Consequently, there is a need to understand the impact of gender on workforce participation, particularly women in FCASs. Methods: This scoping review examined the extent and nature of existing literature, as well as identifed factors afecting women’s participation in the health workforce in FCASs. Following Arksey and O’Malley’s scoping review methodology framework, a systematic search was conducted of published literature in fve health sciences databases and grey literature. Two reviewers independently screened the title and abstract, followed by a full-text review for shortlisted sources against set criteria. Results: Of 4284, 34 sources were reviewed for full text, including 18 primary studies, fve review papers, and 11 grey literature sources. In most FCASs, women predominate in the health workforce, concentrated in nursing and mid- wifery professions; medicine, and the decision-making and leadership positions, however, are occupied by men. -

For Human Dignity
ZIMBABWE HUMAN RIGHTS COMMISSION For Human Dignity REPORT ON: APRIL 2020 i DISTRIBUTED BY VERITAS e-mail: [email protected]; website: www.veritaszim.net Veritas makes every effort to ensure the provision of reliable information, but cannot take legal responsibility for information supplied. NATIONAL INQUIRY REPORT NATIONAL INQUIRY REPORT ZIMBABWE HUMAN RIGHTS COMMISSION ZIMBABWE HUMAN RIGHTS COMMISSION For Human Dignity For Human Dignity TABLE OF CONTENTS FOREWORD .................................................................................................................................................. vii ACRONYMS.................................................................................................................................................... ix GLOSSARY OF TERMS .................................................................................................................................. xi PART A: INTRODUCTION TO THE NATIONAL INQUIRY PROCESS ................................................................ 1 CHAPTER 1: INTRODUCTION ........................................................................................................................ 1 1.1 Establishment of the National Inquiry and its Terms of Reference ....................................................... 2 1.2 Methodology ..................................................................................................................................... 3 CHAPTER 2: THE NATIONAL INQUIRY PROCESS ......................................................................................... -

Zimbabwe.Beef.20190321.Approved V2
Value Chain Analysis for Development (VCA4D) is a tool funded by the European Commission / DEVCO and is implemented in partnership with Agrinatura. Agrinatura (http://agrinatura-eu.eu) is the European AllianCe of Universities and Research Centers involved in agricultural researCh and CapaCity building for development. The information and knowledge produCed through the value Chain studies are intended to support the Delegations of the European Union and their partners in improving poliCy dialogue, investing in value Chains and better understanding the Changes linked to their aCtions VCA4D uses a systematiC methodologiCal framework for analysing value Chains in agriCulture, livestoCk, fishery, aquaCulture and agroforestry. More information inCluding reports and communication material Can be found at: https://europa.eu/CapaCity4dev/value-chain-analysis-for- development-vca4d- Team Composition Ben Bennett, Team Leader and eConomist (NRI) Muriel Figué, social expert (CIRAD) Mathieu Vigne, environmental expert (CIRAD) Charles Chakoma, national consultant (independent) Pamela KatiC, support to economist (NRI) The report was produCed through the finanCial support of the European Union. Its content is the sole responsibility of its authors and does not neCessarily refleCt the views of the European Union. The report has been realised within a projeCt finanCed by the European Union (VCA4D CTR 2016/375-804). Citation of this report: Bennett, B., Chakoma, C., Figué, M, Vigne, M., KatiC, P.; 2019. Beef Value Chain Analysis in Zimbabwe. Report for the -
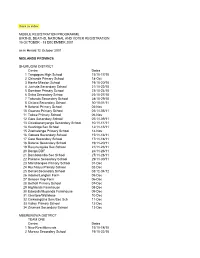
Back to Index MOBILE REGISTRATION PROGRAMME
Back to index MOBILE REGISTRATION PROGRAMME BIRTHS, DEATHS, NATIONAL AND VOTER REGISTRATION 15 OCTOBER - 13 DECEMBER 2001 as in Herald 12 October 2001 MIDLANDS PROVINCE SHURUGWI DISTRICT Centre Dates 1 Tongogara High School 15/10-17/10 2 Chironde Primary School 18-Oct 3 Hanke Mission School 19/10-20/10 4 Juchuta Secondary School 21/10-22/10 5 Dombwe Primary School 23/10-24/10 6 Svika Secondary Schoo 25/10-27/10 7 Takunda Secondary School 28/10-29/10 8 Chitora Secondary School 30/10-01/11 9 Batanai Primary School 02-Nov 10 Gwanza Primary School 03/11-05/11 11 Tokwe Primary School 06-Nov 12 Gare Secondary School 07/11-09/11 13 Chivakanenyanga Secondary School 10/11-11/11 14 Kushinga Sec School 12/11-13/11 15 Zvamatenga Primary School 14-Nov 16 Gamwa Secondary School 15/11-16/11 17 Gato Secondary School 17/11-18/11 18 Batanai Secondary School 19/11-20/11 19 Rusununguko Sec School 21/11-23/11 20 Donga DDF 24/11-26/11 21 Dombotombo Sec School 27/11-28/11 22 Pakame Secondary School 29/11-30/11 23 Marishongwe Primary School 01-Dec 24 Ruchanyu Primary School 02-Dec 25 Dorset Secondary School 03/12-04/12 26 Adams/Longton Farm 05-Dec 27 Beacon Kop Farm 06-Dec 28 Bethall Primary School 07-Dec 29 Highlands Farmhouse 08-Dec 30 Edwards/Muponda Farmhouse 09-Dec 31 Glentore/Wallclose 10-Dec 32 Chikwingizha Sem/Sec Sch 11-Dec 33 Valley Primary School 12-Dec 34 Zvumwa Secondary School 13-Dec MBERENGWA DISTRICT TEAM ONE Centre Dates 1 New Resettlements 15/10-18/10 2 Murezu Secondary School 19/10-22/10 3 Chizungu Secondary School 23/10-26/10 4 Matobo Secondary -

Zimbabwe Livestock Development Program June 2015 – September 2016
Annual Report #1 Zimbabwe Livestock Development Program June 2015 – September 2016 Feed the Future Zimbabwe Livestock Development Program | Annual Report #1 Fintrac Inc. www.fintrac.com [email protected] US Virgin Islands 3077 Kronprindsens Gade 72 St. Thomas, USVI 00802 Tel: (340) 776-7600 Fax: (340) 776-7601 Washington, DC 1400 16th Street, NW, Suite 400 Washington, D.C. 20036 USA Tel: (202) 462-8475 Fax: (202) 462-8478 Feed the Future Zimbabwe Livestock Development Program (FTFZ-LD) 5 Premium Close Mt. Pleasant Business Park Mt. Pleasant, Harare Zimbabwe Tel: +263 4 338964-69 [email protected] www.fintrac.com All Photos by Fintrac October 2016 This publication was produced for review by the United States Agency for International Development (USAID). It was prepared by Fintrac Inc. under contract AID-613-C-15-00001 with USAID/Zimbabwe. Prepared by Fintrac Inc. Feed the Future Zimbabwe Livestock Development Program | Annual Report #1 CONTENTS FOREWORD .................................................................................................................... III 1. EXECUTIVE SUMMARY ................................................................................... 1 2. PROGRAM OBJECTIVES .................................................................................. 5 3. ACTIVITIES ................................................................................................................... 7 3.1 Beneficiaries ......................................................................................................................................................... -

Zimbabwe HIV Care and Treatment Project Baseline Assessment Report
20 16 Zimbabwe HIV Care and Treatment Project Baseline Assessment Report '' CARG members in Chipinge meet for drug refill in the community. Photo Credits// FHI 360 Zimbabwe'' This study is made possible through the support of the American People through the United States Agency for International Development (USAID.) The contents are the sole responsibility of the Zimbabwe HIV care and Treatment (ZHCT) Project and do not necessarily reflect the views of USAID or the U.S. Government. FOREWORD The Government of Zimbabwe (GoZ) through the Ministry of Health and Child Care (MoHCC) is committed to strengthening the linkages between public health facilities and communities for HIV prevention, care and treatment services provision in Zimbabwe. The Ministry acknowledges the complementary efforts of non-governmental organisations in consolidating and scaling up community based initiatives towards achieving the UNAIDS ‘90-90-90’ targets aimed at ending AIDS by 2030. The contribution by Family Health International (FHI360) through the Zimbabwe HIV Care and Treatment (ZHCT) project aimed at increasing the availability and quality of care and treatment services for persons living with HIV (PLHIV), primarily through community based interventions is therefore, lauded and acknowledged by the Ministry. As part of the multi-sectoral response led by the Government of Zimbabwe (GOZ), we believe the input of the ZHCT project will strengthen community-based service delivery, an integral part of the response to HIV. The Ministry of Health and Child Care however, has noted the paucity of data on the cascade of HIV treatment and care services provided at community level and the ZHCT baseline and mapping assessment provides valuable baseline information which will be used to measure progress in this regard. -
Investment Case Sixth Replenishment 2019 Ending the Epidemics of Hiv, Tuberculosis and Malaria by 2030 Is Within Reach, but Not Yet Fully in Our Grasp
INVESTMENT CASE SIXTH REPLENISHMENT 2019 ENDING THE EPIDEMICS OF HIV, TUBERCULOSIS AND MALARIA BY 2030 IS WITHIN REACH, BUT NOT YET FULLY IN OUR GRASP. WITH ONLY 11 YEARS LEFT, WE HAVE NO TIME TO WASTE. WE MUST STEP UP THE FIGHT NOW. I. TABLE OF CONTENTS I. Executive Summary 1 II. Ending AIDS, TB and Malaria is Critical to Achieving the SDGs and Universal Health Coverage 8 III. Step Up or Slip Back? 12 IV. More Innovation, Collaboration, and Execution 19 V. The Global Fund Needs at Least US$14 Billion for the Next Three-Year Cycle 29 VI. The Global Fund Partnership Builds on a Robust Track Record of Impact 39 VII. Conclusion: Now is the Time to Step Up the Fight 44 ANNEX 1: Selected Global Fund 2017-2022 Key Performance Indicators and Targets 47 ANNEX 2: Methodology for Estimating the Resource Needs 48 ANNEX 3: Projection of Available Resources 49 ANNEX 4: Methodology for Impact Modelling 51 ANNEX 5: Methodology for ROI calculation 54 ANNEX 6: Results: Essential Indicators 55 STEP UP THE FIGHT 2019 I. EXECUTIVE SUMMARY 1 STEP UP THE FIGHT 2019 Ending the epidemics of HIV, tuberculosis and malaria The Global Fund plays a vital role in achieving this target If we don’t prevent teens, particularly girls, from getting by 2030 is within reach, but not yet fully in our grasp. and in accelerating progress toward universal health infected with HIV, the massive increase in the youth With only 11 years left, we have no time to waste. We coverage. While governments and communities must population in Africa will lead to more new infections must step up the fight now. -

Zimbabwe Page 1 of 35
Zimbabwe Page 1 of 35 Zimbabwe Country Reports on Human Rights Practices - 2001 Released by the Bureau of Democracy, Human Rights, and Labor March 4, 2002 Zimbabwe is a republic in which President Robert Mugabe and his Zimbabwe African National Union-Patriotic Front (ZANU-PF) have dominated the executive and legislative branches of the Government since independence in 1980. Although the Constitution allows for multiple parties, opposition parties and their supporters were subjected to significant intimidation and violence by the ruling party and government security forces, and financial restrictions continued to be imposed on the opposition. The 2000 parliamentary elections were preceded by a government-sanctioned campaign of violence directed towards supporters and potential supporters of the opposition. Although most election observers agreed that the voting process itself generally was peaceful, there were irregularities. In 1999 the country's first viable opposition party emerged, the Movement for Democratic Change (MDC), which won 57 out of 120 seats in the June 2000 parliamentary elections. The Constitution provides for an independent judiciary, and in practice the judiciary remained largely independent despite government attempts to dilute its independence; however, the Government repeatedly refused to abide by judicial decisions. The Zimbabwe Republic Police (ZRP) is responsible for maintaining law and order. Although the ZRP officially is under the authority of the Ministry of Home Affairs, in practice it is controlled by the President's office. The Zimbabwe National Army and Air Force under the Defense Ministry are responsible for external security; however, they frequently were called upon for domestic operations during the year. The Central Intelligence Organization (CIO), under the Minister of State for National Security in the President's Office, is responsible for internal and external security, but it does not have powers of arrest. -

Zimconsult Independent Economic & Planning Consultants
Zimconsult Independent economic & planning consultants FAMINE IN ZIMBABWE Famine in Zimbabwe Implications of 2003/04 Cropping season Prepared for the Friedrich Ebert Stiftung April 2004 ii Famine in Zimbabwe Implications of 2003/04 Cropping season CONTENTS Acronyms………………………………………………………………………...…ii 1. INTRODUCTION.........................................................................................1 2. METHODOLOGY........................................................................................1 3. SUMMARY OF FINDINGS..........................................................................2 3.1 Demand..............................................................................................................2 3.2 Production..........................................................................................................3 3.3 Urban Maize.......................................................................................................3 4. FACTORS DETERMINING FOOD PRODUCTION ....................................4 4.1 Maize Seed .......................................................................................................4 4.2 Shortage of Fertilizers.......................................................................................5 4.3 Tillage................................................................................................................6 4.4 Rainfall ..............................................................................................................6 4.5 Combined Effects of the -

The Impact of Economic Performance on Health in Zimbabwe
The Impact of Economic Performance on Health in Zimbabwe Policy Brief By Dr. A. Makochekanwa Gaborone, Botswana Mobile: +267 76 19 19 97 : +267 7552 7583 Email : [email protected] :[email protected] 4th July 2012 1 1 Introduction The nexus between economic growth and health outcomes has been extensively studied. However the relationship between the two is not clear. Historically, decline in both infant and child mortality rates, and the fall in both male and female adult mortality rates especially since the turn of the 20 th century has been attributed to a multiplicity of factors associated with economic and social advancement. These factors include rising availability of material goods, urbanization, improved infrastructure and housing, rising levels of education, improvement in personal and social hygiene, medical advances, the disappearance of slavery, and other host of significant reductions in discrimination for gender, religious, ethnic groups, etc Whilst most studies and logical reasoning posits a positive relationship between economic growth and improved health, it is important to note that sometimes improved economic growth can result in decline in health. Granados and Ionides (2007) indicate that the negative association found between economic growth and health progress in the most recent half century. These modern studies reveal a short-term tendency of death rates to increase during economic expansions in industrialized countries in recent decades (Graham et al., 1992; Abdala et al., 2000; Ruhm 2000 and 2003). Despite existence of inverse relationship between increase in gross domestic product (GDP) and decline in health in some instances, this study is however going to dwell on the positive correlation between these two variables. -
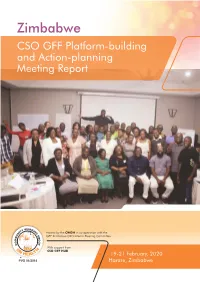
CSO GFF Platform-Building and Action-Planning Meeting Report
Zimbabwe CSO GFF Platform-building and Action-planning Meeting Report Hosted by the CWGH in co-operation with the GFF Zimbabwe CSO Interim Steering Committee With support from CSO GFF HUB 19-21 February, 2020 PVO 01/2014 Harare, Zimbabwe Contents I. Background 1 II. Health Sector Investment Case & GFF Process in Zimbabwe 2 III. The HSIC We Want 5 IV. Coalition structure & leadership 7 V. Next steps 12 Appendix 1: Programme 13 Appendix 2: List of Participants 18 Zimbabwe CSO GFF Platform-building and Action-planning Meeting ound I. Background r Backg Zimbabwe joined the GFF in July 2019 to improve the health and nutrition of Zimbabwean people. The Government of Zimbabwe through the Ministry of Health and Child Care (MOHCC) is currently leading the GFF process. The experience of GFF countries has shown that civil society is most effective when it is structured and coordinated in a coalition. Through forming a new GFF CSO Platform, or designating an existing platform for engagement on GFF, Zimbabwean civil society can be stronger together. Civil society can collectively dene priorities to share information, ensure that policy and program “asks” by different members of the platform are mutually reinforcing and emphasize shared concerns, and streamline engagement with government and donors. A small team of Zimbabwean civil society organizations working in the health sector formed an interim coalition steering committee: CWGH, supported by Zimbabwe AIDS Network (ZAN), Women’s Action Group (WAG), and The Centre for Sexual Health and HIV/AIDS Research Zimbabwe (CeSHHAR Zimbabwe). This group worked with the CSO GFF Resource and Engagement Hub to design a workshop to orient Zimbabwean health civil society organizations to the GFF, and develop plans to engage in the process.