Zimbabwe HIV Care and Treatment Project Baseline Assessment Report
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Midlands Province Mobile Voter Registration Centres
Midlands Province Mobile Voter Registration Centres Chirumhanzu District Team 1 Ward Centre Dates 18 Mwire primary school 10/06/13-11/06/13 18 Tokwe 4 clinic 12/06/13-13/06/13 18 Chingegomo primary school 14/06/13-15/06/13 16 Chishuku Seondary school 16/06/13-18/06/13 9 Upfumba Secondary school 19/06/13-21/06/13 3 Mutya primary school 22/06/13-24/06/13 2 Gonawapotera secondary school 25/06/13-27/06/13 20 Wildegroove primary school 28/06/13-29/06/13 15 Kushinga primary school 30/06/13-02/07/13 12 Huchu compound 03/07/13-04/-07/13 12 Central estates HQ 5/7/13 20 Mtao/Fair Field compound 6/7/13 12 Chiudza homestead 07/07/13-08/06/13 14 Njerere primary school 9/7/13 Team 2 Ward Centre Dates 22 Hillview Secondary school 10/07/13-12/07/13 17 Lalapanzi Secondary school 13/07/13-15/07/13 16 Makuti homestead 16/06/13-17/06/13 1 Mapiravana Secondary school 18/06/13-19/06/13 9 Siyahukwe Secondary school 20/06/13-23/06/13 4 Chizvinire primary school 24/06/13-25/06/13 21 Mukomberana Seconadry school 26/06/13-29/06/13 20 Union primary school 30/06/13-01/07/13 15 Nyikavanhu primary school 02/07/13-03/07/13 19 Musens primary school 04/07/13-06/07/13 16 Utah primary school 07/7/13-09/07/13 Team 3 Ward Centre Dates 11 Faerdan primary school 10/07/13-11/07/13 11 Chamakanda Secondary school 12/07/13-14/07/13 11 Chamakanda primary school 15/07/13-16/07/13 5 Chizhou Secondary school 17/06/13-16/06/13 3 Chilimanzi primary school 21/06/13-23/06/13 25 Maponda primary school 24/06/13-25/06/13 6 Holy Cross seconadry school 26/06/13-28/06/13 20 New England Secondary -

(Ports of Entry and Routes) (Amendment) Order, 2020
Statutory Instrument 55 ofS.I. 2020. 55 of 2020 Customs and Excise (Ports of Entry and Routes) (Amendment) [CAP. 23:02 Order, 2020 (No. 20) Customs and Excise (Ports of Entry and Routes) (Amendment) “THIRTEENTH SCHEDULE Order, 2020 (No. 20) CUSTOMS DRY PORTS IT is hereby notifi ed that the Minister of Finance and Economic (a) Masvingo; Development has, in terms of sections 14 and 236 of the Customs (b) Bulawayo; and Excise Act [Chapter 23:02], made the following notice:— (c) Makuti; and 1. This notice may be cited as the Customs and Excise (Ports (d) Mutare. of Entry and Routes) (Amendment) Order, 2020 (No. 20). 2. Part I (Ports of Entry) of the Customs and Excise (Ports of Entry and Routes) Order, 2002, published in Statutory Instrument 14 of 2002, hereinafter called the Order, is amended as follows— (a) by the insertion of a new section 9A after section 9 to read as follows: “Customs dry ports 9A. (1) Customs dry ports are appointed at the places indicated in the Thirteenth Schedule for the collection of revenue, the report and clearance of goods imported or exported and matters incidental thereto and the general administration of the provisions of the Act. (2) The customs dry ports set up in terms of subsection (1) are also appointed as places where the Commissioner may establish bonded warehouses for the housing of uncleared goods. The bonded warehouses may be operated by persons authorised by the Commissioner in terms of the Act, and may store and also sell the bonded goods to the general public subject to the purchasers of the said goods paying the duty due and payable on the goods. -

Bulawayo City Mpilo Central Hospital
Province District Name of Site Bulawayo Bulawayo City E. F. Watson Clinic Bulawayo Bulawayo City Mpilo Central Hospital Bulawayo Bulawayo City Nkulumane Clinic Bulawayo Bulawayo City United Bulawayo Hospital Manicaland Buhera Birchenough Bridge Hospital Manicaland Buhera Murambinda Mission Hospital Manicaland Chipinge Chipinge District Hospital Manicaland Makoni Rusape District Hospital Manicaland Mutare Mutare Provincial Hospital Manicaland Mutasa Bonda Mission Hospital Manicaland Mutasa Hauna District Hospital Harare Chitungwiza Chitungwiza Central Hospital Harare Chitungwiza CITIMED Clinic Masvingo Chiredzi Chikombedzi Mission Hospital Masvingo Chiredzi Chiredzi District Hospital Masvingo Chivi Chivi District Hospital Masvingo Gutu Chimombe Rural Hospital Masvingo Gutu Chinyika Rural Hospital Masvingo Gutu Chitando Rural Health Centre Masvingo Gutu Gutu Mission Hospital Masvingo Gutu Gutu Rural Hospital Masvingo Gutu Mukaro Mission Hospital Masvingo Masvingo Masvingo Provincial Hospital Masvingo Masvingo Morgenster Mission Hospital Masvingo Mwenezi Matibi Mission Hospital Masvingo Mwenezi Neshuro District Hospital Masvingo Zaka Musiso Mission Hospital Masvingo Zaka Ndanga District Hospital Matabeleland South Beitbridge Beitbridge District Hospital Matabeleland South Gwanda Gwanda Provincial Hospital Matabeleland South Insiza Filabusi District Hospital Matabeleland South Mangwe Plumtree District Hospital Matabeleland South Mangwe St Annes Mission Hospital (Brunapeg) Matabeleland South Matobo Maphisa District Hospital Matabeleland South Umzingwane Esigodini District Hospital Midlands Gokwe South Gokwe South District Hospital Midlands Gweru Gweru Provincial Hospital Midlands Kwekwe Kwekwe General Hospital Midlands Kwekwe Silobela District Hospital Midlands Mberengwa Mberengwa District Hospital . -

CHAPTER 10: Restructuring and Recovery in Railway Services
CHAPTER 10: Restructuring and Recovery in Railway Services 10.1 OVERVIEW OF Republic of Congo (DRC) (See Map 10.1). THE SECTOR As a result, the national railway of Zimbabwe has been critical to the growth of the country’s domestic, regional, and international trade as 10.1.1 The Setting it connects all major economic centers and Although continental rail master plans have provides transport for bulk raw materials, existed for more than a century, most of the fi nished goods, and passengers. As in most African railway network remains disconnected, other African countries, the Zimbabwean operating within a single country, or linking railway system served as a primary conduit a port and its immediate regional hinterland. for agricultural and other natural resources The only signifi cant international network is and this largely accounts for the standards and centered in South Africa and stretches north routing that were adopted. to Zimbabwe, Zambia, and the Democratic Map 10.1: Railway Network for the Southern Africa Region Within Zimbabwe, the railway network and its ports of Durban, Richards Bay, and Port connects all major mines and heavy industrial Elizabeth. It is also at the centre of shorter and plants, as well as major collection points for cost-effective railroad links between Malawi farms. The system has three well connected and South Africa through Bulawayo, the port hubs, Bulawayo, Gweru, and Harare (See of Beira through Harare, and Lusaka and the Map 10.2). The railway is at the centre of the port of Durban through Bulawayo. The -

The Spatial Dimension of Socio-Economic Development in Zimbabwe
THE SPATIAL DIMENSION OF SOCIO-ECONOMIC DEVELOPMENT IN ZIMBABWE by EVANS CHAZIRENI Submitted in fulfillment of the requirements for the degree of MASTER OF ARTS in the subject GEOGRAPHY at the UNIVERSITY OF SOUTH AFRICA SUPERVISOR: MRS AC HARMSE NOVEMBER 2003 1 Table of Contents List of figures 7 List of tables 8 Acknowledgements 10 Abstract 11 Chapter 1: Introduction, problem statement and method 1.1 Introduction 12 1.2 Statement of the problem 12 1.3 Objectives of the study 13 1.4 Geography and economic development 14 1.4.1 Economic geography 14 1.4.2 Paradigms in Economic Geography 16 1.4.3 Development paradigms 19 1.5 The spatial economy 21 1.5.1 Unequal development in space 22 1.5.2 The core-periphery model 22 1.5.3 Development strategies 23 1.6 Research design and methodology 26 1.6.1 Objectives of the research 26 1.6.2 Research method 27 1.6.3 Study area 27 1.6.4 Time period 30 1.6.5 Data gathering 30 1.6.6 Data analysis 31 1.7 Organisation of the thesis 32 2 Chapter 2: Spatial Economic development: Theory, Policy and practice 2.1 Introduction 34 2.2. Spatial economic development 34 2.3. Models of spatial economic development 36 2.3.1. The core-periphery model 37 2.3.2 Model of development regions 39 2.3.2.1 Core region 41 2.3.2.2 Upward transitional region 41 2.3.2.3 Resource frontier region 42 2.3.2.4 Downward transitional regions 43 2.3.2.5 Special problem region 44 2.3.3 Application of the model of development regions 44 2.3.3.1 Application of the model in Venezuela 44 2.3.3.2 Application of the model in South Africa 46 2.3.3.3 Application of the model in Swaziland 49 2.4. -

Promotion of Climate-Resilient Lifestyles Among Rural Families in Gutu
Promotion of climate-resilient lifestyles among rural families in Gutu (Masvingo Province), Mutasa (Manicaland Province) and Shamva (Mashonaland Central Province) Districts | Zimbabwe Sahara and Sahel Observatory 26 November 2019 Promotion of climate-resilient lifestyles among rural families in Gutu Project/Programme title: (Masvingo Province), Mutasa (Manicaland Province) and Shamva (Mashonaland Central Province) Districts Country(ies): Zimbabwe National Designated Climate Change Management Department, Ministry of Authority(ies) (NDA): Environment, Water and Climate Development Aid from People to People in Zimbabwe (DAPP Executing Entities: Zimbabwe) Accredited Entity(ies) (AE): Sahara and Sahel Observatory Date of first submission/ 7/19/2019 V.1 version number: Date of current submission/ 11/26/2019 V.2 version number A. Project / Programme Information (max. 1 page) ☒ Project ☒ Public sector A.2. Public or A.1. Project or programme A.3 RFP Not applicable private sector ☐ Programme ☐ Private sector Mitigation: Reduced emissions from: ☐ Energy access and power generation: 0% ☐ Low emission transport: 0% ☐ Buildings, cities and industries and appliances: 0% A.4. Indicate the result ☒ Forestry and land use: 25% areas for the project/programme Adaptation: Increased resilience of: ☒ Most vulnerable people and communities: 25% ☒ Health and well-being, and food and water security: 25% ☐ Infrastructure and built environment: 0% ☒ Ecosystem and ecosystem services: 25% A.5.1. Estimated mitigation impact 399,223 tCO2eq (tCO2eq over project lifespan) A.5.2. Estimated adaptation impact 12,000 direct beneficiaries (number of direct beneficiaries) A.5. Impact potential A.5.3. Estimated adaptation impact 40,000 indirect beneficiaries (number of indirect beneficiaries) A.5.4. Estimated adaptation impact 0.28% of the country’s total population (% of total population) A.6. -

Crop Area, Condition and Stage
Foreword The Government of Zimbabwe has continued to exhibit its commitment for reducing food and nutrition insecurity in Zimbabwe. Evidence include the culmination of ZimASSET’s Food and Nutrition Security Cluster and the multi-sector Food and Nutrition Security Policy (FNSP). Recognising the vagaries of climate variabilities and the unforeseeable potential livelihood challenges, Government put in place structures whose mandates are, among other things to provide early warning information for early actioning. The Food and Nutrition Council, through the ZimVAC, is one of such structures which strives to fulfil the aspirations of the FNSP’s commitment number 6 of providing food and nutrition early warning information. In response to the advent of the El Nino phenomena which has resulted in the country experiencing long dry spells, the ZimVAC undertook a rapid assessment focussing on updating the ZimVAC May 2015 results. The lean season monitoring focused on the relevant food and nutrition security parameters. The process followed a 3 pronged approach which were, a review of existing food and nutrition secondary data, qualitative district Focus Group Discussions (FGDs) and for other variables a quantitative household survey which in most cases are representative at provincial and national level. This report provides a summation of the results for the 3 processes undertaken and focuses on the following thematic areas: the rainfall season quality, 2015/16 agricultural assistance, crop and livestock condition, food and livestock markets, gender based violence, household income sources and livelihoods strategies, domestic and production water situation, health and nutrition, food assistance and a review of the rural food security projections. -
Zimbabwe Return Intention Survey July 2021
ZIMBABWE RETURN INTENTION SURVEY JULY 2021 Contents Overview .................................................................................................................................................................... 2 Methodology............................................................................................................................................................. 2 Map Of Chimanimani District And Idps Assessed By Ward ....................................................................... 3 Current Livelihoods ............................................................................................................................................... 3 Shelter ....................................................................................................................................................................... 3 Food, Water And Education ............................................................................................................................... 4 Wash And Health ................................................................................................................................................... 4 Intentions ................................................................................................................................................................. 5 Vulnerabilities .......................................................................................................................................................... 5 Support Received .................................................................................................................................................. -

1 Research Application Summary Evaluating the Level of Adoption Of
Research Application Summary Evaluating the level of adoption of improved agrosilvopastoral technologies, factors affecting adoption and establishing the species and systems adopted among small holder farmers of Buhera and Mutasa Districts of Manicaland Province, Zimbabwe Chihota B.P., Mupanda K., Mrema M., Tagwira F. & Ajayi O.C. Background Two thirds of the rural populations in most countries of Sub-Saharan Africa subsist on less than US$1 a day. The farmers’ economies have weak linkages to the markets and they have little or no access to external inputs. The increasing cost of inputs and high transport costs make external inputs unaffordable for the smallholder farmer (Spencer, 2002). Inorganic fertilizer use has declined to 8kg/ha (NEPAD, 2006). Smallholder farmers cannot afford stock feeds for supplementing limited and poor quality pasture during the dry and cold season. Land degradation and siltation are an environmental concern that also reduces yields (Rattsø, 1996). Crop and livestock yields are low and declining. Countries like Zimbabwe, Malawi, Zambia, Mozambique and Botswana are affected and as a result, food insecure (Bohringer, 2002). Some agroforestry technologies have been shown to improve the soil and animal fodder availability (Dzowela, 1994; Govere, 2003). Agroforestry can improve crop and livestock production by providing relatively less costly, more affordable and locally available inputs for fodder and soil amendments to the smallholder farmer. Government departments and non-governmental organizations (NGOs) like World Agroforestry Centre (WAC) are scaling up agroforestry through training and distributing germplasm to the smallholder farmers in the region. Not much has been done on assessment of adoption and factors that affect adoption of agroforestry in different geographical areas and agricultural sectors in Zimbabwe. -
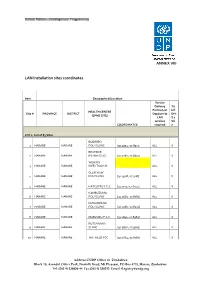
LAN Installation Sites Coordinates
ANNEX VIII LAN Installation sites coordinates Item Geographical/Location Service Delivery Tic Points (List k if HEALTH CENTRE Site # PROVINCE DISTRICT Dept/umits DHI (EPMS SITE) LAN S 2 services Sit COORDINATES required e LOT 1: List of 83 Sites BUDIRIRO 1 HARARE HARARE POLYCLINIC [30.9354,-17.8912] ALL X BEATRICE 2 HARARE HARARE RD.INFECTIO [31.0282,-17.8601] ALL X WILKINS 3 HARARE HARARE INFECTIOUS H ALL X GLEN VIEW 4 HARARE HARARE POLYCLINIC [30.9508,-17.908] ALL X 5 HARARE HARARE HATCLIFFE P.C.C. [31.1075,-17.6974] ALL X KAMBUZUMA 6 HARARE HARARE POLYCLINIC [30.9683,-17.8581] ALL X KUWADZANA 7 HARARE HARARE POLYCLINIC [30.9285,-17.8323] ALL X 8 HARARE HARARE MABVUKU P.C.C. [31.1841,-17.8389] ALL X RUTSANANA 9 HARARE HARARE CLINIC [30.9861,-17.9065] ALL X 10 HARARE HARARE HATFIELD PCC [31.0864,-17.8787] ALL X Address UNDP Office in Zimbabwe Block 10, Arundel Office Park, Norfolk Road, Mt Pleasant, PO Box 4775, Harare, Zimbabwe Tel: (263 4) 338836-44 Fax:(263 4) 338292 Email: [email protected] NEWLANDS 11 HARARE HARARE CLINIC ALL X SEKE SOUTH 12 HARARE CHITUNGWIZA CLINIC [31.0763,-18.0314] ALL X SEKE NORTH 13 HARARE CHITUNGWIZA CLINIC [31.0943,-18.0152] ALL X 14 HARARE CHITUNGWIZA ST.MARYS CLINIC [31.0427,-17.9947] ALL X 15 HARARE CHITUNGWIZA ZENGEZA CLINIC [31.0582,-18.0066] ALL X CHITUNGWIZA CENTRAL 16 HARARE CHITUNGWIZA HOSPITAL [31.0628,-18.0176] ALL X HARARE CENTRAL 17 HARARE HARARE HOSPITAL [31.0128,-17.8609] ALL X PARIRENYATWA CENTRAL 18 HARARE HARARE HOSPITAL [30.0433,-17.8122] ALL X MURAMBINDA [31.65555953980,- 19 MANICALAND -

Tendayi Mutimukuru-Maravanyika Phd Thesis
Can We Learn Our Way to Sustainable Management? Adaptive Collaborative Management in Mafungautsi State Forest, Zimbabwe. Tendayi Mutimukuru-Maravanyika Thesis committee Thesis supervisors Prof. dr. P. Richards Professor of Technology and Agrarian Development Wageningen University Prof. dr. K.E. Giller Professor of Plant Production Systems Wageningen University Thesis co-supervisor Dr. ir. C. J. M. Almekinders Assistant Professor, Technology and Agrarian Development Group Wageningen University Other members Prof. dr. ir. C. Leeuwis, Wageningen University Prof. dr. L.E. Visser, Wageningen University Dr. ir. K. F. Wiersum, Wageningen University Dr. B.B. Mukamuri, University of Zimbabwe This research was conducted under the auspices of the CERES Research School for Resource Studies for Development. Can We Learn Our Way to Sustainable Management? Adaptive Collaborative Management in Mafungautsi State Forest, Zimbabwe. Tendayi Mutimukuru-Maravanyika Thesis submitted in fulfilment of the requirements for the degree of doctor at Wageningen University by the authority of the Rector Magnificus Prof. dr. M. J. Kropff in the presence of the Thesis Committee appointed by the Academic Board to be defended in public on Friday 23 April 2010 at 11 a.m. in the Aula. Tendayi Mutimukuru-Maravanyika Can We Learn Our Way to Sustainable Management? Adaptive Collaborative Management in Mafungautsi State Forest, Zimbabwe. 231 pages Thesis Wageningen University, Wageningen, NL (2010) ISBN 978-90-8585-651-1 Dedication To my parents, my husband Simeon , my son Tafadzwa -

Zimbabwe-HIV-Estimates Report 2018
ZIMBABWE NATIONAL AND SUB-NATIONAL HIV ESTIMATES REPORT 2017 AIDS & TB PROGRAMME MINISTRY OF HEALTH AND CHILD CARE July 2018 Foreword The Ministry of Health and Child Care (MOHCC) in collaboration with National AIDS Council (NAC) and support from partners, produced the Zimbabwe 2017 National, Provincial and District HIV and AIDS Estimates. The UNAIDS, Avenir Health and NAC continued to provide technical assistance and training in order to build national capacity to produce sub-national estimates in order to track the epidemic. The 2017 Estimates report gives estimates for the impact of the programme. It provide an update of the HIV and AIDS estimates and projections, which include HIV prevalence and incidence, programme coverages, AIDS-related deaths and orphans, pregnant women in need of PMTCT services in the country based on the Spectrum Model version 5.63. The 2017 Estimates report will assist the country to monitor progress towards the fast track targets by outlining programme coverage and possible gaps. This report will assist programme managers in accounting for efforts in the national response and policy makers in planning and resource mobilization. Brigadier General (Dr.) G. Gwinji Permanent Secretary for Health and Child Care Page | i Acknowledgements The Ministry of Health and Child Care (MOHCC) would want to acknowledge effort from all individuals and organizations that contributed to the production of these estimates and projections. We are particularly grateful to the National AIDS Council (NAC) for funding the national and sub-national capacity building and report writing workshop. We are also grateful to the National HIV and AIDS Estimates Working Group for working tirelessly to produce this report.