Dermoscopy of Pigmented Skin Lesions (Part
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Clinical Features of Benign Tumors of the External Auditory Canal According to Pathology
Central Annals of Otolaryngology and Rhinology Research Article *Corresponding author Jae-Jun Song, Department of Otorhinolaryngology – Head and Neck Surgery, Korea University College of Clinical Features of Benign Medicine, 148 Gurodong-ro, Guro-gu, Seoul, 152-703, South Korea, Tel: 82-2-2626-3191; Fax: 82-2-868-0475; Tumors of the External Auditory Email: Submitted: 31 March 2017 Accepted: 20 April 2017 Canal According to Pathology Published: 21 April 2017 ISSN: 2379-948X Jeong-Rok Kim, HwibinIm, Sung Won Chae, and Jae-Jun Song* Copyright Department of Otorhinolaryngology-Head and Neck Surgery, Korea University College © 2017 Song et al. of Medicine, South Korea OPEN ACCESS Abstract Keywords Background and Objectives: Benign tumors of the external auditory canal (EAC) • External auditory canal are rare among head and neck tumors. The aim of this study was to analyze the clinical • Benign tumor features of patients who underwent surgery for an EAC mass confirmed as a benign • Surgical excision lesion. • Recurrence • Infection Methods: This retrospective study involved 53 patients with external auditory tumors who received surgical treatment at Korea University, Guro Hospital. Medical records and evaluations over a 10-year period were examined for clinical characteristics and pathologic diagnoses. Results: The most common pathologic diagnoses were nevus (40%), osteoma (13%), and cholesteatoma (13%). Among the five pathologic subgroups based on the origin organ of the tumor, the most prevalent pathologic subgroup was the skin lesion (47%), followed by the epithelial lesion (26%), and the bony lesion (13%). No significant differences were found in recurrence rate, recurrence duration, sex, or affected side between pathologic diagnoses. -
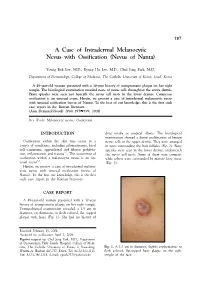
A Case of Intradermal Melanocytic Nevus with Ossification (Nevus of Nanta)
197 A Case of Intradermal Melanocytic Nevus with Ossification (Nevus of Nanta) Young Bok Lee, M.D., Kyung Ho Lee, M.D., Chul Jong Park, M.D. Department of Dermatology, College of Medicine, The Catholic University of Korea, Seoul, Korea A 49-year-old woman presented with a 30-year history of asymptomatic plaque on her right temple. The histological examination revealed nests of nevus cells throughout the entire dermis. Bony spicules were seen just beneath the nevus cell nests in the lower dermis. Cutaneous ossification is an unusual event. Herein, we present a case of intradermal melanocytic nevus with unusual ossification (nevus of Nanta). To the best of our knowledge, this is the first such case report in the Korean literature. (Ann Dermatol (Seoul) 20(4) 197∼199, 2008) Key Words: Melanocytic nevus, Ossification INTRODUCTION drug intake or medical illness. The histological examination showed a dense proliferation of benign Ossification within the skin may occur in a nevus cells in the upper dermis. They were arranged variety of conditions, including pilomatricoma, basal in nests surrounding the hair follicles (Fig. 2). Bony cell carcinoma, appendageal and fibrous prolifera- spicules were seen in the lower dermis, underneath 1,2 tion, inflammation and trauma . The occurrence of the nevus cell nests. Some of them were compact ossification within a melanocytic nevus is an un- while others were surrounded by mature fatty tissue 3-5 usual event . (Fig. 3). Herein, we present a case of intradermal melano- cytic nevus with unusual ossification (nevus of Nanta). To the best our knowledge, this is the first such case report in the Korean literature. -

Nevus Spilus: Is the Presence of Hair Associated with an Increased Risk for Melanoma?
Nevus Spilus: Is the Presence of Hair Associated With an Increased Risk for Melanoma? Robert Milton Gathings, MD; Raveena Reddy, MD; Ashish C. Bhatia, MD; Robert T. Brodell, MD PRACTICE POINTS • Nevus spilus (NS) appears as a café au lait macule studded with darker brown “moles.” • Although melanoma has been described in NS, it is rare. • There is no evidence that hairy NS are predisposed to melanoma. copy not Nevus spilus (NS), also known as speckled len- he term nevus spilus (NS), also known as tiginous nevus, is characterized by background speckled lentiginous nevus, was first used café au lait–like lentiginous melanocytic hyperpla- Tin the 19th century to describe lesions with sia speckled with small, 1- to 3-mm, darker foci.Do background café au lait–like lentiginous melanocytic Nevus spilus occurs in 1.3% to 2.3% of the adult hyperplasia speckled with small, 1- to 3-mm, darker population worldwide. Reports of melanoma aris- foci. The dark spots reflect lentigines; junctional, ing within hypertrichotic NS suggest that hyper- compound, and intradermal nevus cell nests; and trichosis may be a marker for the development of more rarely Spitz and blue nevi. Both macular and melanoma. We present a case of a hypertrichotic papular subtypes have been described.1 This birth- NS without melanoma and also provide a review of mark is quite common, occurring in 1.3% to 2.3% previously reported cases of hypertrichosis in NS. of the adult population worldwide.2 Hypertrichosis We believe that NS has aCUTIS lower risk for malignant has been described in NS.3-9 Two subsequent cases degeneration than congenital melanocytic nevi of malignant melanoma in hairy NS suggested that (CMN) of the same size, and it is unlikely that lesions may be particularly prone to malignant hypertrichosis is a marker for melanoma in NS. -

Acquired Bilateral Nevus of Ota–Like Macules (Hori's Nevus): a Case
Acquired Bilateral Nevus of Ota–like Macules (Hori’s Nevus): A Case Report and Treatment Update Jamie Hale, DO,* David Dorton, DO,** Kaisa van der Kooi, MD*** *Dermatology Resident, 2nd year, Largo Medical Center/NSUCOM, Largo, FL **Dermatologist, Teaching Faculty, Largo Medical Center/NSUCOM, Largo, FL ***Dermatopathologist, Teaching Faculty, Largo Medical Center/NSUCOM, Largo, FL Abstract This is a case of a 71-year-old African American female who presented with bilateral periorbital hyperpigmentation. After failing treatment with a topical retinoid and hydroquinone, a biopsy was performed and was consistent with acquired bilateral nevus of Ota-like macules, or Hori’s nevus. A review of histopathology, etiology, and treatment is discussed below. cream and tretinoin 0.05% gel. At this visit, a Introduction Figure 2 Acquired nevus of Ota-like macules (ABNOM), punch biopsy of her left zygoma was performed. or Hori’s nevus, clinically presents as bilateral, Histopathology reported sparse proliferation blue-gray to gray-brown macules of the zygomatic of irregularly shaped, haphazardly arranged melanocytes extending from the superficial area. It less often presents on the forehead, upper reticular dermis to mid-deep reticular dermis outer eyelids, and nose.1 It is most common in women of Asian descent and has been reported Figure 4 in ages 20 to 70. Classically, the eye and oral mucosa are uninvolved. This condition is commonly misdiagnosed as melasma.1 The etiology of this condition is not fully understood, and therefore no standardized treatment has been Figure 3 established. Case Report A 71-year-old African American female initially presented with a two week history of a pruritic, flaky rash with discoloration of her face. -

Short Course 11 Pigmented Lesions of the Skin
Rev Esp Patol 1999; Vol. 32, N~ 3: 447-453 © Prous Science, SA. © Sociedad Espafiola de Anatomfa Patol6gica Short Course 11 © Sociedad Espafiola de Citologia Pigmented lesions of the skin Chairperson F Contreras Spain Ca-chairpersons S McNutt USA and P McKee, USA. Problematic melanocytic nevi melanin pigment is often evident. Frequently, however, the lesion is solely intradermal when it may be confused with a fibrohistiocytic RH. McKee and F.R.C. Path tumor, particularly epithelloid cell fibrous histiocytoma (4). It is typi- cally composed of epitheliold nevus cells with abundant eosinophilic Brigham and Women’s Hospital, Harvard Medical School, Boston, cytoplasm and large, round, to oval vesicular nuclei containing pro- USA. minent eosinophilic nucleoli. Intranuclear cytoplasmic pseudoinclu- sions are common and mitotic figures are occasionally present. The nevus cells which are embedded in a dense, sclerotic connective tis- Whether the diagnosis of any particular nevus is problematic or not sue stroma, usually show maturation with depth. Less frequently the nevus is composed solely of spindle cells which may result in confu- depends upon a variety of factors, including the experience and enthusiasm of the pathologist, the nature of the specimen (shave vs. sion with atrophic fibrous histiocytoma. Desmoplastic nevus can be distinguished from epithelloid fibrous histiocytoma by its paucicellu- punch vs. excisional), the quality of the sections (and their staining), larity, absence of even a focal storiform growth pattern and SiQO pro- the hour of the day or day of the week in addition to the problems relating to the ever-increasing range of histological variants that we tein/HMB 45 expression. -

Optimal Management of Common Acquired Melanocytic Nevi (Moles): Current Perspectives
Clinical, Cosmetic and Investigational Dermatology Dovepress open access to scientific and medical research Open Access Full Text Article REVIEW Optimal management of common acquired melanocytic nevi (moles): current perspectives Kabir Sardana Abstract: Although common acquired melanocytic nevi are largely benign, they are probably Payal Chakravarty one of the most common indications for cosmetic surgery encountered by dermatologists. With Khushbu Goel recent advances, noninvasive tools can largely determine the potential for malignancy, although they cannot supplant histology. Although surgical shave excision with its myriad modifications Department of Dermatology and STD, Maulana Azad Medical College and has been in vogue for decades, the lack of an adequate histological sample, the largely blind Lok Nayak Hospital, New Delhi, Delhi, nature of the procedure, and the possibility of recurrence are persisting issues. Pigment-specific India lasers were initially used in the Q-switched mode, which was based on the thermal relaxation time of the melanocyte (size 7 µm; 1 µsec), which is not the primary target in melanocytic nevus. The cluster of nevus cells (100 µm) probably lends itself to treatment with a millisecond laser rather than a nanosecond laser. Thus, normal mode pigment-specific lasers and pulsed ablative lasers (CO2/erbium [Er]:yttrium aluminum garnet [YAG]) are more suited to treat acquired melanocytic nevi. The complexities of treating this disorder can be overcome by following a structured approach by using lasers that achieve the appropriate depth to treat the three subtypes of nevi: junctional, compound, and dermal. Thus, junctional nevi respond to Q-switched/normal mode pigment lasers, where for the compound and dermal nevi, pulsed ablative laser (CO2/ Er:YAG) may be needed. -

8.5 X12.5 Doublelines.P65
Cambridge University Press 978-0-521-87409-0 - Modern Soft Tissue Pathology: Tumors and Non-Neoplastic Conditions Edited by Markku Miettinen Index More information Index abdominal ependymoma, 744 mucinous cystadenocarcinoma, 631 adult fibrosarcoma (AF), 364–365, 1026 abdominal extrauterine smooth muscle ovarian adenocarcinoma, 72, 79 adult granulosa cell tumor, 523–524 tumors, 79 pancreatic adenocarcinoma, 846 clinical features, 523 abdominal inflammatory myofibroblastic pulmonary adenocarcinoma, 51 genetics, 524 tumors, 297–298 renal adenocarcinoma, 67 pathology, 523–524 abdominal leiomyoma, 467, 477 serous cystadenocarcinoma, 631 adult rhabdomyoma, 548–549 abdominal leiomyosarcoma. See urinary bladder/urogenital tract clinical features, 548 gastrointestinal stromal tumor adenocarcinoma, 72, 401 differential diagnosis, 549 (GIST) uterine adenocarcinomas, 72 genetics, 549 abdominal perivascular epithelioid cell tumors adenofibroma, 523 pathology, 548–549 (PEComas), 542 adenoid cystic carcinoma, 1035 aggressive angiomyxoma (AAM), 514–518 abdominal wall desmoids, 244 adenomatoid tumor, 811–813 clinical features, 514–516 acquired elastotic hemangioma, 598 adenomatous polyposis coli (APC) gene, 143 differential diagnosis, 518 acquired tufted angioma, 590 adenosarcoma (mullerian¨ adenosarcoma), 523 genetics, 518 acral arteriovenous tumor, 583 adipocytic lesions (cytology), 1017–1022 pathology, 516 acral myxoinflammatory fibroblastic sarcoma atypical lipomatous tumor/well- aggressive digital papillary adenocarcinoma, (AMIFS), 365–370, 1026 differentiated -

Nonpigmented Metastatic Melanoma in a Two-Year-Old Girl: a Serious Diagnostic Dilemma
Hindawi Publishing Corporation Case Reports in Oncological Medicine Volume 2015, Article ID 298273, 3 pages http://dx.doi.org/10.1155/2015/298273 Case Report Nonpigmented Metastatic Melanoma in a Two-Year-Old Girl: A Serious Diagnostic Dilemma Gulden Diniz,1 Hulya Tosun Yildirim,2 Selcen Yamaci,2 and Nur Olgun3 1 Izmir Tepecik Education and Research Hospital, Pathology Laboratory, Turkey 2Izmir Dr. Behcet Uz Children’s Hospital, Pathology Laboratory and Dermatology Clinics, Turkey 3Pediatric Oncology Clinics, Izmir Dokuz Eylul University, Turkey Correspondence should be addressed to Gulden Diniz; [email protected] Received 23 July 2014; Revised 20 January 2015; Accepted 21 January 2015 Academic Editor: Francesca Micci Copyright © 2015 Gulden Diniz et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Although rare, malignant melanoma may occur in children. Childhood melanomas account for only 0.3–3% of all melanomas. In particular the presence of congenital melanocytic nevi is associated with an increased risk of development of melanoma. We herein report a case of malignant melanoma that developed on a giant congenital melanocytic nevus and made a metastasis to the subcutaneous tissue of neck in a two-year-old girl. The patient was hospitalized for differential diagnosis and treatment of cervical mass with a suspicion of hematological malignancy, because the malignant transformation of congenital nevus was not noticed before. In this case, we found out a nonpigmented malignant tumor of pleomorphic cells after the microscopic examination of subcutaneous lesion. -
Pigmented Vulvar Lesions. Dermatoscopy. Is It Advisable?
"ISSVD - International Society for the Study of Vulvovaginal Disease " PIGMENTED VULVAR LESIONS. DERMATOSCOPY. IS IT ADVISABLE? Damian Ferrario MD. Dermatology Department. Italian Hospital of Buenos Aires Without Conflic Interest PIGMENTED VULVAR LESIONS • Pigmented skin lesions in the vulvar area include nevi, melanoma, melanotic macules (lentiginosis, melanosis), angiokeratomas, seborrheic keratosis, SeborrHeic keratosis AMNGT squamous cell carcinoma, basal cell carcinoma (BCC). • Atypical melanocytic nevi of the genital type (AMNGT) and vulvar melanomas usually affect postmenopausal women and the prognosis is poor. Melanosis Melanoma Pigmented lesions of the vulva are present in 20% of the women who Have Had gynecological examination. Even thougH vulvar pigmented lesions Has a benign prognosis, it causes concern to the patient and to the pHysician, owing to its melanoma-liKe presentation. Vulvar melanosis is the most frequent lesion among these pigmented disorders... but COLPOSCOPY You examine a 40-year-old patient and detect a nevus in the upper labia majora. According to Her, she Has it since childHood. She does not remember whether it grew or not. It is asymptomatic. WHAT IS YOUR BEHAVIOR? A. Do nothing and continue the examination. B. Urgently refer the patient to a dermatologist telling her it may be a melanoma. C. Performing radical You examine a 40-year-old patient and detect a nevus in the region of the labia surgery for suspected majora. According to Her, she Has it since childHood. He does not remember melanoma. whether He grew up. It is asymptomatic. D. Take a biopsy. A. Do nothing and continue the examination. B. Urgently refer the patient to a dermatologist telling her it may be a melanoma. -

Laser Dermatology
Laser Dermatology David J. Goldberg Editor Laser Dermatology Second Edition Editor David J. Goldberg, M.D. Division of New York & New Jersey Skin Laser & Surgery Specialists Hackensack , NY USA ISBN 978-3-642-32005-7 ISBN 978-3-642-32006-4 (eBook) DOI 10.1007/978-3-642-32006-4 Springer Heidelberg New York Dordrecht London Library of Congress Control Number: 2012954390 © Springer-Verlag Berlin Heidelberg 2013 This work is subject to copyright. All rights are reserved by the Publisher, whether the whole or part of the material is concerned, speci fi cally the rights of translation, reprinting, reuse of illustrations, recitation, broadcasting, reproduction on micro fi lms or in any other physical way, and transmission or information storage and retrieval, electronic adaptation, computer software, or by similar or dissimilar methodology now known or hereafter developed. Exempted from this legal reservation are brief excerpts in connection with reviews or scholarly analysis or material supplied speci fi cally for the purpose of being entered and executed on a computer system, for exclusive use by the purchaser of the work. Duplication of this publication or parts thereof is permitted only under the provisions of the Copyright Law of the Publisher’s location, in its current version, and permission for use must always be obtained from Springer. Permissions for use may be obtained through RightsLink at the Copyright Clearance Center. Violations are liable to prosecution under the respective Copyright Law. The use of general descriptive names, registered names, trademarks, service marks, etc. in this publication does not imply, even in the absence of a speci fi c statement, that such names are exempt from the relevant protective laws and regulations and therefore free for general use. -

A Nevus of OTA with Intraoral Involvement: a Rare Case Report
Shivare P. et al.: Nevus of OTA- a rare entity CASE REPORT A Nevus of OTA with Intraoral Involvement: A Rare Case Report Peeyush Shivhare1, Lata S.2, Monu Yadav3, Naqoosh Haidry4, Shruthi T. Patil5 1,5- Senior lecturer department of oral medicine and radiology, Narsinhbhai patel dental college and hospital, Visnagar, Gujarat. 2- Professor and head of the department, Rungta Correspondence to: College Of Dental Sciences And Research, Bhilai, Chhattisgarh. 3- PG student. Dr. Peeyush Shivhare Senior lecturer department of Department Of Oral Medicine And Radiology, Carrier Dental College And Hospital. oral medicine and radiology, Narsinhbhai patel dental Lucknow. 4- Senior lecturer department of maxillofacial surgery, Narsinhbhai patel college and hospital, Visnagar, Gujarat. dental college and hospital, Visnagar, Gujarat. Contact Us: www.ijohmr.com ABSTRACT Nevus of Ota, which originally was described by Ota and Tanino in 1939. It is characterized as congenital or acquired hamartoma of dermal melanocytes, presents clinically as a blue or gray patch on the face within the distribution of the ophthalmic and maxillary branches of the fifth cranial (trigeminal) nerve. Involvement of the palatal mucosa occurs rarely in nevus of Ota, when it occurs, it usually blends with the oral mucosa and is typically irregular, ill defined and often present as a mottled patch. Nevus of Ota is rare in the Indian subcontinent. So far very less cases of nevus of ota with intraoral involvement have been documented in the English literature. We report a rare case of intraoral nevus of Ota in a 20 year-old female patient. KEYWORDS: Nevus of Ota, Melanoma, Hamartoma, Glaucoma AA aaaasasasss INTRODUCTION The nevus of Ota (nevus fuscoceruleus ophthal- momaxillaris” or oculodermal melanocytosis) is a macular discoloration of the face, found most commonly in the Japanese people.1 Nevus of ota develops when the melanocyte get entrapped in the upper third of the dermis. -

Expert-Level Diagnosis of Nonpigmented Skin Cancer by Combined Convolutional Neural Networks
Supplementary Online Content Tschandl P, Rosendahl C, Akay BN, et al. Expert-level diagnosis of nonpigmented skin cancer by combined convolutional neural networks. JAMA Dermatol. Published online November 28, 2018. doi:10.1001/jamadermatol.2018.4378 eFigure. Sensitivities (Blue) and Specificities (Orange) at Different Threshold Cutoffs (Green) of the Combined Classifier Evaluated on the Validation Set eAppendix. Neural Network Training eTable 1. Complete List of Diagnoses and Their Frequencies Within the Test-Set eTable 2. Education of Users According to Their Experience Group eTable 3. Percent of Correct Prediction of the Malignancy Status for Specific Diagnoses of a CNN Using Either Close-up or Dermatoscopic Images This supplementary material has been provided by the authors to give readers additional information about their work. © 2018 American Medical Association. All rights reserved. Downloaded From: https://jamanetwork.com/ on 09/25/2021 eFigure. Sensitivities (Blue) and Specificities (Orange) at Different Threshold Cutoffs (Green) of the Combined Classifier Evaluated on the Validation Set A threshold cut at 0.2 (black) is found for a minimum of 51.3% specificity. © 2018 American Medical Association. All rights reserved. Downloaded From: https://jamanetwork.com/ on 09/25/2021 eAppendix. Neural Network Training We compared multiple architecture and training hyperparameter combinations in a grid-search fashion, and used only the single best performing network for dermoscopic and close-up images, based on validation accuracy, for further analyses. We trained four different CNN architectures (InceptionResNetV2, InceptionV3, Xception, ResNet50) and used model definitions and ImageNet pretrained weights as available in the Tensorflow (version 1.3.0)/ Keras (version 2.0.8) frameworks.