Comparative Pharmacology of the H Antihistamines
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Pharmacology
Pharmacology New for 2020-2021 Competitor orientation deleted from ILC. Event Summary Pharmacology provides HOSA members with the opportunity to gain knowledge and skills regarding the area of healthcare concerned with uses, effects, and modes of actions of drugs. This competitive event consists of a written test with a tie-breaker essay question. This event aims to inspire members to learn about how drugs work in the body, proper administration, and adaptations for different patients and conditions. Dress Code Competitors must be in official HOSA uniform or proper business attire. Bonus points will be awarded for proper dress. General Rules 1. Competitors in this event must be active members of HOSA-Future Health Professionals, in good standing. 2. Secondary and Postsecondary/Collegiate divisions are eligible to compete in this event. 3. Competitors must be familiar with and adhere to the “General Rules and Regulations of the HOSA Competitive Events Program (GRR)." 4. All competitors shall report to the site of the event at the time designated for each round of competition. At ILC, competitor’s photo ID must be presented prior to ALL competition rounds. Official References • Fulcher, Soto and Fulcher. Pharmacology: Principles and Applications. Elsevier, Latest edition. • Ford, Susan and Sally Roach. Roach’s Introductory Clinical Pharmacology. Wolters Kluwer, Latest edition. Written Test 5. Test Instructions: The written test will consist of 100 multiple choice items in a maximum of 90 minutes. 6. Time Remaining Announcements: There will be a verbal announcement when there are 60 minutes, 30 minutes, 15 minutes, 5 minutes, and 1 minute remaining to complete the test. -

ADHD Parents Medication Guide Revised July 2013
ADHD Parents Medication Guide Revised July 2013 Attention-Deficit/Hyperactivity Disorder Prepared by: American Academy of Child & Adolescent Psychiatry and American Psychiatric Association Supported by the Elaine Schlosser Lewis Fund Physician: ___________________________________________________ Address: ___________________________________________________ ___________________________________________________ ___________________________________________________ Phone: ___________________________________________________ Email: ___________________________________________________ ADHD Parents Medication Guide – July 2013 2 Introduction Attention-Deficit/Hyperactivity Disorder (ADHD) is a neurodevelopmental disorder characterized by difficulty paying attention, excessive activity, and impulsivity (acting before you think). ADHD is usually identified when children are in grade school but can be diagnosed at any time from preschool to adulthood. Recent studies indicate that almost 10 percent of children between the ages of 4 to 17 are reported by their parents as being diagnosed with ADHD. So in a classroom of 30 children, two to three children may have ADHD.1,2,3,4,5 Short attention spans and high levels of activity are a normal part of childhood. For children with ADHD, these behaviors are excessive, inappropriate for their age, and interfere with daily functioning at home, school, and with peers. Some children with ADHD only have problems with attention; other children only have issues with hyperactivity and impulsivity; most children with ADHD have problems with all three. As they grow into adolescence and young adulthood, children with ADHD may become less hyperactive yet continue to have significant problems with distraction, disorganization, and poor impulse control. ADHD can interfere with a child’s ability to perform in school, do homework, follow rules, and develop and maintain peer relationships. When children become adolescents, ADHD can increase their risk of dropping out of school or having disciplinary problems. -

Clinical Pharmacology 1: Phase 1 Studies and Early Drug Development
Clinical Pharmacology 1: Phase 1 Studies and Early Drug Development Gerlie Gieser, Ph.D. Office of Clinical Pharmacology, Div. IV Objectives • Outline the Phase 1 studies conducted to characterize the Clinical Pharmacology of a drug; describe important design elements of and the information gained from these studies. • List the Clinical Pharmacology characteristics of an Ideal Drug • Describe how the Clinical Pharmacology information from Phase 1 can help design Phase 2/3 trials • Discuss the timing of Clinical Pharmacology studies during drug development, and provide examples of how the information generated could impact the overall clinical development plan and product labeling. Phase 1 of Drug Development CLINICAL DEVELOPMENT RESEARCH PRE POST AND CLINICAL APPROVAL 1 DISCOVERY DEVELOPMENT 2 3 PHASE e e e s s s a a a h h h P P P Clinical Pharmacology Studies Initial IND (first in human) NDA/BLA SUBMISSION Phase 1 – studies designed mainly to investigate the safety/tolerability (if possible, identify MTD), pharmacokinetics and pharmacodynamics of an investigational drug in humans Clinical Pharmacology • Study of the Pharmacokinetics (PK) and Pharmacodynamics (PD) of the drug in humans – PK: what the body does to the drug (Absorption, Distribution, Metabolism, Excretion) – PD: what the drug does to the body • PK and PD profiles of the drug are influenced by physicochemical properties of the drug, product/formulation, administration route, patient’s intrinsic and extrinsic factors (e.g., organ dysfunction, diseases, concomitant medications, -
For Personal Use Only
SedatiWITH ANTIi ® Dowden Health Media CopyrightFor personal use only Initiate the antipsychotic at a reasonable, not overly high dose, then use a nonantipsychotic to help control insomnia, anxiety, and agitation For mass reproduction, content licensing and permissions contact Dowden Health Media. pSYCHIATRY i PSYCHOTICSon edation is a frequent side effect of antipsychot- ics, especially at relatively high doses. Antipsy- S chotics’ sedative effects can reduce agitation in acute psychosis and promote sleep in insomnia, but Manage, don’t long-term sedation may: • interfere with schizophrenia patients’ efforts to go accept adverse to work or school or engage in normal socialization • prevent improvement from psychosocial training, psychiatric rehabilitation, and other treatments. ‘calming’ eff ect This article discusses how to manage acute psycho- sis without oversedation and ways to address persistent sedation and chronic insomnia with less-sedating anti- Del D. Miller, PharmD, MD Professor of psychiatry psychotics or adjunctive medications. University of Iowa Carver College of Medicine Iowa City Neurobiology or psychopharmacology? Many patients experience only mild, transient som- nolence at the beginning of antipsychotic treatment, and most develop some tolerance to the sedating ef- fects with continued administration. Others may have persistent daytime sedation that interferes with nor- mal functioning. Sedation is especially common in elderly patients re- ceiving antipsychotics. Compared with younger patients, older patients receiving -

The Case of Ketamine Allergy
CASE REPORT The Case of Ketamine Allergy William Bylund, MD Department of Emergency Medicine, Naval Medical Center Portsmouth, Portsmouth, Virginia Liam Delahanty, MD Maxwell Cooper, MD Section Editor: Rick A. McPheeters, DO Submission history: Submitted April 3, 2017; Revision received June 29, 2017; Accepted July 11, 2017 Electronically published October 3, 2017 Full text available through open access at http://escholarship.org/uc/uciem_cpcem DOI: 10.5811/cpcem.2017.7.34405 Ketamine is often used for pediatric procedural sedation due to low rates of complications, with allergic reactions being rare. Immediately following intramuscular (IM) ketamine administration, a three-year-old female rapidly developed facial edema and diffuse urticarial rash, with associated wheezing and oxygen desaturation. Symptoms resolved following treatment with epinephrine, dexamethasone and diphenhydramine. This case presents a clinical reaction to ketamine consistent with anaphylaxis due to histamine release, but it is uncertain whether this was immunoglobulin E mediated. This is the only case reported to date of allergic reaction to IM ketamine, without co- administration of other agents. [Clin Pract Cases Emerg Med.2017;1(4):323–325.] INTRODUCTION cardiac monitor, end tidal CO2 (ETCO2) and pulse oximetry Ketamine is a common medication, used in isolation as well (POx), in addition to being placed on two liters nasal cannula as with other agents, for pediatric sedation in the emergency (NC). No intravenous (IV) access was obtained prior to sedation. department (ED). It is often turned to because of its efficacy, ease Seventy milligrams (4.4mg/kg) of ketamine was administered IM of use, and favorable safety profile. Common side effects of into the right thigh. -

Medicines That Affect Fluid Balance in the Body
the bulk of stools by getting them to retain liquid, which encourages the Medicines that affect fluid bowels to push them out. balance in the body Osmotic laxatives e.g. Lactulose, Macrogol - these soften stools by increasing the amount of water released into the bowels, making them easier to pass. Older people are at higher risk of dehydration due to body changes in the ageing process. The risk of dehydration can be increased further when Stimulant laxatives e.g. Senna, Bisacodyl - these stimulate the bowels elderly patients are prescribed medicines for chronic conditions due to old speeding up bowel movements and so less water is absorbed from the age. stool as it passes through the bowels. Some medicines can affect fluid balance in the body and this may result in more water being lost through the kidneys as urine. Stool softener laxatives e.g. Docusate - These can cause more water to The medicines that can increase risk of dehydration are be reabsorbed from the bowel, making the stools softer. listed below. ANTACIDS Antacids are also known to cause dehydration because of the moisture DIURETICS they require when being absorbed by your body. Drinking plenty of water Diuretics are sometimes called 'water tablets' because they can cause you can reduce the dry mouth, stomach cramps and dry skin that is sometimes to pass more urine than usual. They work on the kidneys by increasing the associated with antacids. amount of salt and water that comes out through the urine. Diuretics are often prescribed for heart failure patients and sometimes for patients with The major side effect of antacids containing magnesium is diarrhoea and high blood pressure. -

Histamine and Antihistamines
ACTA FACULTATIS MEDICAE NAISSENSIS UDC: 615.218 DOI: 10.1515/afmnai-2015-0001 Review article Histamine and Antihistamines Nikola Stojković1, Snežana Cekić2, Milica Ristov3, Marko Ristić1, Davor Đukić1, Maša Binić1, Dragan Virijević1 1University of Niš, Faculty of Medicine, PhD student, Serbia 2Institute of Physiology, University of Niš, Faculty of Medicine , Serbia 3Doctor of Medicine SUMMARY In recent years, there has been a steady increase in the prevalence of allergic diseases. Allergic immune response represents a complex network of cellular events involving numerous immune cells and mediators. It represents the interaction of innate and acquired immune response. The key role in the immune cascade is taken by histamine, a natural component of the body, which in the allergic inflammatory response is releasesd by the mast cells and basophils. The aim of this study was to highlight the role of histamine in allergic immunological events, their effect on Th1 and Th2 subpopulation of lymphocytes and the production of the corresponding cytokines, as well as the role of histamine blockers in the treatment of these conditions. Histamine achieves its effect by binding to the four types of its receptors, which are widely distributed in the body. Histamine blockers block a numerous effects of histamine by binding to these receptors. As a highly selective second-generation antihistamine, cetirizine not only achieves its effects by binding to H1 receptors, but also attenuates numerous events during the inflammatory process. Knowledge of the effects -

Histamine Receptors
Tocris Scientific Review Series Tocri-lu-2945 Histamine Receptors Iwan de Esch and Rob Leurs Introduction Leiden/Amsterdam Center for Drug Research (LACDR), Division Histamine is one of the aminergic neurotransmitters and plays of Medicinal Chemistry, Faculty of Sciences, Vrije Universiteit an important role in the regulation of several (patho)physiological Amsterdam, De Boelelaan 1083, 1081 HV, Amsterdam, The processes. In the mammalian brain histamine is synthesised in Netherlands restricted populations of neurons that are located in the tuberomammillary nucleus of the posterior hypothalamus.1 Dr. Iwan de Esch is an assistant professor and Prof. Rob Leurs is These neurons project diffusely to most cerebral areas and have full professor and head of the Division of Medicinal Chemistry of been implicated in several brain functions (e.g. sleep/ the Leiden/Amsterdam Center of Drug Research (LACDR), VU wakefulness, hormonal secretion, cardiovascular control, University Amsterdam, The Netherlands. Since the seventies, thermoregulation, food intake, and memory formation).2 In histamine receptor research has been one of the traditional peripheral tissues, histamine is stored in mast cells, eosinophils, themes of the division. Molecular understanding of ligand- basophils, enterochromaffin cells and probably also in some receptor interaction is obtained by combining pharmacology specific neurons. Mast cell histamine plays an important role in (signal transduction, proliferation), molecular biology, receptor the pathogenesis of various allergic conditions. After mast cell modelling and the synthesis and identification of new ligands. degranulation, release of histamine leads to various well-known symptoms of allergic conditions in the skin and the airway system. In 1937, Bovet and Staub discovered compounds that antagonise the effect of histamine on these allergic reactions.3 Ever since, there has been intense research devoted towards finding novel ligands with (anti-) histaminergic activity. -

Download Large Text CMI (PDF)
Children's Paedamin Antihistamine Oral Liquid Decongestant and Antihistamine Children 6-12 years Consumer Medicine Information What is in this leaflet? • Itchy, watery eyes Before you give • Nasal congestion Children's Paedamin This leaflet answers some common Children's Paedamin Decongestant Decongestant and questions about Children's and Antihistamine contains Antihistamine Paedamin® Decongestant and Diphenhydramine Hydrochloride Antihistamine. and Phenylephrine Hydrochloride. When you must not give it It does not contain all the available Diphenhydramine Hydrochloride Do not use Children's Paedamin information. It does not take the belongs to a group of medicines Decongestant and Antihistamine if place of talking to your doctor or called 'antihistamines'. you/ your child have an allergy to: pharmacist. Antihistamines help reduce allergic All medicines have risks and symptoms, such as sneezing, runny • any medicine containing benefits. Your doctor or pharmacist nose or itchy, watery eyes, by Diphenhydramine has weighed the risks of you/your preventing the effects of a substance Hydrochloride or other child taking Children's Paedamin called histamine. Histamine is antihistamines Decongestant and Antihistamine produced by the body in response to • any medicine containing against the benefits they expect it foreign substances that the body is Phenylephrine Hydrochloride will have for you. allergic to. • any of the ingredients listed at If you have any concerns about Phenylephrine Hydrochloride the end of this leaflet taking this medicine, ask your belongs to a group of medicines Some of the symptoms of an doctor or pharmacist. called decongestants. allergic reaction may include: Keep this leaflet with the It works by reducing congestion in • shortness of breath medicine. -
Beta Blocker
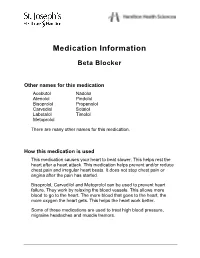
Medication Information Beta Blocker Other names for this medication Acebutol Nadolol Atenolol Pindolol Bisoprolol Propanolol Carvediol Sotalol Labetalol Timolol Metoprolol There are many other names for this medication. How this medication is used This medication causes your heart to beat slower. This helps rest the heart after a heart attack. This medication helps prevent and/or reduce chest pain and irregular heart beats. It does not stop chest pain or angina after the pain has started. Bisoprolol, Carvedilol and Metoprolol can be used to prevent heart failure. They work by relaxing the blood vessels. This allows more blood to go to the heart. The more blood that goes to the heart, the more oxygen the heart gets. This helps the heart work better. Some of these medications are used to treat high blood pressure, migraine headaches and muscle tremors. Beta Blocker How to take this medication Take this medication exactly as directed by your doctor or health care provider. It must be taken regularly, even if you feel well. Do not suddenly stop taking this medication without checking with your doctor or health care provider first. Suddenly stopping this medication can cause: • chest pain • irregular heart beats • high blood pressure. When it is time to stop taking this medication your doctor or health care provider may slowly decrease the amount. If you miss a dose of this medication, take it as soon as possible. However, if it is almost time for the next dose, skip the missed dose and go back to your regular time. Do not take 2 doses at one time. -

H1-Antihistamines for Chronic Spontaneous Urticaria: an Abridged Cochrane Systematic Review
H1-antihistamines for chronic spontaneous urticaria: An abridged Cochrane Systematic Review Sharma, Maulina , Bennett, C. , Carter, Ben and Cohen, Stuart N. Author post-print (accepted) deposited by Coventry University’s Repository Original citation & hyperlink: Sharma, Maulina , Bennett, C. , Carter, Ben and Cohen, Stuart N. (2015) H1-antihistamines for chronic spontaneous urticaria: An abridged Cochrane Systematic Review . Journal of the American Academy of Dermatology, volume 73 (4): 710-716 http://dx.doi.org/10.1016/j.jaad.2015.06.048 DOI 10.1016/j.jaad.2015.06.048 ISSN 0190-9622 ESSN 1097-6787 Publisher: Elsevier NOTICE: this is the author’s version of a work that was accepted for publication in Journal of the American Academy of Dermatology. Changes resulting from the publishing process, such as peer review, editing, corrections, structural formatting, and other quality control mechanisms may not be reflected in this document. Changes may have been made to this work since it was submitted for publication. A definitive version was subsequently published in Journal of the American Academy of Dermatology, [VOL 73, ISSUE 4, (2015)] DOI: 10.1016/j.jaad.2015.06.048 © 2015, Elsevier. Licensed under the Creative Commons Attribution-NonCommercial- NoDerivatives 4.0 International http://creativecommons.org/licenses/by-nc-nd/4.0/ Copyright © and Moral Rights are retained by the author(s) and/ or other copyright owners. A copy can be downloaded for personal non-commercial research or study, without prior permission or charge. This item cannot be reproduced or quoted extensively from without first obtaining permission in writing from the copyright holder(s). The content must not be changed in any way or sold commercially in any format or medium without the formal permission of the copyright holders. -

Wo 2010/075090 A2
(12) INTERNATIONAL APPLICATION PUBLISHED UNDER THE PATENT COOPERATION TREATY (PCT) (19) World Intellectual Property Organization International Bureau (10) International Publication Number (43) International Publication Date 1 July 2010 (01.07.2010) WO 2010/075090 A2 (51) International Patent Classification: (81) Designated States (unless otherwise indicated, for every C07D 409/14 (2006.01) A61K 31/7028 (2006.01) kind of national protection available): AE, AG, AL, AM, C07D 409/12 (2006.01) A61P 11/06 (2006.01) AO, AT, AU, AZ, BA, BB, BG, BH, BR, BW, BY, BZ, CA, CH, CL, CN, CO, CR, CU, CZ, DE, DK, DM, DO, (21) International Application Number: DZ, EC, EE, EG, ES, FI, GB, GD, GE, GH, GM, GT, PCT/US2009/068073 HN, HR, HU, ID, IL, IN, IS, JP, KE, KG, KM, KN, KP, (22) International Filing Date: KR, KZ, LA, LC, LK, LR, LS, LT, LU, LY, MA, MD, 15 December 2009 (15.12.2009) ME, MG, MK, MN, MW, MX, MY, MZ, NA, NG, NI, NO, NZ, OM, PE, PG, PH, PL, PT, RO, RS, RU, SC, SD, (25) Filing Language: English SE, SG, SK, SL, SM, ST, SV, SY, TJ, TM, TN, TR, TT, (26) Publication Language: English TZ, UA, UG, US, UZ, VC, VN, ZA, ZM, ZW. (30) Priority Data: (84) Designated States (unless otherwise indicated, for every 61/122,478 15 December 2008 (15.12.2008) US kind of regional protection available): ARIPO (BW, GH, GM, KE, LS, MW, MZ, NA, SD, SL, SZ, TZ, UG, ZM, (71) Applicant (for all designated States except US): AUS- ZW), Eurasian (AM, AZ, BY, KG, KZ, MD, RU, TJ, PEX PHARMACEUTICALS, INC.