DOXYLAMINE SUCCINATE 1. Exposure Data
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Guidelines for the Forensic Analysis of Drugs Facilitating Sexual Assault and Other Criminal Acts
Vienna International Centre, PO Box 500, 1400 Vienna, Austria Tel.: (+43-1) 26060-0, Fax: (+43-1) 26060-5866, www.unodc.org Guidelines for the Forensic analysis of drugs facilitating sexual assault and other criminal acts United Nations publication Printed in Austria ST/NAR/45 *1186331*V.11-86331—December 2011 —300 Photo credits: UNODC Photo Library, iStock.com/Abel Mitja Varela Laboratory and Scientific Section UNITED NATIONS OFFICE ON DRUGS AND CRIME Vienna Guidelines for the forensic analysis of drugs facilitating sexual assault and other criminal acts UNITED NATIONS New York, 2011 ST/NAR/45 © United Nations, December 2011. All rights reserved. The designations employed and the presentation of material in this publication do not imply the expression of any opinion whatsoever on the part of the Secretariat of the United Nations concerning the legal status of any country, territory, city or area, or of its authorities, or concerning the delimitation of its frontiers or boundaries. This publication has not been formally edited. Publishing production: English, Publishing and Library Section, United Nations Office at Vienna. List of abbreviations . v Acknowledgements .......................................... vii 1. Introduction............................................. 1 1.1. Background ........................................ 1 1.2. Purpose and scope of the manual ...................... 2 2. Investigative and analytical challenges ....................... 5 3 Evidence collection ...................................... 9 3.1. Evidence collection kits .............................. 9 3.2. Sample transfer and storage........................... 10 3.3. Biological samples and sampling ...................... 11 3.4. Other samples ...................................... 12 4. Analytical considerations .................................. 13 4.1. Substances encountered in DFSA and other DFC cases .... 13 4.2. Procedures and analytical strategy...................... 14 4.3. Analytical methodology .............................. 15 4.4. -

Diphenhydramine Hydrochloride (CASRN 147-24-0) in F344/N Rats
NATIONAL TOXICOLOGY PROGRAM Technical Report Series No. 355 TOXICOLOGY AND CARCINOGENESIS STUDIES OF DIPHENHYDRAMINE HYDROCHLORIDE (CAS NO. 147-24-0) IN F344/N RATS AND B6C3F1 MICE (FEED STUDIES) LJ.S. DEPARTMENT OF HEALTH AND HUMAN SERVICES Public Health Service National Institutes of Health NTP ‘TECHNICAL REPORT ON THE TOXICOLOGY AND CARCINOGENESIS STUDIES OF DIPHENHYDRAMINE HYDROCHLORIDE (CAS NO. 147-24-0) IN F344/N RATS AND B6C3F1 MICE (FEED STUDIES) R. Melnick, Ph.D., Study Scientist NATIONAL TOXICOLOGY PROGRAM P.O. Box 12233 Research Triangle Park, NC 27709 September 1989 NTP TR 355 NIH Publication No. 89-2810 U.S. DEPARTMENT OF HEALTH AND HUMAN SERVICES Public Health Service National Institutes of Health CONTENTS PAGE ABSTRACT ................................................................ 3 EXPLANATION OF LEVELS OF EVIDENCE OF CARCINOGENIC ACTIVITY .................. 6 CONTRIBUTORS ............................................................ 7 PEERREVIEWPANEL ........................................................ 8 SUMMARY OF PEER REVIEW COMMENTS ......................................... 9 I. INTRODUCTION ........................................................ 11 I1. MATERIALS AND METHODS .............................................. 21 III. RESULTS ............................................................. 35 RATS ............................................................. 36 MICE ............................................................. 45 GENETIC TOXICOLOGY ............................................... 53 IV. -

The In¯Uence of Medication on Erectile Function
International Journal of Impotence Research (1997) 9, 17±26 ß 1997 Stockton Press All rights reserved 0955-9930/97 $12.00 The in¯uence of medication on erectile function W Meinhardt1, RF Kropman2, P Vermeij3, AAB Lycklama aÁ Nijeholt4 and J Zwartendijk4 1Department of Urology, Netherlands Cancer Institute/Antoni van Leeuwenhoek Hospital, Plesmanlaan 121, 1066 CX Amsterdam, The Netherlands; 2Department of Urology, Leyenburg Hospital, Leyweg 275, 2545 CH The Hague, The Netherlands; 3Pharmacy; and 4Department of Urology, Leiden University Hospital, P.O. Box 9600, 2300 RC Leiden, The Netherlands Keywords: impotence; side-effect; antipsychotic; antihypertensive; physiology; erectile function Introduction stopped their antihypertensive treatment over a ®ve year period, because of side-effects on sexual function.5 In the drug registration procedures sexual Several physiological mechanisms are involved in function is not a major issue. This means that erectile function. A negative in¯uence of prescrip- knowledge of the problem is mainly dependent on tion-drugs on these mechanisms will not always case reports and the lists from side effect registries.6±8 come to the attention of the clinician, whereas a Another way of looking at the problem is drug causing priapism will rarely escape the atten- combining available data on mechanisms of action tion. of drugs with the knowledge of the physiological When erectile function is in¯uenced in a negative mechanisms involved in erectile function. The way compensation may occur. For example, age- advantage of this approach is that remedies may related penile sensory disorders may be compen- evolve from it. sated for by extra stimulation.1 Diminished in¯ux of In this paper we will discuss the subject in the blood will lead to a slower onset of the erection, but following order: may be accepted. -

Pregnancy-Safe-Medications
PEACHTREE WOMEN’S SPECIALISTS, P.C. Obstetrics and Gynecology Melissa Counihan, M.D Bonita Dozier, M.D. James P. Ingvoldstad, MD James Knoer, M.D. Helen McSwain, M.D. Archie Roberts, M.D. Lillian Schapiro, MD PREGNANCY SAFE MEDICATIONS Antihistamines o Actifed o Benadryl o Claritin o Claritin-D o Chlor-Trimeton-D o Chlor-Trimeton-DM o Sudafed* o Zyrtec and Zyrtec-D * Georgia law now requires that Sudafed be requested from the pharmacist, even though it is not a prescription medication. Cough o Robitussin o Robitussin DM o Robitussin PE* o You may take any cough drop *DO NOT use if taking Sudafed or Brethine/Terbutaline. Calcium Supplement o Tums EX- two tablets twice daily o Viactiv Constipation o Colace o Fibercon o Konsyl o Metamucil o Milk of Magnesia o Perdiem Increase dietary roughage, bran, dark green leafy vegetables and fruits. Drink eight to ten glasses of water daily. Decongestants* o Sudafed o Sudafed Sinus o Sudafed Non-drying o Actifed o Tylenol Sinus o Benadryl o Doxylamine Succinate *After the first trimester PREGNANCY SAFE MEDICATIONS (Continued) Dry Skin o Cocoa Butter o Eucerin Lotion o Vitamin E Lotion Fever o Tylenol* o Tylenol Extra Strength* *DO NOT take more than 12 tablets of Regular Strength Tylenol in 24 hours and no more than 6 tablets of Extra Strength Tylenol in 24 hours. Gas o Mylicon o Mylanta GAS o Phazyme o Mylanta Antacid/Anti-gas Hemorrhoids o Preparation H o Colace o Annusol Suppository/Ointment (With or without Cortisone) Increase dietary roughage, bran, dark green leafy vegetables and fruits. -

Histamine and Antihistamines
ACTA FACULTATIS MEDICAE NAISSENSIS UDC: 615.218 DOI: 10.1515/afmnai-2015-0001 Review article Histamine and Antihistamines Nikola Stojković1, Snežana Cekić2, Milica Ristov3, Marko Ristić1, Davor Đukić1, Maša Binić1, Dragan Virijević1 1University of Niš, Faculty of Medicine, PhD student, Serbia 2Institute of Physiology, University of Niš, Faculty of Medicine , Serbia 3Doctor of Medicine SUMMARY In recent years, there has been a steady increase in the prevalence of allergic diseases. Allergic immune response represents a complex network of cellular events involving numerous immune cells and mediators. It represents the interaction of innate and acquired immune response. The key role in the immune cascade is taken by histamine, a natural component of the body, which in the allergic inflammatory response is releasesd by the mast cells and basophils. The aim of this study was to highlight the role of histamine in allergic immunological events, their effect on Th1 and Th2 subpopulation of lymphocytes and the production of the corresponding cytokines, as well as the role of histamine blockers in the treatment of these conditions. Histamine achieves its effect by binding to the four types of its receptors, which are widely distributed in the body. Histamine blockers block a numerous effects of histamine by binding to these receptors. As a highly selective second-generation antihistamine, cetirizine not only achieves its effects by binding to H1 receptors, but also attenuates numerous events during the inflammatory process. Knowledge of the effects -

Download Large Text CMI (PDF)
Children's Paedamin Antihistamine Oral Liquid Decongestant and Antihistamine Children 6-12 years Consumer Medicine Information What is in this leaflet? • Itchy, watery eyes Before you give • Nasal congestion Children's Paedamin This leaflet answers some common Children's Paedamin Decongestant Decongestant and questions about Children's and Antihistamine contains Antihistamine Paedamin® Decongestant and Diphenhydramine Hydrochloride Antihistamine. and Phenylephrine Hydrochloride. When you must not give it It does not contain all the available Diphenhydramine Hydrochloride Do not use Children's Paedamin information. It does not take the belongs to a group of medicines Decongestant and Antihistamine if place of talking to your doctor or called 'antihistamines'. you/ your child have an allergy to: pharmacist. Antihistamines help reduce allergic All medicines have risks and symptoms, such as sneezing, runny • any medicine containing benefits. Your doctor or pharmacist nose or itchy, watery eyes, by Diphenhydramine has weighed the risks of you/your preventing the effects of a substance Hydrochloride or other child taking Children's Paedamin called histamine. Histamine is antihistamines Decongestant and Antihistamine produced by the body in response to • any medicine containing against the benefits they expect it foreign substances that the body is Phenylephrine Hydrochloride will have for you. allergic to. • any of the ingredients listed at If you have any concerns about Phenylephrine Hydrochloride the end of this leaflet taking this medicine, ask your belongs to a group of medicines Some of the symptoms of an doctor or pharmacist. called decongestants. allergic reaction may include: Keep this leaflet with the It works by reducing congestion in • shortness of breath medicine. -

(12) United States Patent (10) Patent No.: US 7,863,296 B2 Weiner Et Al
USOO7863296B2 (12) United States Patent (10) Patent No.: US 7,863,296 B2 Weiner et al. (45) Date of Patent: *Jan. 4, 2011 (54) SELECTIVE SEROTONIN RECEPTOR 5,795,894. A 8, 1998 Shue et al. NVERSEAGONSTS AS THERAPEUTICS 5,869,488 A 2f1999 Shue et al. FOR DISEASE 5,874.445 A * 2/1999 Carr et al. ................... 514,317 5,877,173 A 3/1999 Olney et al. 5,912,132 A 6/1999 Brann (75) Inventors: David M. Weiner, San Diego, CA (US); 5,952.324 A 9/1999 Barbachyn et al. Robert E. Davis, San Diego, CA (US); 5,955,281 A 9, 1999 Brann Mark R. Brann, Del Mar, CA (US); 6,107,324 A 8, 2000 Behan et al. Anna-Maria Frost-Jensen, legal 6,140,509 A 10/2000 Behan et al. representative, Rye, NH (US); Norman 6,150,393 A 11/2000 Behan et al. Nash, Carlsbad, CA (US) 6,358,698 B1 3/2002 Weiner et al. 6.479,480 B1 1 1/2002 Moyes et al. (73) Assignee: ACADIA Pharmaceuticals, Inc., San 6,486,153 B1 1 1/2002 Castro Pineiro et al. Diego, CA (US) 6,617.339 B1 9, 2003 Gravestock 6,756,393 B2 6/2004 Andersson et al. (*) Notice: Subject to any disclaimer, the term of this 6,815,458 B2 11/2004 Andersson et al. 6,911,452 B2 6/2005 Schlienger patent is extended or adjusted under 35 7,022,698 B2 4/2006 Hamied et al. U.S.C. 154(b) by 1393 days. -

Doxylamine Succinate and Pyridoxine Hydrochloride (Diclegis®, Bonjesta®) Duration Limit
Cigna National Formulary Coverage Policy Drug Quantity Management – Per Days Doxylamine succinate and pyridoxine hydrochloride (Diclegis®, Bonjesta®) Duration Limit Table of Contents Product Identifer(s) National Formulary Medical Necessity ................ 1 60889 Conditions Not Covered....................................... 2 Background .......................................................... 2 References .......................................................... 2 Revision History ................................................... 2 INSTRUCTIONS FOR USE The following Coverage Policy applies to health benefit plans administered by Cigna Companies. Certain Cigna Companies and/or lines of business only provide utilization review services to clients and do not make coverage determinations. References to standard benefit plan language and coverage determinations do not apply to those clients. Coverage Policies are intended to provide guidance in interpreting certain standard benefit plans administered by Cigna Companies. Please note, the terms of a customer’s particular benefit plan document [Group Service Agreement, Evidence of Coverage, Certificate of Coverage, Summary Plan Description (SPD) or similar plan document] may differ significantly from the standard benefit plans upon which these Coverage Policies are based. For example, a customer’s benefit plan document may contain a specific exclusion related to a topic addressed in a Coverage Policy. In the event of a conflict, a customer’s benefit plan document always supersedes the information in the Coverage Policies. In the absence of a controlling federal or state coverage mandate, benefits are ultimately determined by the terms of the applicable benefit plan document. Coverage determinations in each specific instance require consideration of 1) the terms of the applicable benefit plan document in effect on the date of service; 2) any applicable laws/regulations; 3) any relevant collateral source materials including Coverage Policies and; 4) the specific facts of the particular situation. -

Methapyrilene Hydrochloride (CAS No
National Toxicology Program Toxicity Report Series Number 46 NTP Technical Report on the Hepatotoxicity Studies of the Liver Carcinogen Methapyrilene Hydrochloride (CAS No. 135-23-9) Administered in Feed to Male F344/N Rats July 2000 U.S. Department of Health and Human Services Public Health Service National Institutes of Health FOREWORD The National Toxicology Program (NTP) is made up of four charter agencies of the U.S. Department of Health and Human Services (DHHS): the National Cancer Institute (NCI), National Institutes of Health; the National Institute of Environmental Health Sciences (NIEHS), National Institutes of Health; the National Center for Toxicological Research (NCTR), Food and Drug Administration; and the National Institute for Occupational Safety and Health (NIOSH), Centers for Disease Control and Prevention. In July 1981, the Carcinogenesis Bioassay Testing Program, NCI, was transferred to the NIEHS. The NTP coordinates the relevant programs, staff, and resources from these Public Health Service agencies relating to basic and applied research and to biological assay development and validation. The NTP develops, evaluates, and disseminates scientific information about potentially toxic and hazardous chemicals. This knowledge is used for protecting the health of the American people and for the primary prevention of disease. The studies described in this Toxicity Study Report were performed under the direction of the NIEHS and were conducted in compliance with NTP laboratory health and safety requirements and must meet or exceed all applicable federal, state, and local health and safety regulations. Animal care and use were in accordance with the Public Health Service Policy on Humane Care and Use of Animals. -
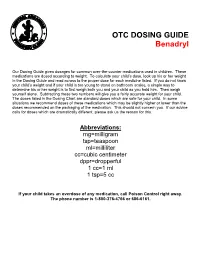
OTC DOSING GUIDE Benadryl
OTC DOSING GUIDE Benadryl Our Dosing Guide gives dosages for common over-the-counter medications used in children. These medications are dosed according to weight. To calculate your child’s dose, look up his or her weight in the Dosing Guide and read across to the proper dose for each medicine listed. If you do not know your child’s weight and if your child is too young to stand on bathroom scales, a simple way to determine his or her weight is to first weigh both you and your child as you hold him. Then weigh yourself alone. Subtracting these two numbers will give you a fairly accurate weight for your child. The doses listed in the Dosing Chart are standard doses which are safe for your child. In some situations we recommend doses of these medications which may be slightly higher or lower than the doses recommended on the packaging of the medication. This should not concern you. If our advice calls for doses which are dramatically different, please ask us the reason for this. Abbreviations: mg=milligram tsp=teaspoon ml=milliliter cc=cubic centimeter dppr=dropperful 1 cc=1 ml 1 tsp=5 cc If your child takes an overdose of any medication, call Poison Control right away. The phone number is 1-800-376-4766 or 686-6161. CHILDREN’S BENADRYL ALLERGY LIQUID (Generic Name: Diphenhydramine) (Antihistamine) NEVER GIVE TO INFANTS LESS THAN 6 MONTHS OLD. DO NOT GIVE TO CHILDREN LESS THAN 2 YEARS OLD UNLESS ADVISED BY A PHYSICIAN. Dosage: Every 4 -6 hours. -
Doxylamine Succinate-Pyridoxine Hydrochloride
Doxylamine succinate-pyridoxine hydrochloride This sheet is about exposure to doxylamine succinate-pyridoxine hydrochloride in pregnancy and while breastfeeding. This information should not take the place of medical care and advice from your healthcare providers. What is doxylamine succinate-pyridoxine hydrochloride? The combination of 10mg of doxylamine succinate and 10mg of pyridoxine hydrochloride is a medication used to treat nausea and vomiting of pregnancy (NVP), also called “morning sickness.” For more information on NVP, please see the MotherToBaby fact sheet Nausea and Vomiting of Pregnancy (https://mothertobaby.org/fact-sheets/nausea-vomiting-pregnancy-nvp/pdf/). Doxylamine succinate is an antihistamine. Antihistamines lessen the symptoms of allergic reactions and colds and help to treat insomnia (hard time sleeping). Pyridoxine hydrochloride is a form of vitamin B6. In the United States, the combination of doxylamine and pyridoxine has been sold under the name Diclegis® since 2013. In Canada, it has been sold under the brand name Diclectin®. Diclegis® and Diclectin® are delayed-release tablets available by prescription. Delayed-release means that the tablet coating prevents the ingredients from being absorbed too quickly by the body. Doxylamine succinate and/or pyridoxine hydrochloride may also be available as over-the- counter medicines. I take doxylamine succinate-pyridoxine hydrochloride. Can it make it harder for me to get pregnant? Based on the data available, it is not known if doxylamine succinate-pyridoxine hydrochloride can make it harder to become pregnant. I just found out I am pregnant. Should I stop taking doxylamine succinate-pyridoxine hydrochloride? Talk with your healthcare providers before making any changes to how you take your medication(s). -

Doxylamine/Pyridoxine
BonjestaTM (doxylamine/pyridoxine) – New Drug Approval • On November 7, 2016, the FDA approved Duchesnay’s Bonjesta (doxylamine/pyridoxine) for the treatment of nausea and vomiting of pregnancy in women who do not respond to conservative management. — Bonjesta has not been studied in women with hyperemesis gravidarum. • Bonjesta is a fixed dose combination product containing an antihistamine (doxylamine) and a vitamin B6 analog (pyridoxine). The exact mechanism of Bonjesta is not known. — Doxylamine/pyridoxine is also available as Diclegis®, which contains 10 mg of doxylamine and 10 mg of pyridoxine as delayed-release tablets for the same indication. • There have been no efficacy and safety trials for Bonjesta. However, a placebo-controlled study was conducted to support the safety and efficacy of 10 mg doxylamine succinate and 10 mg pyridoxine hydrochloride tablets (a different formulation and dosage strength than Bonjesta) in the treatment of nausea and vomiting of pregnancy. • Bonjesta is contraindicated in women with known hypersensitivity to doxylamine, other ethanolamine derivative antihistamines, or pyridoxine or any inactive ingredient in the formulation; monoamine oxidase (MAO) inhibitors intensify and prolong the adverse central nervous system effects of Bonjesta. • Warnings and precautions of Bonjesta include somnolence and concomitant medical conditions. • The most common adverse event (≥ 5% and exceeding placebo) with combination 10 mg doxylamine and 10 mg pyridoxine tablets was somnolence. • The recommended dose of Bonjesta is one tablet orally at bedtime on day 1. If the dose adequately controls symptoms the next day, the patient may continue taking one tablet daily at bedtime only. However, if symptoms persist on day 2, the dose may be increased to one tablet in the morning and one tablet at bedtime.