Histamine and Antihistamines
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Download Large Text CMI (PDF)
Children's Paedamin Antihistamine Oral Liquid Decongestant and Antihistamine Children 6-12 years Consumer Medicine Information What is in this leaflet? • Itchy, watery eyes Before you give • Nasal congestion Children's Paedamin This leaflet answers some common Children's Paedamin Decongestant Decongestant and questions about Children's and Antihistamine contains Antihistamine Paedamin® Decongestant and Diphenhydramine Hydrochloride Antihistamine. and Phenylephrine Hydrochloride. When you must not give it It does not contain all the available Diphenhydramine Hydrochloride Do not use Children's Paedamin information. It does not take the belongs to a group of medicines Decongestant and Antihistamine if place of talking to your doctor or called 'antihistamines'. you/ your child have an allergy to: pharmacist. Antihistamines help reduce allergic All medicines have risks and symptoms, such as sneezing, runny • any medicine containing benefits. Your doctor or pharmacist nose or itchy, watery eyes, by Diphenhydramine has weighed the risks of you/your preventing the effects of a substance Hydrochloride or other child taking Children's Paedamin called histamine. Histamine is antihistamines Decongestant and Antihistamine produced by the body in response to • any medicine containing against the benefits they expect it foreign substances that the body is Phenylephrine Hydrochloride will have for you. allergic to. • any of the ingredients listed at If you have any concerns about Phenylephrine Hydrochloride the end of this leaflet taking this medicine, ask your belongs to a group of medicines Some of the symptoms of an doctor or pharmacist. called decongestants. allergic reaction may include: Keep this leaflet with the It works by reducing congestion in • shortness of breath medicine. -
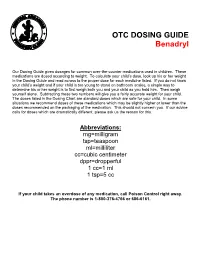
OTC DOSING GUIDE Benadryl
OTC DOSING GUIDE Benadryl Our Dosing Guide gives dosages for common over-the-counter medications used in children. These medications are dosed according to weight. To calculate your child’s dose, look up his or her weight in the Dosing Guide and read across to the proper dose for each medicine listed. If you do not know your child’s weight and if your child is too young to stand on bathroom scales, a simple way to determine his or her weight is to first weigh both you and your child as you hold him. Then weigh yourself alone. Subtracting these two numbers will give you a fairly accurate weight for your child. The doses listed in the Dosing Chart are standard doses which are safe for your child. In some situations we recommend doses of these medications which may be slightly higher or lower than the doses recommended on the packaging of the medication. This should not concern you. If our advice calls for doses which are dramatically different, please ask us the reason for this. Abbreviations: mg=milligram tsp=teaspoon ml=milliliter cc=cubic centimeter dppr=dropperful 1 cc=1 ml 1 tsp=5 cc If your child takes an overdose of any medication, call Poison Control right away. The phone number is 1-800-376-4766 or 686-6161. CHILDREN’S BENADRYL ALLERGY LIQUID (Generic Name: Diphenhydramine) (Antihistamine) NEVER GIVE TO INFANTS LESS THAN 6 MONTHS OLD. DO NOT GIVE TO CHILDREN LESS THAN 2 YEARS OLD UNLESS ADVISED BY A PHYSICIAN. Dosage: Every 4 -6 hours. -
Doxylamine Succinate-Pyridoxine Hydrochloride
Doxylamine succinate-pyridoxine hydrochloride This sheet is about exposure to doxylamine succinate-pyridoxine hydrochloride in pregnancy and while breastfeeding. This information should not take the place of medical care and advice from your healthcare providers. What is doxylamine succinate-pyridoxine hydrochloride? The combination of 10mg of doxylamine succinate and 10mg of pyridoxine hydrochloride is a medication used to treat nausea and vomiting of pregnancy (NVP), also called “morning sickness.” For more information on NVP, please see the MotherToBaby fact sheet Nausea and Vomiting of Pregnancy (https://mothertobaby.org/fact-sheets/nausea-vomiting-pregnancy-nvp/pdf/). Doxylamine succinate is an antihistamine. Antihistamines lessen the symptoms of allergic reactions and colds and help to treat insomnia (hard time sleeping). Pyridoxine hydrochloride is a form of vitamin B6. In the United States, the combination of doxylamine and pyridoxine has been sold under the name Diclegis® since 2013. In Canada, it has been sold under the brand name Diclectin®. Diclegis® and Diclectin® are delayed-release tablets available by prescription. Delayed-release means that the tablet coating prevents the ingredients from being absorbed too quickly by the body. Doxylamine succinate and/or pyridoxine hydrochloride may also be available as over-the- counter medicines. I take doxylamine succinate-pyridoxine hydrochloride. Can it make it harder for me to get pregnant? Based on the data available, it is not known if doxylamine succinate-pyridoxine hydrochloride can make it harder to become pregnant. I just found out I am pregnant. Should I stop taking doxylamine succinate-pyridoxine hydrochloride? Talk with your healthcare providers before making any changes to how you take your medication(s). -

Doxylamine/Pyridoxine
BonjestaTM (doxylamine/pyridoxine) – New Drug Approval • On November 7, 2016, the FDA approved Duchesnay’s Bonjesta (doxylamine/pyridoxine) for the treatment of nausea and vomiting of pregnancy in women who do not respond to conservative management. — Bonjesta has not been studied in women with hyperemesis gravidarum. • Bonjesta is a fixed dose combination product containing an antihistamine (doxylamine) and a vitamin B6 analog (pyridoxine). The exact mechanism of Bonjesta is not known. — Doxylamine/pyridoxine is also available as Diclegis®, which contains 10 mg of doxylamine and 10 mg of pyridoxine as delayed-release tablets for the same indication. • There have been no efficacy and safety trials for Bonjesta. However, a placebo-controlled study was conducted to support the safety and efficacy of 10 mg doxylamine succinate and 10 mg pyridoxine hydrochloride tablets (a different formulation and dosage strength than Bonjesta) in the treatment of nausea and vomiting of pregnancy. • Bonjesta is contraindicated in women with known hypersensitivity to doxylamine, other ethanolamine derivative antihistamines, or pyridoxine or any inactive ingredient in the formulation; monoamine oxidase (MAO) inhibitors intensify and prolong the adverse central nervous system effects of Bonjesta. • Warnings and precautions of Bonjesta include somnolence and concomitant medical conditions. • The most common adverse event (≥ 5% and exceeding placebo) with combination 10 mg doxylamine and 10 mg pyridoxine tablets was somnolence. • The recommended dose of Bonjesta is one tablet orally at bedtime on day 1. If the dose adequately controls symptoms the next day, the patient may continue taking one tablet daily at bedtime only. However, if symptoms persist on day 2, the dose may be increased to one tablet in the morning and one tablet at bedtime. -

Doxepin (Dox-E-Pin) Description: Tricyclic Antidepressant; Antihistamine Other Names for This Medication: Sinequan®, Silenor® Common Dosage Forms: Veterinary: None
Prescription Label Patient Name: Species: Drug Name & Strength: Directions (amount to give how often & for how long): Prescribing Veterinarian's Name & Contact Information: Refills: [Content to be provided by prescribing veterinarian] Doxepin (dox-e-pin) Description: Tricyclic Antidepressant; Antihistamine Other Names for this Medication: Sinequan®, Silenor® Common Dosage Forms: Veterinary: None. Human: 3 mg, 6 mg, 10 mg, 25 mg, 50 mg, 75 mg, 100 mg, & 150 mg capsules; 10 mg/mL oral liquid concentrates. This information sheet does not contain all available information for this medication. It is to help answer commonly asked questions and help you give the medication safely and effectively to your animal. If you have other questions or need more information about this medication, contact your veterinarian or pharmacist. Key Information When used as an antihistamine, doxepin should be used on a regular, ongoing basis in animals that respond to it. This drug works better if used before exposure to an allergen (eg, pollens). When used for behavior modification, it may take several days to weeks to determine if doxepin is effective. May be given with or without food. If your animal vomits or acts sick after receiving the drug on an empty stomach, try giving the next dose with food or a small treat. If vomiting continues, contact your veterinarian. Most common side effects are sleepiness, dry mouth, and constipation. Be sure your animal always has access to plenty of fresh, clean water. Rare side effects that can be serious (contact veterinarian immediately) include abnormal bleeding, lack of an appetite, seizures, collapse, or profound sleepiness. -

Histamine and Antihistamines Sites of Action Conditions Which Cause Release Aron H
Learning Objectives I Histamine Pharmacological effects Histamine and Antihistamines Sites of action Conditions which cause release Aron H. Lichtman, Ph.D. Diagnostic uses Associate Professor II Antihistamines acting at the H1 and H2 receptor Pharmacology and Toxicology Pharmacological effects Mechanisms of action Therapeutic uses Side effects and drug interactions Be familiar with the existence of the H3 receptor III Be able to describe the main mechanism of action of cromolyn sodium and its clinical uses Histamine Pharmacology First autacoid to be discovered. (Greek: autos=self; Histamine Formation akos=cure) Synthesized in 1907 Synthesized in mammalian tissues by Demonstrated to be a natural constituent of decarboxylation of the amino acid l-histidine mammalian tissues (1927) Involved in inflammatory and anaphylactic reactions. Local application causes swelling redness, and edema, mimicking a mild inflammatory reaction. Large systemic doses leads to profound vascular changes similar to those seen after shock or anaphylactic origin Histamine Stored in complex with: Heparin Chondroitin Sulfate Eosinophilic Chemotactic Factor Neutrophilic Chemotactic Factor Proteases 1 Conditions That Release Histamine 1. Tissue injury: Any physical or chemical agent that injures tissue, skin or mucosa are particularly sensitive to injury and will cause the immediate release of histamine from mast cells. 2. Allergic reactions: exposure of an antigen to a previously sensitized (exposed) subject can immediately trigger allergic reactions. If sensitized by IgE antibodies attached to their surface membranes will degranulate when exposed to the appropriate antigen and release histamine, ATP and other mediators. 3. Drugs and other foreign compounds: morphine, dextran, antimalarial drugs, dyes, antibiotic bases, alkaloids, amides, quaternary ammonium compounds, enzymes (phospholipase C). -

Allergy, Depression and Tricyclic Antidepressants
Allergy, Depression and Tricyclic Antidepressants A. Hoffer, M.D., Ph.D.1 INTRODUCTION causes a variety of symptoms of which mood Psychiatrists have been very reluctant to disorder is one. The patient with asthma is not accept the idea that depressions, which they depressed because it is hard to breathe—the know so well, may be caused by allergies to depression and the difficulty in breathing are common environmental molecules such as both expressions of an allergic reaction to one foods, airborne particles, and chemicals in or more foreign types of molecules. water. When patients were depressed and Many years ago allergists recognized that it anxious, and at the same time suffered from was possible to be allergic to foods as well as diseases accepted as allergic, psychosomatic to pollens or dusts, and described the mood explanations were used. This usually meant symptoms which were also present. The that a psychological explanation for the depression and anxiety was recognized as a presence of the allergic reactions was invoked. reaction to the allergen, but prime emphasis The mood disorder was looked upon as a was given to the non-psychiatric symptoms. natural reaction to the discomfort of the Clinical allergists who are now practicing allergic reaction. Asthma for a long time was clinical ecology went one step further when one of the seven major psychosomatic they recognized that allergic reactions could diseases. Most psychiatrists still believe cause depression and anxiety as the main schizophrenic patients can not be allergic, at symptom with minimal somatic reactions. least not when they are ill, but it was accepted Dr. -

Pharmacology of Antihistamines
SYMPOSIUM REPORT SUPPLEMENT Pharmacology of Antihistamines Diana S. Church, MD, and Martin K. Church, PhD, DSc compounds was to measure histamine-induced contractions Abstract: This article reviews the molecular biology of the inter- of pieces of muscle from experimental animals, usually action of histamine with its H -receptor and describes the concept 1 guinea-pig intestine, suspended in an organ bath. Candidate that H1-antihistamines are not receptor antagonists but are inverse agonists i.e. they produce the opposite effect on the receptor to hista- antihistaminic compounds were primarily modifications of those synthesized as cholinergic antagonists and are from mine. It then discourages the use of first-generation H1-antihistamines in clinical practice today for two main reasons. First, they are less diverse chemical entities, ethanolamines, ethylene diamines, alkylamines, piperazines, piperidines, and phenothiazines. It effective than second generation H1-antihistamines. Second, they have unwanted side effects, particularly central nervous system and is hardly surprising, therefore, that these first-generation an- anti-cholinergic effects, and have the potential for causing severe tihistamines had poor receptor selectivity and significant unwanted side effects. toxic reactions which are not shared by second-generation H1- antihistamines. There are many efficacious and safe second-gener- During this time, knowledge of the nature and diversity of receptors was rudimentary to say the least and it was only ation H1-antihistamines on the market for the treatment of allergic disease. Of the three drugs highlighted in this review, levocetirizine several decades later that the existence of more than one and fexofenadine are the most efficacious in humans in vivo. -

Brief Report
Brief Report Histamine 2 blocker potentiates the effects of histamine 1 blocker in suppressing histamine-induced wheal N. B. Dhanya, Reena Rai, C. R. Srinivas Department of Dermatology, PSG Hospitals, Coimbatore, India Address for correspondence: Dr. Reena Rai, Department of Dermatology, PSG Hospitals, Peelamedu, Coimbatore - 641 004, Tamil Nadu, India. E-mail: [email protected] ABSTRACT Background: Histamine is responsible for the wheal and flare reaction in various allergic conditions. Classical antihistamines are the drugs which block the H1 receptors and are widely used in various allergic conditions, whereas H2 blockers are mainly used for acid peptic disease. Although H1 receptor-mediated actions of histamine are primarily responsible for vasodilatation, vasopermeability, and itching, it has been observed that combined blocking of both H1 and H2 receptors may provide better relief. Aim: To compare the efficacy of levocetirizine (H1 blocker) versus levocetirizine and ranitidine (H2blocker) in suppressing histamine-induced wheal. Methods: Fifteen volunteers were given a single dose of levocetirizine 5 mg on day 1 and a single dose of levocetirizine 5 mg with ranitidine 150 mg twice a day on day 7. A pretest was performed by intradermal histamine prick test. After administration of the drugs, the prick test was repeated at 1 hour, 2, 3, 6, and 24 hours, and the size of the wheal measured and statistically analyzed. Results: At 1 hour, there was no statistically significant difference in the wheal size between levocetirizine alone and the combination of levocetirizine and ranitidine. Levocetirizine with ranitidine resulted in statistically significant reduction of wheal size at 2, 3, 6, and 24 hours when compared with levocetirizine alone. -

Diphenhydramine and Pregnancy
Diphenhydramine This sheet is about exposure to diphenhydramine in pregnancy and while breastfeeding. This information should not take the place of medical care and advice from your healthcare providers. What is diphenhydramine? Diphenhydramine is an antihistamine. It is found in many medications, both prescription and over-the-counter. It is commonly used to treat allergy symptoms, and may also be used to treat nausea, motion sickness, insomnia, itchy skin, and tremor of Parkinson’s disease. Some brand names for diphenhydramine include: Benadryl®, Unisom®, Sominex®, or Nytol®. I take diphenhydramine. Can it make it harder for me to get pregnant? It is not known if diphenhydramine can make it harder to become pregnant. I just found out I am pregnant. Should I stop taking diphenhydramine? You should talk with your healthcare provider before making any changes to how you take your medication. It is important to consider the benefits of treating your condition during pregnancy. Does taking diphenhydramine increase the chance for miscarriage? Miscarriage can occur in any pregnancy. The results from one study did not show an increased chance of miscarriage with the use of antihistamines, including diphenhydramine, in early pregnancy. Does taking diphenhydramine increase the chance of birth defects? Every pregnancy starts out with a 3-5% chance of having a birth defect. This is called the background risk. A few studies have suggested a higher chance for birth defects when diphenhydramine is used during the first trimester. However, these studies do not all agree and no consistent pattern of birth defects has been noted. In addition, several studies showed no increased chance of birth defects with the use of diphenhydramine in early pregnancy. -

Antihistamines
Leaders In Allergy & Asthma Care For Over 40 Years Antihistamines Actions: Antihistamines are medications which block the effects of histamine, which is released by allergy cells during allergic reactions. Types: There are many different brands of antihistamines. They are commonly used as capsules, tablets (swallowed or dissolvable), and liquids, all of which are taken by mouth. Most antihistamines are currently available OTC (over‐the‐counter); However there are a few that are still available only by prescription. The older antihistamines (1st generation) are typically more sedating and shorter acting. The newer antihistamines (2nd generation) are less sedating and longer acting. Examples of Antihistamines: 1st Generation: Atarax (hydroxyzine), Benadryl (diphenhydramine), Chlor‐Trimeton (chlorpheniramine), Doxepin, Tavist (clemastine), and Periactin (cyproheptadine). 2nd Generation: Allegra (fexofenadine), Claritin (loratadine), Clarinex (desloratadine), Zyrtec (cetirizine), and Xyzal (levocetirizine). Side Effects: Sedation and dryness are the most common side effects of antihistamines. These effects can occur with either 1st or 2nd generation antihistamines however, it is far more of an issue with the 1st generation antihistamines. Alcohol, tranquilizers, and other sedating medications may increase the sedative effects of antihistamines. If an antihistamine is combined with a decongestant, side effects may include nervousness, insomnia, irritability, palpitations, rapid heart beat. Consult your prescribing doctor if these side effects occur. Special Instructions: ● Notify your doctor if you: ○ Are pregnant or breast‐feeding ○ Have glaucoma ○ Have prostate problems ○ Have liver disease ○ Have a heart condition or high blood pressure ● Chronic hives: Your provider will frequently prescribe antihistamines at higher doses than is recommended on package labeling. ● Notify your provider of all other medications you are taking (prescription and OTC), since drug interactions or over‐dosages may occur. -

Medication Instructions for Allergy Patients
MEDICATION INSTRUCTIONS FOR ALLERGY PATIENTS Drugs which contain antihistamine or have antihistaminic effects can result in negative reactions to skin testing. As a result, it may not be possible to properly interpret skin test results, and testing may have to be repeated at a later date. While this list is extensive, it is NOT all inclusive (particularly of the various brand names). Discontinue ALL antihistamines including the following medications seven (7) days prior to skin testing (unless longer time specified): Antihistamines – Generic name (Brand name(s)): Cetirizine (Zyrtec, Zyrtec-D) Hydroxyzine (Vistaril, Atarax) Desloratidine (Clarinex) Levocetirizine (Xyzal) Fexofenadine (Allegra, Allegra-D) Loratidine (Claritin, Claritin-D, Alavert) Diphenhydramine (Aleve PM, Benadryl, Bayer P.M., Benylin, Contac P.M., Doans P.M, Excedrin PM, Legatrin P.M.. Nytol, Tylenol Nighttime, Unisom, Zzzquil) Chlorpheniramine (Aller-Chlor, Allerest, Alka Seltzer Plus, Chlor-Trimeton, Comtrex, Contac, Co-Pyronil, Coricidin, CTM, Deconamine, Dristan, Dura-tap, Naldecon, Ornade Spansules, Rondec, Sinutab, Teldrin, Triaminic, Triaminicin, Tylenol Allergy) Azatadine (Optimine, Trinalin) Doxylamine (Nyquil) Brompheniramine (Bromfed, Dimetane, Dimetapp) Meclizine (Antivert) Carbinoxamine (Clistin, Rondec) Pheniramine Clemastine (Tavist) Phenyltoloxamine (Nadecon) Cyclizine (Marezine) Promethazine (Phenergan) Cyprohepatidine (Periactin) (9 days) Pyrilamine (Mepyramine) Dexbrompheniramine (Drixoral) Quinacrine (Atabrine) Dexchlorpheniramine (Extendryl, Polaramine)