Spatial Analysis of HIV Infection and Associated Risk Factors in Botswana
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

GOVERNMENT of BOTSWANA/UNFPA 5Th COUNTRY PROGRAMME 2010-2016
25 September 2015 GOVERNMENT OF BOTSWANA/UNFPA 5th COUNTRY PROGRAMME 2010-2016 End of Programme Evaluation i Map of Botswana Consultant Team Position and Team Role Name Team Leader, plus Gender Component Helen Jackson Reproductive Health and Rights Component Thabo Phologolo Population and Development Component Enock Ngome ii Acknowledgements The evaluation team would like to thank UNFPA for the opportunity to undertake the GoB/UNFPA 5th Country Programme Evaluation. We would also like to express our great appreciation to all staff who gave generously of their time, both for interview and in providing documents, and in particular the evaluation manager. We greatly appreciate their support and guidance throughout and would also like to acknowledge the very helpful logistics support by administrative staff including the drivers. We also wish to express our gratitude to the members of the Evaluation Reference Group and to the many stakeholders in government, the UN and civil society for their flexibility and willingness to contribute their views, provide further documents, and generally assist the evaluation. The regional office, ESARO is acknowledged for financial and technical support for the evaluation. Last but not least, we appreciate the beneficiaries that we were able to meet who provided valuable insights into the programmes and how they had impacted on their lives. iii TABLE OF CONTENTS ACKNOWLEDGEMENTS .................................................................................................................................. -

Measuring Social Vulnerability to Natural Hazards at the District Level in Botswana
Jàmbá - Journal of Disaster Risk Studies ISSN: (Online) 2072-845X, (Print) 1996-1421 Page 1 of 11 Original Research Measuring social vulnerability to natural hazards at the district level in Botswana Authors: Social vulnerability to natural hazards has become a topical issue in the face of climate change. 1,2 Kakanyo F. Dintwa For disaster risk reduction strategies to be effective, prior assessments of social vulnerability Gobopamang Letamo2 Kannan Navaneetham2 have to be undertaken. This study applies the household social vulnerability methodology to measure social vulnerability to natural hazards in Botswana. A total of 11 indicators were Affiliations: used to develop the District Social Vulnerability Index (DSVI). Literature informed the 1 Environment Statistics Unit, selection of indicators constituting the model. The principal component analysis (PCA) Statistics Botswana, Gaborone, Botswana method was used to calculate indicators’ weights. The results of this study reveal that social vulnerability is mainly driven by size of household, disability, level of education, age, people 2Department of Population receiving social security, employment status, households status and levels of poverty, in that Studies, University of order. The spatial distribution of DSVI scores shows that Ngamiland West, Kweneng West Botswana, Gaborone, and Central Tutume are highly socially vulnerable. A correlation analysis was run between Botswana DSVI scores and the number of households affected by floods, showing a positive linear Corresponding author: correlation. The government, non-governmental organisations and the private sector should Kakanyo Dintwa, appreciate that social vulnerability is differentiated, and intervention programmes should [email protected] take cognisance of this. Dates: Keywords: Botswana; District Social Vulnerability; place vulnerability; natural hazards; Received: 21 Feb. -

2011 Population and Housing Census
2011 POPULATION AND HOUSING CENSUS Ministry of Finance and Development Planning 2011 Census Slogan: Palo yame, tsela ya ditlhabololo My count, a guide to developments August 2009 CSO in Collaboration with UNFPA PROJECT DOCUMENT 2011 POPULATION AND HOUSING CENSUS Published by Central Statistics Office Private Bag 0024, Gaborone Telephone: 33671300 Fax: 3952201 E-mail:[email protected] Website: www.cso.gov.bw Contact Unit : Census Secretariat Telephone: 3671300 Ext. 1305 August 2009 COPYRIGHT RESERVED Extracts may be published if source is duly acknowledged i CONTENTS PREFACE .................................................................................................................... 1 LIST OF ABBREVIATIONS AND ACRONYMS ....................................................... 2 EXECUTIVE SUMMARY ........................................................................................... 4 1. BACKGROUND AND JUSTIFICATION ................................................................ 5 1.1 Background of the 2011 Census Taking .............................................................. 5 1.2 Justification ......................................................................................................... 5 1.2.1 Evidence-based decision making, policy-making, planning and administration ....................................................................................................... 5 1.2.2 Research .................................................................................................... 5 1.2.3 Service to stakeholders -

Department of Road Transport and Safety Offices
DEPARTMENT OF ROAD TRANSPORT AND SAFETY OFFICES AND SERVICES MOLEPOLOLE • Registration & Licensing of vehicles and drivers • Driver Examination (Theory & Practical Tests) • Transport Inspectorate Tel: 5920148 Fax: 5910620 P/Bag 52 Molepolole Next to Molepolole Police MOCHUDI • Registration & Licensing of vehicles and drivers • Driver Examination (Theory & Practical Tests) • Transport Inspectorate P/Bag 36 Mochudi Tel : 5777127 Fax : 5748542 White House GABORONE Headquarters BBS Mall Plot no 53796 Tshomarelo House (Botswana Savings Bank) 1st, 2nd &3rd Floor Corner Lekgarapa/Letswai Road •Registration & Licensing of vehicles and drivers •Road safety (Public Education) Tel: 3688600/62 Fax : Fax: 3904067 P/Bag 0054 Gaborone GABORONE VTS – MARUAPULA • Registration & Licensing of vehicles and drivers • Driver Examination (Theory & Practical Tests) • Vehicle Examination Tel: 3912674/2259 P/Bag BR 318 B/Hurst Near Roads Training & Roads Maintenance behind Maruapula Flats GABORONE II – FAIRGROUNDS • Registration & Licensing of vehicles and drivers • Driver Examination : Theory Tel: 3190214/3911540/3911994 Fax : P/Bag 0054 Gaborone GABORONE - OLD SUPPLIES • Registration & Licensing of vehicles and drivers • Transport Permits • Transport Inspectorate Tel: 3905050 Fax :3932671 P/Bag 0054 Gaborone Plot 1221, Along Nkrumah Road, Near Botswana Power Corporation CHILDREN TRAFFIC SCHOOL •Road Safety Promotion for children only Tel: 3161851 P/Bag BR 318 B/Hurst RAMOTSWA •Registration & Licensing of vehicles and drivers •Driver Examination (Theory & Practical -

2011 Population & Housing Census Preliminary Results Brief
2011 Population & Housing Census Preliminary Results Brief For further details contact Census Office, Private Bag 0024 Gaborone: Tel 3188500; Fax 3188610 1. Botswana Population at 2 Million Botswana’s population has reached the 2 million mark. Preliminary results show that there were 2 038 228 persons enumerated in Botswana during the 2011 Population and Housing Census, compared with 1 680 863 enumerated in 2001. Suffice to note that this is the de-facto population – persons enumerated where they were found during enumeration. 2. General Comments on the Results 2.1 Population Growth The annual population growth rate 1 between 2001 and 2011 is 1.9 percent. This gives further evidence to the effect that Botswana’s population continues to increase at diminishing growth rates. Suffice to note that inter-census annual population growth rates for decennial censuses held from 1971 to 2001 were 4.6, 3.5 and 2.4 percent respectively. A close analysis of the results shows that it has taken 28 years for Botswana’s population to increase by one million. At the current rate and furthermore, with the current conditions 2 prevailing, it would take 23 years for the population to increase by another million - to reach 3 million. Marked differences are visible in district population annual growths, with estimated zero 3 growth for Selebi-Phikwe and Lobatse and a rate of over 4 percent per annum for South East District. Most district growth rates hover around 2 percent per annum. High growth rates in Kweneng and South East Districts have been observed, due largely to very high growth rates of villages within the proximity of Gaborone. -
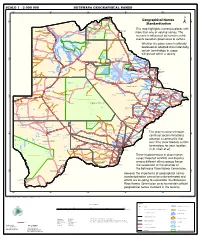
Geographical Names Standardization BOTSWANA GEOGRAPHICAL
SCALE 1 : 2 000 000 BOTSWANA GEOGRAPHICAL NAMES 20°0'0"E 22°0'0"E 24°0'0"E 26°0'0"E 28°0'0"E Kasane e ! ob Ch S Ngoma Bridge S " ! " 0 0 ' ' 0 0 ° Geographical Names ° ! 8 !( 8 1 ! 1 Parakarungu/ Kavimba ti Mbalakalungu ! ± n !( a Kakulwane Pan y K n Ga-Sekao/Kachikaubwe/Kachikabwe Standardization w e a L i/ n d d n o a y ba ! in m Shakawe Ngarange L ! zu ! !(Ghoha/Gcoha Gate we !(! Ng Samochema/Samochima Mpandamatenga/ This map highlights numerous places with Savute/Savuti Chobe National Park !(! Pandamatenga O Gudigwa te ! ! k Savu !( !( a ! v Nxamasere/Ncamasere a n a CHOBE DISTRICT more than one or varying names. The g Zweizwe Pan o an uiq !(! ag ! Sepupa/Sepopa Seronga M ! Savute Marsh Tsodilo !(! Gonutsuga/Gonitsuga scenario is influenced by human-centric Xau dum Nxauxau/Nxaunxau !(! ! Etsha 13 Jao! events based on governance or culture. achira Moan i e a h hw a k K g o n B Cakanaca/Xakanaka Mababe Ta ! u o N r o Moremi Wildlife Reserve Whether the place name is officially X a u ! G Gumare o d o l u OKAVANGO DELTA m m o e ! ti g Sankuyo o bestowed or adopted circumstantially, Qangwa g ! o !(! M Xaxaba/Cacaba B certain terminology in usage Nokaneng ! o r o Nxai National ! e Park n Shorobe a e k n will prevail within a society a Xaxa/Caecae/Xaixai m l e ! C u a n !( a d m a e a a b S c b K h i S " a " e a u T z 0 d ih n D 0 ' u ' m w NGAMILAND DISTRICT y ! Nxai Pan 0 m Tsokotshaa/Tsokatshaa 0 Gcwihabadu C T e Maun ° r ° h e ! 0 0 Ghwihaba/ ! a !( o 2 !( i ata Mmanxotae/Manxotae 2 g Botet N ! Gcwihaba e !( ! Nxharaga/Nxaraga !(! Maitengwe -
Republic of Botswana the Project for Enhancing National Forest Monitoring System for the Promotion of Sustainable Natural Resource Management
DEPARTMENT OF FORESTRY AND RANGE RESOURCES (DFRR) MINISTRY OF ENVIRONMENT, NATURAL RESOURCES CONSERVATION AND TOURISM (MENT) REPUBLIC OF BOTSWANA REPUBLIC OF BOTSWANA THE PROJECT FOR ENHANCING NATIONAL FOREST MONITORING SYSTEM FOR THE PROMOTION OF SUSTAINABLE NATURAL RESOURCE MANAGEMENT PROJECT COMPLETION REPORT DECEMBER 2017 JAPAN INTERNATIONAL COOPERATION AGENCY(JICA) ORIENTAL CONSULTANTS GLOBAL CO., LTD. JAPAN FOREST TECHNOLOGY ASSOCIATION GE JR 17-131 DEPARTMENT OF FORESTRY AND RANGE RESOURCES (DFRR) MINISTRY OF ENVIRONMENT, NATURAL RESOURCES CONSERVATION AND TOURISM (MENT) REPUBLIC OF BOTSWANA REPUBLIC OF BOTSWANA THE PROJECT FOR ENHANCING NATIONAL FOREST MONITORING SYSTEM FOR THE PROMOTION OF SUSTAINABLE NATURAL RESOURCE MANAGEMENT PROJECT COMPLETION REPORT DECEMBER 2017 JAPAN INTERNATIONAL COOPERATION AGENCY(JICA) ORIENTAL CONSULTANTS GLOBAL CO., LTD. JAPAN FOREST TECHNOLOGY ASSOCIATION DFRR/JICA: Botswana Forest Distribution Map Zambia Angola Zambia Legend KASANE Angola ! ! Settlement CountryBoundary Riparian Forest Typical Forest Woodland Zimbabwe Zimbabwe Bushland/Shrubland Savanna/Grassland/Forbs MAUN ! NATA Baregorund ! TUTUME ! Desert/Sand Dunes Marsh/Wetland FRANCISTOWN Waterbody/Pan ! ORAPA Namibia ! TONOTA ! GHANZI Angola Zambia Namibia ! SELEBI-PHIKWE BOBONONG ! ! Zimbabwe SEROWE ! PALAPYE ! Namibia MAHALAPYE ! South Africa KANG ! MOLEPOLOLE MOCHUDI ! ! JWANENG ! GABORONE ! ´ 0 50 100 200 RAMOTSWA ! KANYE Kilometres ! Coordinate System: GCS WGS 1984 Datum: WGS 1984 LOBATSE ! Botswana Forest Distribution Map Produced from -

List of Schools Visited for Monitoring Visits
LIST OF SCHOOLS VISITED FOR MONITORING VISITS CENTRAL INSPECTORAL AREA LOCATION NAME OF SCHOOL MMADINARE Diloro Diloro MMADINARE Mmadinare Kelele MMADINARE Kgagodi Kgagodi MMADINARE Mmadinare Mmadinare MMADINARE Mmadinare Phethu Mphoeng MMADINARE Robelela Robelela MMADINARE Gojwane Sedibe MMADINARE Serule Serule MMADINARE Mmadinare Tlapalakoma BOTETI Rakops Etsile BOTETI Khumaga Khumaga BOTETI Khwee Khwee BOTETI Mopipi Manthabakwe BOTETI Mmadikola Mmadikola BOTETI Letlhakane Mokane BOTETI Mokoboxane Mokoboxane BOTETI Mokubilo Mokubilo BOTETI Moreomaoto Moreomaoto BOTETI Mosu Mosu BOTETI Motlopi Motlopi BOTETI Letlhakane Retlhatloleng Selibe Phikwe Selibe Phikwe Boitshoko Selibe Phikwe Selibe Phikwe Boswelakgomo Selibe Phikwe Selibe Phikwe Phikwe Selibe Phikwe Selibe Phikwe Tebogo BOBIRWA Bobonong Bobonong BOBIRWA Gobojango Gobojango BOBIRWA Bobonong Mabumahibidu BOBIRWA Bobonong Madikwe BOBIRWA Mogapi Mogapi BOBIRWA Molalatau Molalatau BOBIRWA Bobonong Rasetimela BOBIRWA Semolale Semolale BOBIRWA Tsetsebye Tsetsebye 1 | P a g e MAHALAPYE WEST Bonwapitse Bonwapitse MAHALAPYE WEST Mahalapye Leetile MAHALAPYE WEST Mokgenene Mokgenene MAHALAPYE WEST Moralane Moralane MAHALAPYE WEST Mosolotshane Mosolotshane MAHALAPYE WEST Otse Setlhamo MAHALAPYE WEST Mahalapye St James MAHALAPYE WEST Mahalapye Tshikinyega MHALAPYE EAST Mahalapye Flowertown MHALAPYE EAST Mahalapye Mahalapye MHALAPYE EAST Matlhako Matlhako MHALAPYE EAST Mmaphashalala Mmaphashalala MHALAPYE EAST Sefhare Mmutle PALAPYE NORTH Goo-Sekgweng Goo-Sekgweng PALAPYE NORTH Goo-Tau Goo-Tau -

Ecosystem-Based Adaptation and Mitigation in Botswana's Communal
Ecosystem-Based Adaptation and Mitigation in Botswana’s Communal Rangelands ANNEX 6: Environmental and Social Impact Assessment (ESIA) and Environmental and Social Management Plan (ESMP) Prepared by Conservation International and C4 EcoSolutions through a PPF grant from the Green Climate Fund ESIA and ESMP Table of Contents 1. Executive summary .................................................................................................... 4 2. Introduction............................................................................................................... 9 3. Project Description .................................................................................................. 10 3.1. Strengthening community institutions and gender equitable capacity for collective action 11 3.2. Building individual capacity in herders and the community .......................................... 12 3.3. Supporting climate smart land and livestock management ........................................... 13 3.4. Strengthening mitigation & adaptive capacity across the value-chain for long-term sustainability.......................................................................................................................... 14 3.5. Knowledge sharing and mechanisms for continual improvement and replication .......... 15 4. Policy, legal and administrative framework ............................................................. 16 4.1. Governance, decentralisation and resource management instruments ......................... 16 4.2. Environmental -

SABONET Report No 18
ii Quick Guide This book is divided into two sections: the first part provides descriptions of some common trees and shrubs of Botswana, and the second is the complete checklist. The scientific names of the families, genera, and species are arranged alphabetically. Vernacular names are also arranged alphabetically, starting with Setswana and followed by English. Setswana names are separated by a semi-colon from English names. A glossary at the end of the book defines botanical terms used in the text. Species that are listed in the Red Data List for Botswana are indicated by an ® preceding the name. The letters N, SW, and SE indicate the distribution of the species within Botswana according to the Flora zambesiaca geographical regions. Flora zambesiaca regions used in the checklist. Administrative District FZ geographical region Central District SE & N Chobe District N Ghanzi District SW Kgalagadi District SW Kgatleng District SE Kweneng District SW & SE Ngamiland District N North East District N South East District SE Southern District SW & SE N CHOBE DISTRICT NGAMILAND DISTRICT ZIMBABWE NAMIBIA NORTH EAST DISTRICT CENTRAL DISTRICT GHANZI DISTRICT KWENENG DISTRICT KGATLENG KGALAGADI DISTRICT DISTRICT SOUTHERN SOUTH EAST DISTRICT DISTRICT SOUTH AFRICA 0 Kilometres 400 i ii Trees of Botswana: names and distribution Moffat P. Setshogo & Fanie Venter iii Recommended citation format SETSHOGO, M.P. & VENTER, F. 2003. Trees of Botswana: names and distribution. Southern African Botanical Diversity Network Report No. 18. Pretoria. Produced by University of Botswana Herbarium Private Bag UB00704 Gaborone Tel: (267) 355 2602 Fax: (267) 318 5097 E-mail: [email protected] Published by Southern African Botanical Diversity Network (SABONET), c/o National Botanical Institute, Private Bag X101, 0001 Pretoria and University of Botswana Herbarium, Private Bag UB00704, Gaborone. -
Soils and Land Suitability of the Motloutse Area Between Mmadinare and Bobonong
AG : BOT/85/011 FIELD DOCUMENT 6 Soil Mapping and Advisory Services Botswana SOILS AND LAND SUITABILITY OF THE MOTLOUTSE AREA BETWEEN MMADINARE AND BOBONONG FOOD Et AGRICULTURE UNITED NATIONS REPUBLIC OF ORGANIZATION OF THE DEVELOPMENT BOTSWANA UNITED NATIONS PROGRAMME GABORONE, 1990 AG: HOT/85/011 FIELD DOCUMENT 6 Soil Mapping and Advisory Services Botswana SOILS AND LAND SUITABILIT\ OftE IVIOTLOUT- AREA BETVVEEN IkIRIADINARE AND 3OL1ONON, by F. DE WIT an A. CAVALIERE-PARZANB7E FOOD AND AGRICULTURE ORGANIZATION OF THE UNT:_RD NATIONS UNITED NATIONS DEVELOPMENT PROGRAMY GOVE. NT OF POTSWANA Gaborone, 1990 The conclusions given in thisreport are those considered appropriate at the time of its preparation. They may be modified in the light of further knowledge gained at subsequent stages of this project. The definitions employed and-17- sentation of the ilaterial in s do not imply the expression o -pinion whatsoeve.: on the th,FociJ and Agricultural Organization the United Nations conce7:n' or consititutional statusofany country, territory or sea area ccrecn; the delimitation of frontiers. De Wit, P.V. , Cavaliere-Parzaneze, A., 1990. Soils and land suitability of the Motloutse area between Mmadinare and Bobonong. FAO/UNDP/Government of Botswana. Soil Mapping and Advisory Services Project AG: BOT/85/011, Field Document 6 . 104 pp, 2 maps Table of contents 1. THE SURVEY AREA ..............................................1 1.1 Location and infrastructure ..............................1 1.2 Climate 1.2.1 Rainfall and potential evapotranspiration -

Indigenous Peoples' Rights in Southern Africa
IWGIA INDIGENOUS PEOPLES’ RIGHTS IN INDIGENOUS PEOPLES’ RIGHTS SOUTHERN AFRICA IN SOUTHERN AFRICA Robert K. Hitchcock and Diana Vinding (Eds) This book is concerned with the first peo- ples (those people who are considered INDIGENOUS PEOPLES’ RIGHTS IN SOUTHERN AFRICA indigenous by themselves and others) of southern Africa such as the San, the Nama, and the Khoi, and their rights. It analyses the civil and political rights situation, assessing the extent to which these people benefit from such rights as compared to the wider society. The rights to land and to natural resources – or the lack of them – are an important focus of exploration and the book gives several examples of what the loss of these rights has meant for the existence and cultural identity of southern Africa’s indigenous men and women. Other themes addressed in the book are community-based natural resource management, education and the efforts being made in general by indigenous groups and their supporters to defend and promote indigenous rights. INTERNATIONAL WORK 1 GROUP FOR INDIGENOUS AFFAIRS IWGIA 2 INDIGENOUS PEOPLES’ RIGHTS IN SOUTHERN AFRICA Edited by Robert Hitchcock and Diana Vinding IWGIA Document No. 110 - Copenhagen 2004 3 INDIGENOUS PEOPLES’ RIGHTS IN SOUTHERN AFRICA Editors: Robert K. Hitchcock and Diana Vinding Copyright: IWGIA 2004 – All Rights Reserved Cover design, typesetting and maps: Jorge Monrás Proofreading: Elaine Bolton Prepress and Print: Eks/Skolens Trykkeri, Copenhagen, Denmark ISBN: 87-91563-08-9 Distribution in North America: Transaction Publishers 390 Campus Drive / Somerset, New Jersey 08873 www.transactionpub.com INTERNATIONAL WORK GROUP FOR INDIGENOUS AFFAIRS Classensgade 11 E, DK 2100 - Copenhagen, Denmark Tel: (45) 35 27 05 00 - Fax: (45) 35 27 05 07 E-mail: [email protected] - Web: www.iwgia.org 4 This book has been produced with financial support from the Danish Ministry of Foreign Affairs 5 CONTENTS Introduction Robert K.