Histamine and Antihistamines Sites of Action Conditions Which Cause Release Aron H
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

MASCC/ESMO ANTIEMETIC GUIDELINE 2016 with Updates in 2019
1 ANTIEMETIC GUIDELINES: MASCC/ESMO MASCC/ESMO ANTIEMETIC GUIDELINE 2016 With Updates in 2019 Organizing and Overall Meeting Chairs: Matti Aapro, MD Richard J. Gralla, MD Jørn Herrstedt, MD, DMSci Alex Molassiotis, RN, PhD Fausto Roila, MD © Multinational Association of Supportive Care in CancerTM All rights reserved worldwide. 2 ANTIEMETIC GUIDELINES: MASCC/ESMO These slides are provided to all by the Multinational Association of Supportive Care in Cancer and can be used freely, provided no changes are made and the MASCC and ESMO logos, as well as date of the information are retained. For questions please contact: Matti Aapro at [email protected] Chair, MASCC Antiemetic Study Group or Alex Molassiotis at [email protected] Past Chair, MASCC Antiemetic Study Group 3 ANTIEMETIC GUIDELINES: MASCC/ESMO Consensus A few comments on this guideline set: • This set of guideline slides represents the latest edition of the guideline process. • This set of slides has been endorsed by the MASCC Antiemetic Guideline Committee and ESMO Guideline Committee. • The guidelines are based on the votes of the panel at the Copenhagen Consensus Conference on Antiemetic Therapy, June 2015. • Latest version: March 2016, with updates in 2019. 4 ANTIEMETIC GUIDELINES: MASCC/ESMO Changes: The Steering Committee has clarified some points: 2016: • A footnote clarified that aprepitant 165 mg is approved by regulatory authorities in some parts of the world ( although no randomised clinical trial has investigated this dose ). Thus use of aprepitant 80 mg in the delayed phase is only for those cases where aprepitant 125 mg is used on day 1. • A probable modification in pediatric guidelines based on the recent Cochrane meta-analysis is indicated. -

Pharmacology
Pharmacology New for 2020-2021 Competitor orientation deleted from ILC. Event Summary Pharmacology provides HOSA members with the opportunity to gain knowledge and skills regarding the area of healthcare concerned with uses, effects, and modes of actions of drugs. This competitive event consists of a written test with a tie-breaker essay question. This event aims to inspire members to learn about how drugs work in the body, proper administration, and adaptations for different patients and conditions. Dress Code Competitors must be in official HOSA uniform or proper business attire. Bonus points will be awarded for proper dress. General Rules 1. Competitors in this event must be active members of HOSA-Future Health Professionals, in good standing. 2. Secondary and Postsecondary/Collegiate divisions are eligible to compete in this event. 3. Competitors must be familiar with and adhere to the “General Rules and Regulations of the HOSA Competitive Events Program (GRR)." 4. All competitors shall report to the site of the event at the time designated for each round of competition. At ILC, competitor’s photo ID must be presented prior to ALL competition rounds. Official References • Fulcher, Soto and Fulcher. Pharmacology: Principles and Applications. Elsevier, Latest edition. • Ford, Susan and Sally Roach. Roach’s Introductory Clinical Pharmacology. Wolters Kluwer, Latest edition. Written Test 5. Test Instructions: The written test will consist of 100 multiple choice items in a maximum of 90 minutes. 6. Time Remaining Announcements: There will be a verbal announcement when there are 60 minutes, 30 minutes, 15 minutes, 5 minutes, and 1 minute remaining to complete the test. -

Guidelines for the Forensic Analysis of Drugs Facilitating Sexual Assault and Other Criminal Acts
Vienna International Centre, PO Box 500, 1400 Vienna, Austria Tel.: (+43-1) 26060-0, Fax: (+43-1) 26060-5866, www.unodc.org Guidelines for the Forensic analysis of drugs facilitating sexual assault and other criminal acts United Nations publication Printed in Austria ST/NAR/45 *1186331*V.11-86331—December 2011 —300 Photo credits: UNODC Photo Library, iStock.com/Abel Mitja Varela Laboratory and Scientific Section UNITED NATIONS OFFICE ON DRUGS AND CRIME Vienna Guidelines for the forensic analysis of drugs facilitating sexual assault and other criminal acts UNITED NATIONS New York, 2011 ST/NAR/45 © United Nations, December 2011. All rights reserved. The designations employed and the presentation of material in this publication do not imply the expression of any opinion whatsoever on the part of the Secretariat of the United Nations concerning the legal status of any country, territory, city or area, or of its authorities, or concerning the delimitation of its frontiers or boundaries. This publication has not been formally edited. Publishing production: English, Publishing and Library Section, United Nations Office at Vienna. List of abbreviations . v Acknowledgements .......................................... vii 1. Introduction............................................. 1 1.1. Background ........................................ 1 1.2. Purpose and scope of the manual ...................... 2 2. Investigative and analytical challenges ....................... 5 3 Evidence collection ...................................... 9 3.1. Evidence collection kits .............................. 9 3.2. Sample transfer and storage........................... 10 3.3. Biological samples and sampling ...................... 11 3.4. Other samples ...................................... 12 4. Analytical considerations .................................. 13 4.1. Substances encountered in DFSA and other DFC cases .... 13 4.2. Procedures and analytical strategy...................... 14 4.3. Analytical methodology .............................. 15 4.4. -

Clinical Practice Guideline for Emergency Department Ketamine Dissociative Sedation: 2011 Update
PAIN MANAGEMENT/CONCEPTS Clinical Practice Guideline for Emergency Department Ketamine Dissociative Sedation: 2011 Update Steven M. Green, MD, Mark G. Roback, MD, Robert M. Kennedy, MD, Baruch Krauss, MD, EdM From the Department of Emergency Medicine, Loma Linda University Medical Center and Children’s Hospital, Loma Linda, CA (Green); the Department of Pediatrics, University of Minnesota, Minneapolis, MN (Roback); the Division of Emergency Medicine, St. Louis Children’s Hospital, Washington University, St. Louis, MO (Kennedy); and the Division of Emergency Medicine, Children’s Hospital Boston and Department of Pediatrics, Harvard Medical School, Boston, MA (Krauss). We update an evidence-based clinical practice guideline for the administration of the dissociative agent ketamine for emergency department procedural sedation and analgesia. Substantial new research warrants revision of the widely disseminated 2004 guideline, particularly with respect to contraindications, age recommendations, potential neurotoxicity, and the role of coadministered anticholinergics and benzodiazepines. We critically discuss indications, contraindications, personnel requirements, monitoring, dosing, coadministered medications, recovery issues, and future research questions for ketamine dissociative sedation. [Ann Emerg Med. 2011;xx:xxx.] 0196-0644/$-see front matter Copyright © 2011 by the American College of Emergency Physicians. doi:10.1016/j.annemergmed.2010.11.030 INTRODUCTION thalamocortical and limbic systems, effectively dissociating the The dissociative -

Cysteinyl Leukotriene Receptor 1/2 Antagonists Nonselectively Modulate Organic Anion Transport by Multidrug Resistance Proteins (MRP1-4) S
Supplemental material to this article can be found at: http://dmd.aspetjournals.org/content/suppl/2016/04/11/dmd.116.069468.DC1 1521-009X/44/6/857–866$25.00 http://dx.doi.org/10.1124/dmd.116.069468 DRUG METABOLISM AND DISPOSITION Drug Metab Dispos 44:857–866, June 2016 Copyright ª 2016 by The American Society for Pharmacology and Experimental Therapeutics Cysteinyl Leukotriene Receptor 1/2 Antagonists Nonselectively Modulate Organic Anion Transport by Multidrug Resistance Proteins (MRP1-4) s Mark A. Csandl, Gwenaëlle Conseil, and Susan P. C. Cole Departments of Biomedical and Molecular Sciences (M.A.C., S.P.C.C.), and Pathology and Molecular Medicine (G.C., S.P.C.C.), Division of Cancer Biology and Genetics, Queen’s University Cancer Research Institute, Kingston, ON, Canada Received January 13, 2016; accepted April 7, 2016 ABSTRACT Active efflux of both drugs and organic anion metabolites is class of antagonists showed any MRP selectivity. For E217bG Downloaded from mediated by the multidrug resistance proteins (MRPs). MRP1 uptake, LTM IC50s ranged from 1.2 to 26.9 mMandweremost (ABCC1), MRP2 (ABCC2), MRP3 (ABCC3), and MRP4 (ABCC4) have comparable for MRP1 and MRP4. The LTM rank order inhibitory partially overlapping substrate specificities and all transport 17b- potencies for E217bGversusLTC4 uptake by MRP1, and E217bG estradiol 17-(b-D-glucuronide) (E217bG). The cysteinyl leukotriene versus PGE2 uptake by MRP4, were also similar. Three of four receptor 1 (CysLT1R) antagonist MK-571 inhibits all four MRP CysLT1R-selective LTMs also stimulated MRP2 (but not MRP3) homologs, but little is known about the modulatory effects of newer transport and thus exerted a concentration-dependent biphasic leukotriene modifiers (LTMs). -

Clinical Pharmacology 1: Phase 1 Studies and Early Drug Development
Clinical Pharmacology 1: Phase 1 Studies and Early Drug Development Gerlie Gieser, Ph.D. Office of Clinical Pharmacology, Div. IV Objectives • Outline the Phase 1 studies conducted to characterize the Clinical Pharmacology of a drug; describe important design elements of and the information gained from these studies. • List the Clinical Pharmacology characteristics of an Ideal Drug • Describe how the Clinical Pharmacology information from Phase 1 can help design Phase 2/3 trials • Discuss the timing of Clinical Pharmacology studies during drug development, and provide examples of how the information generated could impact the overall clinical development plan and product labeling. Phase 1 of Drug Development CLINICAL DEVELOPMENT RESEARCH PRE POST AND CLINICAL APPROVAL 1 DISCOVERY DEVELOPMENT 2 3 PHASE e e e s s s a a a h h h P P P Clinical Pharmacology Studies Initial IND (first in human) NDA/BLA SUBMISSION Phase 1 – studies designed mainly to investigate the safety/tolerability (if possible, identify MTD), pharmacokinetics and pharmacodynamics of an investigational drug in humans Clinical Pharmacology • Study of the Pharmacokinetics (PK) and Pharmacodynamics (PD) of the drug in humans – PK: what the body does to the drug (Absorption, Distribution, Metabolism, Excretion) – PD: what the drug does to the body • PK and PD profiles of the drug are influenced by physicochemical properties of the drug, product/formulation, administration route, patient’s intrinsic and extrinsic factors (e.g., organ dysfunction, diseases, concomitant medications, -

I. Antihistamines Seunghoon Han* Department of Clinical Pharmacology and Therapeutics, Seoul St
2014;22(1):13-18 TCP Translational and Clinical Pharmacology http://dx.doi.org/10.12793/tcp.2014.22.1.13 Clinical Pharmacology Review for Primary Health Care Providers: I. Antihistamines Seunghoon Han* Department of Clinical Pharmacology and Therapeutics, Seoul St. Mary’s Hospital, The Catholic University of Korea, Seoul 137-701, Korea *Correspondence: S. Han; Tel: +82-2-2258-7326, Fax: +82-2-2258-7876, E-mail: [email protected] Received 31 May 2014 Primary health care providers play a critical role in maintaining public health, and the appropri- Accepted 31 May 2014 ate use of pharmaceutical products is one of the major parts of their practice. This series of articles, pISSN: 2289-0882 entitled ‘Clinical Pharmacology Review for Primary Health Care Providers,’ is intended to help pri- mary health care providers select more appropriate prescriptions for frequently used drugs based on up-to-date information. We expect that this effort will contribute to improvements in public health and diminish unnecessary drug use. Introduction tion on the H1 receptor.[8] THERAPEU Antihistamines include some of the most frequently prescribed drugs in the primary health care environment for the symp- Generations and Classes tomatic relief of allergic diseases, the common cold, urticaria, Many primary health care providers are well-informed about T and insomnia.[1-5] The importance of antihistamines has been the different ‘generations’ of antihistamines but not about the ICS TU emphasized as the prevalence of target diseases increases.[6,7] different ‘classes’ characterized according to chemical structure. However, the appropriate use, clinical effectiveness, and target [1] This discrepancy seems reasonable because ‘inter-generation’ T populations for prescription of antihistamines are still a matter differences are more prominent than ‘inter-class’ differences. -
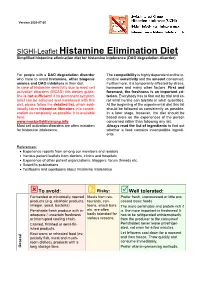
SIGHI-Leaflet Histamine Elimination Diet Simplified Histamine Elimination Diet for Histamine Intolerance (DAO Degradation Disorder)
Version 2020-07-20 SIGHI-Leaflet Histamine Elimination Diet Simplified histamine elimination diet for histamine intolerance (DAO degradation disorder) For people with a DAO degradation disorder The compatibility is highly dependent on the in- who have to avoid histamine, other biogenic dividual sensitivity and the amount consumed. amines and DAO inhibitors in their diet. Furthermore, it is temporarily affected by stress, In case of histamine sensitivity due to mast cell hormones and many other factors. First and activation disorders (MCAD) this dietary guide- foremost, the freshness is an important cri- line is not sufficient! If no permanent symptom terion. Everybody has to find out by trial and er- relief can be achieved and maintained with this ror what he/she can tolerate in what quantities. diet, please follow the detailed list, which addi- At the beginning of the experimental diet this list tionally takes histamine liberators into consid- should be followed as consistently as possible. eration as completely as possible. It is available In a later stage, however, the diet should be here: based more on the experiences of the person www.mastzellaktivierung.info concerned rather than following any list. Mast cell activation disorders are often mistaken Always read the list of ingredients to find out for histamine intolerance. whether a food contains incompatible ingredi- ents. References: • Experience reports from among our members and readers • Various patient leaflets from doctors, clinics and hospitals • Experience of other patient organizations, bloggers, forum threads etc. • Scientific publications • Textbooks and cookbooks about histamine intolerance To avoid: ? Risky: Well tolerated: Fermented or microbially ripened Meals from res- Prefer fresh, unprocessed or little pro- products (e.g. -

The In¯Uence of Medication on Erectile Function
International Journal of Impotence Research (1997) 9, 17±26 ß 1997 Stockton Press All rights reserved 0955-9930/97 $12.00 The in¯uence of medication on erectile function W Meinhardt1, RF Kropman2, P Vermeij3, AAB Lycklama aÁ Nijeholt4 and J Zwartendijk4 1Department of Urology, Netherlands Cancer Institute/Antoni van Leeuwenhoek Hospital, Plesmanlaan 121, 1066 CX Amsterdam, The Netherlands; 2Department of Urology, Leyenburg Hospital, Leyweg 275, 2545 CH The Hague, The Netherlands; 3Pharmacy; and 4Department of Urology, Leiden University Hospital, P.O. Box 9600, 2300 RC Leiden, The Netherlands Keywords: impotence; side-effect; antipsychotic; antihypertensive; physiology; erectile function Introduction stopped their antihypertensive treatment over a ®ve year period, because of side-effects on sexual function.5 In the drug registration procedures sexual Several physiological mechanisms are involved in function is not a major issue. This means that erectile function. A negative in¯uence of prescrip- knowledge of the problem is mainly dependent on tion-drugs on these mechanisms will not always case reports and the lists from side effect registries.6±8 come to the attention of the clinician, whereas a Another way of looking at the problem is drug causing priapism will rarely escape the atten- combining available data on mechanisms of action tion. of drugs with the knowledge of the physiological When erectile function is in¯uenced in a negative mechanisms involved in erectile function. The way compensation may occur. For example, age- advantage of this approach is that remedies may related penile sensory disorders may be compen- evolve from it. sated for by extra stimulation.1 Diminished in¯ux of In this paper we will discuss the subject in the blood will lead to a slower onset of the erection, but following order: may be accepted. -

The 5-HT6 Receptor Antagonist SB-271046 Selectively Enhances Excitatory Neurotransmission in the Rat Frontal Cortex and Hippocampus Lee A
The 5-HT6 Receptor Antagonist SB-271046 Selectively Enhances Excitatory Neurotransmission in the Rat Frontal Cortex and Hippocampus Lee A. Dawson, Ph.D., Huy Q. Nguyen, B.S., and Ping Li, B.S. Preclinical evidence has suggested a possible role for the 5-HT6 increases in extracellular glutamate levels in both frontal receptor in the treatment of cognitive dysfunction. However, cortex and dorsal hippocampus, respectively. These effects were currently there is little neurochemical evidence suggesting the completely attenuated by infusion of tetrodotoxin but mechanism(s) which may be involved. Using the selective unaffected by the muscarinic antagonist, atropine. Here we 5-HT6 antagonist SB-271046 and in vivo microdialysis, we demonstrate for the first time the selective enhancement of have evaluated the effects of this compound on the modulation excitatory neurotransmission by SB-271046 in those brain of basal neurotransmitter release within multiple brain regions regions implicated in cognitive and memory function, and of the freely moving rat. SB-271046 produced no change in provide mechanistic evidence in support of a possible basal levels of dopamine (DA), norepinephrine (NE) or 5-HT therapeutic role for 5-HT6 receptor antagonists in the in the striatum, frontal cortex, dorsal hippocampus or nucleus treatment of cognitive and memory dysfunction. accumbens. Similarly, this compound had no effect on [Neuropsychopharmacology 25:662–668, 2001] excitatory neurotransmission in the striatum or nucleus © 2001 American College of Neuropsychopharmacology. accumbens. Conversely, SB-271046 produced 3- and 2-fold Published by Elsevier Science Inc. KEY WORDS: 5-HT6 receptor; SB-271046; Microdialysis; sma et al. 1993; Ruat et al. -

THE USE of MIRTAZAPINE AS a HYPNOTIC O Uso Da Mirtazapina Como Hipnótico Francisca Magalhães Scoralicka, Einstein Francisco Camargosa, Otávio Toledo Nóbregaa
ARTIGO ESPECIAL THE USE OF MIRTAZAPINE AS A HYPNOTIC O uso da mirtazapina como hipnótico Francisca Magalhães Scoralicka, Einstein Francisco Camargosa, Otávio Toledo Nóbregaa Prescription of approved hypnotics for insomnia decreased by more than 50%, whereas of antidepressive agents outstripped that of hypnotics. However, there is little data on their efficacy to treat insomnia, and many of these medications may be associated with known side effects. Antidepressants are associated with various effects on sleep patterns, depending on the intrinsic pharmacological properties of the active agent, such as degree of inhibition of serotonin or noradrenaline reuptake, effects on 5-HT1A and 5-HT2 receptors, action(s) at alpha-adrenoceptors, and/or histamine H1 sites. Mirtazapine is a noradrenergic and specific serotonergic antidepressive agent that acts by antagonizing alpha-2 adrenergic receptors and blocking 5-HT2 and 5-HT3 receptors. It has high affinity for histamine H1 receptors, low affinity for dopaminergic receptors, and lacks anticholinergic activity. In spite of these potential beneficial effects of mirtazapine on sleep, no placebo-controlled randomized clinical trials of ABSTRACT mirtazapine in primary insomniacs have been conducted. Mirtazapine was associated with improvements in sleep on normal sleepers and depressed patients. The most common side effects of mirtazapine, i.e. dry mouth, drowsiness, increased appetite and increased body weight, were mostly mild and transient. Considering its use in elderly people, this paper provides a revision about studies regarding mirtazapine for sleep disorders. KEYWORDS: sleep; antidepressive agents; sleep disorders; treatment� A prescrição de hipnóticos aprovados para insônia diminuiu em mais de 50%, enquanto de antidepressivos ultrapassou a dos primeiros. -

Tachykinins in the Gut. Part II. Roles in Neural Excitation, Secretion and Inflammation
Pfxnma~ol.Ther. Vol. 73, No. 3, pp. 219-263, 1997 ISSN 0163-7258197$32.00 CopyrIght0 1997 ElsevierScience Inc. PI1 SO163-7258(96)00196-9 ELSEVIER A.wciate Editor: 1. We&r Tachykinins in the Gut. Part II. Roles in Neural Excitation, Secretion and Inflammation Peter Holzer” and Ulrike Holw-er-Pets&e DEPARTMENT0FEXPERIMENTALANDCLINlCALPHARMACOLOGY,UNIVERSlTYOFGRAZ,UNlVERSITiiTSPLATZ4,A-8010GRAZ,AUSTRIA ABSTRACT. The preprotachykinin-A gene-derived peptides substance (substance P; SP) and neurokinin (NK) A are expressed in intrinsic enteric neurons, which supply all layers of the gut, and extrinsic primary afferent nerve fibers, which innervate primarily the arterial vascular system. The actions of tachykinins on the digestive effector systems are mediated by three different types of tachykinin receptor, termed NK,, NKr and NK, receptors. Within the enteric nervous system, SP and NKA are likely to mediate, or comediate, slow synaptic transmission and to modulate neuronal excitability via stimulation of NK, and NK, receptors. In the intestinal mucosa, tachykinins cause net secretion of fluid and electrolytes, and it appears as if SP and NKA play a messenger role in intramural secretory reflex pathways. Secretory processes in the salivary glands and pancreas are likewise influenced by tachykinins. The gastrointestinal arterial system may be dilated or constricted by tachykinins, whereas constriction and an increase in the vascular permeability are the only effects seen in the venous system. Various gastrointestinal disorders are associated with distinct changes in the tachykinin system, and there is increasing evidence that tachykinins participate in the hypersecretory, vascular and immunological disturbances associated with infection and inflammatory bowel disease. In a therapeutic perspective, it would seem conceivable that tachykinin antagonists could be exploited as antidiarrheal, anti- inflammatory and antinociceptive drugs.