Oral Pathology
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Head and Neck Mucosal Melanoma
www.melanomafocus.com Head and Neck Mucosal Melanoma Information for patients and carers Introduction Head and Neck The information in this leaflet relates specifically to melanomas of the head Mucosal and neck mucous membranes. The leaflet summarises a guideline (melanomafocus. Melanoma com/activities/mucosal-guidelines/mucosal- melanoma-resources) developed by experts in the field to advise cancer specialists who treat patients with this condition and is based upon the best evidence available. Skin What is it? cancers can also develop in the same areas of Melanoma develops if there is uncontrolled These melanomas are different in several the body, in the skin rather than in the mucous growth of melanocytes, the cells responsible ways from skin melanomas. For example, membranes. These are known as cutaneous for pigmenting (darkening) the skin. Mucosal while the risk of getting skin melanoma is melanomas and are not covered by this melanoma is a kind of melanoma that increased by too much exposure to the sun, guideline. If you have been diagnosed with occurs in mucous membranes. These are there appears to be no link between sunlight a skin (cutaneous) melanoma please refer to the moist surfaces that line cavities within and mucosal melanomas. No specific causes the NICE guideline (nice.org.uk/guidance/ the body. Mucosal melanomas can occur in or links with lifestyle have been found for ng14) and the other organisations listed at the the mouth (oral mucosal melanoma), nasal mucosal melanoma and as far as we know end of this leaflet. passages (sinonasal mucosal melanoma) there is nothing you can do to prevent it. -
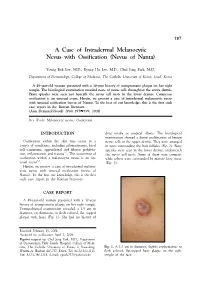
A Case of Intradermal Melanocytic Nevus with Ossification (Nevus of Nanta)
197 A Case of Intradermal Melanocytic Nevus with Ossification (Nevus of Nanta) Young Bok Lee, M.D., Kyung Ho Lee, M.D., Chul Jong Park, M.D. Department of Dermatology, College of Medicine, The Catholic University of Korea, Seoul, Korea A 49-year-old woman presented with a 30-year history of asymptomatic plaque on her right temple. The histological examination revealed nests of nevus cells throughout the entire dermis. Bony spicules were seen just beneath the nevus cell nests in the lower dermis. Cutaneous ossification is an unusual event. Herein, we present a case of intradermal melanocytic nevus with unusual ossification (nevus of Nanta). To the best of our knowledge, this is the first such case report in the Korean literature. (Ann Dermatol (Seoul) 20(4) 197∼199, 2008) Key Words: Melanocytic nevus, Ossification INTRODUCTION drug intake or medical illness. The histological examination showed a dense proliferation of benign Ossification within the skin may occur in a nevus cells in the upper dermis. They were arranged variety of conditions, including pilomatricoma, basal in nests surrounding the hair follicles (Fig. 2). Bony cell carcinoma, appendageal and fibrous prolifera- spicules were seen in the lower dermis, underneath 1,2 tion, inflammation and trauma . The occurrence of the nevus cell nests. Some of them were compact ossification within a melanocytic nevus is an un- while others were surrounded by mature fatty tissue 3-5 usual event . (Fig. 3). Herein, we present a case of intradermal melano- cytic nevus with unusual ossification (nevus of Nanta). To the best our knowledge, this is the first such case report in the Korean literature. -

Sinonasal Neoplasms Mohit Agarwal, MD,* and Bruno Policeni, MD†
Sinonasal Neoplasms Mohit Agarwal, MD,* and Bruno Policeni, MD† Introduction benign lesions will usually cause bone remodeling and/or scle- rosis. Loss of bright fat marrow intensity on T1W MR images f Rip Van Winkle went to medical school during the 80s is a sign of bone involvement. Differentiation of benign vs I and woke up today among a meeting of pathologists, he malignant lesions remains a challenge with imaging and excep- would think he was on a different planet and listening to an tions to the previously mentioned features exist. Pathology is “ ” alien language. The once pink and purple world of pathol- required to determine the diagnosis in the majority of cases.7 ogy is now extensively multicolored with an overwhelming Imaging has more to offer than just histological diagnosis, number of immunostains and molecular markers. Histologi- the most important of which is tumor mapping. It must be cal diagnoses now come with an alphanumeric tail, each determined if the tumor is confined within a single sinus or implying the unique gene expression associated with that if there is extension into surrounding structures. Tumors of tumor entity. Needless to say, similar things have happened the maxillary sinuses can extend to the anterior ethmoid fi to the new fourth edition WHO classi cation of sinonasal sinus, nasal cavity, and orbit. Anterior ethmoid tumors can fi (SN) neoplasms, where SMARC B1-de cient carcinoma, involve the frontal sinuses and the nasal cavity. Nasal cavity Nuclear protein testis (NUT) midline carcinoma, and human tumors commonly involve the ethmoid sinus. Posterior eth- papilloma virus (HPV)-related multiphenotypic SN carci- moid tumors tend to involve the sphenoid sinus.7 1 noma have found a place. -

Short Course 11 Pigmented Lesions of the Skin
Rev Esp Patol 1999; Vol. 32, N~ 3: 447-453 © Prous Science, SA. © Sociedad Espafiola de Anatomfa Patol6gica Short Course 11 © Sociedad Espafiola de Citologia Pigmented lesions of the skin Chairperson F Contreras Spain Ca-chairpersons S McNutt USA and P McKee, USA. Problematic melanocytic nevi melanin pigment is often evident. Frequently, however, the lesion is solely intradermal when it may be confused with a fibrohistiocytic RH. McKee and F.R.C. Path tumor, particularly epithelloid cell fibrous histiocytoma (4). It is typi- cally composed of epitheliold nevus cells with abundant eosinophilic Brigham and Women’s Hospital, Harvard Medical School, Boston, cytoplasm and large, round, to oval vesicular nuclei containing pro- USA. minent eosinophilic nucleoli. Intranuclear cytoplasmic pseudoinclu- sions are common and mitotic figures are occasionally present. The nevus cells which are embedded in a dense, sclerotic connective tis- Whether the diagnosis of any particular nevus is problematic or not sue stroma, usually show maturation with depth. Less frequently the nevus is composed solely of spindle cells which may result in confu- depends upon a variety of factors, including the experience and enthusiasm of the pathologist, the nature of the specimen (shave vs. sion with atrophic fibrous histiocytoma. Desmoplastic nevus can be distinguished from epithelloid fibrous histiocytoma by its paucicellu- punch vs. excisional), the quality of the sections (and their staining), larity, absence of even a focal storiform growth pattern and SiQO pro- the hour of the day or day of the week in addition to the problems relating to the ever-increasing range of histological variants that we tein/HMB 45 expression. -

Melanoma Review
Philip J. Bergman DVM, MS, PhD Diplomate ACVIM-Oncology Director, Clinical Studies, VCA Antech Medical Director, Katonah-Bedford Veterinary Center (#893) 546 North Bedford Rd., Bedford Hills, NY 10507 Office 914-241-7700, Fax 914-241-7708 Adjunct Associate, Memorial Sloan-Kettering Cancer Center, NYC MELANOMA REVIEW Melanomas in dogs have extremely diverse biologic behaviors depending on a variety of factors. A greater understanding of these factors significantly helps the clinician to delineate in advance the appropriate staging, prognosis and treatments. The primary factors which determine the biologic behavior of a melanoma in a dog are site, size, stage and histologic parameters. Unfortunately, even with an understanding of all of these factors, there will be occasional melanomas which have an unreliable biologic behavior; hence the desperate need for additional research into this relatively common (~ 4% of all canine tumors), heterogeneous, but frequently extremely malignant tumor. This review will assume the diagnosis of melanoma has already been made, which in of itself can be fraught with difficulty, and will focus on the aforementioned biologic behavior parameters, the staging and the treatment of canine melanoma. Biologic Behavior The biologic behavior of canine melanoma is extremely variable and best characterized based on anatomic site, size, stage and histologic parameters. On divergent ends of the spectrum would be a 0.5 cm haired-skin melanoma with an extremely low grade likely to be cured with simple surgical removal vs. a 5.0 cm high-grade malignant oral melanoma with a poor-grave prognosis. Similar to the development of a rational staging, prognostic and therapeutic plan for any tumor, two primary questions must be answered; what is the local invasiveness of the tumor and what is the metastatic propensity? The answers to these questions will determine the prognosis, and to be discussed later, the treatment. -

Identification of HRAS Mutations and Absence of GNAQ Or GNA11
Modern Pathology (2013) 26, 1320–1328 1320 & 2013 USCAP, Inc All rights reserved 0893-3952/13 $32.00 Identification of HRAS mutations and absence of GNAQ or GNA11 mutations in deep penetrating nevi Ryan P Bender1, Matthew J McGinniss2, Paula Esmay1, Elsa F Velazquez3,4 and Julie DR Reimann3,4 1Caris Life Sciences, Phoenix, AZ, USA; 2Genoptix Medical Laboratory, Carlsbad, CA, USA; 3Dermatopathology Division, Miraca Life Sciences Research Institute, Newton, MA, USA and 4Department of Dermatology, Tufts Medical Center, Boston, MA, USA HRAS is mutated in B15% of Spitz nevi, and GNAQ or GNA11 is mutated in blue nevi (46–83% and B7% respectively). Epithelioid blue nevi and deep penetrating nevi show features of both blue nevi (intradermal location, pigmentation) and Spitz nevi (epithelioid morphology). Epithelioid blue nevi and deep penetrating nevi can also show overlapping features with melanoma, posing a diagnostic challenge. Although epithelioid blue nevi are considered blue nevic variants, no GNAQ or GNA11 mutations have been reported. Classification of deep penetrating nevi as blue nevic variants has also been proposed, however, no GNAQ or GNA11 mutations have been reported and none have been tested for HRAS mutations. To better characterize these tumors, we performed mutational analysis for GNAQ, GNA11, and HRAS, with blue nevi and Spitz nevi as controls. Within deep penetrating nevi, none demonstrated GNAQ or GNA11 mutations (0/38). However, 6% revealed HRAS mutation (2/32). Twenty percent of epithelioid blue nevi contained a GNAQ mutation (2/10), while none displayed GNA11 or HRAS mutation. Eighty-seven percent of blue nevi contained a GNAQ mutation (26/30), 4% a GNA11 mutation (1/28), and none an HRAS mutation. -

Melanomas Are Comprised of Multiple Biologically Distinct Categories
Melanomas are comprised of multiple biologically distinct categories, which differ in cell of origin, age of onset, clinical and histologic presentation, pattern of metastasis, ethnic distribution, causative role of UV radiation, predisposing germ line alterations, mutational processes, and patterns of somatic mutations. Neoplasms are initiated by gain of function mutations in one of several primary oncogenes, typically leading to benign melanocytic nevi with characteristic histologic features. The progression of nevi is restrained by multiple tumor suppressive mechanisms. Secondary genetic alterations override these barriers and promote intermediate or overtly malignant tumors along distinct progression trajectories. The current knowledge about pathogenesis, clinical, histological and genetic features of primary melanocytic neoplasms is reviewed and integrated into a taxonomic framework. THE MOLECULAR PATHOLOGY OF MELANOMA: AN INTEGRATED TAXONOMY OF MELANOCYTIC NEOPLASIA Boris C. Bastian Corresponding Author: Boris C. Bastian, M.D. Ph.D. Gerson & Barbara Bass Bakar Distinguished Professor of Cancer Biology Departments of Dermatology and Pathology University of California, San Francisco UCSF Cardiovascular Research Institute 555 Mission Bay Blvd South Box 3118, Room 252K San Francisco, CA 94158-9001 [email protected] Key words: Genetics Pathogenesis Classification Mutation Nevi Table of Contents Molecular pathogenesis of melanocytic neoplasia .................................................... 1 Classification of melanocytic neoplasms -

Clinical Characteristics of Malignant Melanoma in Central China and Predictors of Metastasis
1452 ONCOLOGY LETTERS 19: 1452-1464, 2020 Clinical characteristics of malignant melanoma in central China and predictors of metastasis KE SHI1, XURAN ZHU1, ZHONGYANG LIU1, NAN SUN1, LUOSHA GU1, YANG WEI1, XU CHENG1, ZEWEI ZHANG1, BAIHUI XIE1, SHUAIXI YANG2, GUANGSHUAI LI1 and LINBO LIU1 Departments of 1Plastic Surgery and 2Anorectal Surgery, The First Affiliated Hospital of Zhengzhou University, Zhengzhou, Henan 450052, P.R. China Received November 5, 2018; Accepted November 13, 2019 DOI: 10.3892/ol.2019.11219 Abstract. Cutaneous malignant melanoma (MM) is the Introduction most malignant type of all skin neoplasms. There is wide variability in the characteristics of MM between patients of Malignant melanoma (MM) is a highly aggressive cancer different races. The aim of the present study was to investigate derived from neural crest melanocytes and occurs most the clinicopathological characteristics of patients with MM in frequently in the skin, digestive tract, eyes, genitals and nasal central China and to assess the value of specific hematological cavity (1-3) The prognosis of patients with MM is poor and and biochemical indices for predicting metastasis. The data the 5-year survival is reported to be <20% (4). Each year, of 167 patients with MM from the First Affiliated Hospital ~20,000 cases of cutaneous MM are reported in China and of Zhengzhou University (Henan, China) were retrospectively the incidence is growing by 3-5% per year (5). The incidence analyzed and compared with the data of patients with MM of MM is lower in China compared with Western countries, available from cBioPortal for Cancer Genomics. Following but survival is shorter in Chinese patients (6,7). -
Mucosal Melanoma: a Clinically and Biologically Unique Disease Entity
Focused 345 Review Mucosal Melanoma: A Clinically and Biologically Unique Disease Entity Richard D. Carvajal, MDa; Sharon A. Spencer, MDb; and William Lydiatt, MD,c New York, New York; Birmingham, Alabama; and Omaha, Nebraska Key Words of these arise from mucosal surfaces.1–3 Despite a com- Mucosal melanoma, melanoma of the head and neck, anorectal mon cell of origin, MM is a clinical and pathologic entity melanoma, vulvovaginal melanoma, KIT distinct from its more common cutaneous counterpart. MM can arise from any mucosal surface of the body, with Abstract 55% arising from the head and neck, 24% from the ano- Mucosal melanoma (MM) is an aggressive and clinically complex 2 malignancy made more challenging by its relative rarity. Because rectal mucosa, and 18% from the vulvovaginal mucosa. of the rarity of MM as a whole, and because of the unique biology Disease arising from the mucosa of the pharynx, larynx, and clinical challenges of MM arising from each anatomic location, urinary tract, cervix, esophagus, gallbladder, or other mu- understanding of this disease and its optimal management remains cosal sites is less common. limited. The impact of various treatment strategies on disease con- This article summarizes the clinical, pathologic, and trol and survival has been difficult to assess because of the small size of most reported series of MM arising from any one particular site, molecular features, and the diagnostic and therapeutic the retrospective nature of most series, and the lack of a uniform considerations for the management of MM, underscoring comprehensive staging system for this disease. This article summa- the similarities and differences from cutaneous melanoma rizes the clinical, pathologic, and molecular features, and the diag- (CM). -

Lymphatic Invasion and Angiotropism in Primary Cutaneous Melanoma Andrea P Moy, Lyn M Duncan and Stefan Kraft
Laboratory Investigation (2017) 97, 118–129 © 2017 USCAP, Inc All rights reserved 0023-6837/17 $32.00 PATHOBIOLOGY IN FOCUS Lymphatic invasion and angiotropism in primary cutaneous melanoma Andrea P Moy, Lyn M Duncan and Stefan Kraft Access of melanoma cells to the cutaneous vasculature either via lymphatic invasion or angiotropism is a proposed mechanism for metastasis. Lymphatic invasion is believed to be a mechanism by which melanoma cells can disseminate to regional lymph nodes and to distant sites and may be predictive of adverse outcomes. Although it can be detected on hematoxylin- and eosin-stained sections, sensitivity is markedly improved by immunohistochemistry for lymphatic endothelial cells. Multiple studies have reported a significant association between the presence of lymphatic invasion and sentinel lymph node metastasis and survival. More recently, extravascular migratory metastasis has been suggested as another means by which melanoma cells can spread. Angiotropism, the histopathologic correlate of extravascular migratory metastasis, has also been associated with melanoma metastasis and disease recurrence. Although lymphatic invasion and angiotropism are not currently part of routine melanoma reporting, the detection of these attributes using ancillary immunohistochemical stains may be useful in therapeutic planning for patients with melanoma. Laboratory Investigation (2017) 97, 118–129; doi:10.1038/labinvest.2016.131; published online 19 December 2016 Primary cutaneous melanoma has a propensity for metastasis, However, -

Nevus of Ota in Children
PEDIATRIC DERMATOLOGY Series Editor: Camila K. Janniger, MD Nevus of Ota in Children Smeeta Sinha, MD; Philip J. Cohen, MD; Robert A. Schwartz, MD, MPH Nevus of Ota, synonymously termed oculodermal seen most commonly in individuals of Japanese melanosis, is an uncommon dermal melanosis descent, and is less likely to present in individuals most commonly seen at birth in children of of Chinese or Korean descent, though individuals Japanese descent, though it can affect individu- descending from the Indian subcontinent, Africa, als of any age or ethnicity. The disease tends to and Europe also may be affected.7 In early sur- persist and extend locally, becoming increasingly veys of Japanese patients at dermatology clinics, prominent with age, puberty, and postmenopausal the incidence of nevus of Ota was determined to state. Treatment should begin early after diagno- be 0.4% (110/27,500).4 Cowan and Balistocky8 sis using multiple sessions of laser photother- calculated the incidence of oculodermal melano- molysis to avoid darkening and extension of the cytosis in black patients to be 0.016%. A study of lesion. Important associated disorders include 2914 Chinese children in Calgary, Alberta, Canada, ipsilateral glaucoma; intracranial melanocyto- reported an incidence of oculodermal melanocytosis sis; and rarely cutaneous, ocular, or intracranial of 0.034% (1/2914).9 melanoma. Recommendations are discussed for managing nevus of Ota in children. Clinical Manifestation Cutis. 2008;82:25-29. The typical nevus of Ota is a unilateral facial dis- coloration that is macular, speckled, and bluish gray or brown, with edges that blend with bordering skin evus of Ota is a rare disorder characterized (Figure).10 The dermatomal distribution of pigment by melanocytic pigmentation of the sclera characterizes this diagnosis in most cases. -

Blue Nevi and Melanomas Natural Blue BLUE NEVUS Blue Nevus (BN)
KJ Busam, M.D. Paris, 2017 Blue Nevi and Melanomas Natural Blue BLUE NEVUS Blue Nevus (BN) • Spectrum of blue nevi – Common, Sclerosing, Epithelioid, Cellular, Plaque type blue nevi • Differential diagnosis – Melanoma ex BN or simulating BN – BN vs other tumors – Biphenotypic/collision lesions Common Blue Nevus Clinical: - Circumscribed small bluish macule/papule - Preferred sites: Scalp, wrist, foot Pathology: - Predominantly reticular dermal lesion - Pigmented fusiform and dendritic cells - Admixed melanophages - Bland cytology Common Blue Nevus Blue Nevus Sclerosing Blue Nevus Pigm BN Cellular Blue Nevus - 49 yo woman - Buttock nodule CBN Cellular Blue Nevus Thrombi and stromal edema Multinucleated giant melanocytes Cellular Blue Nevus Hemorrhagic cystic (“aneurysmal”) change Amelanotic Cellular Blue Nevus 19 yo man with buttock lesion Atypical CBN Plaque-Type Blue Nevus Plaque-type Blue Nevus Plaque Type Blue Nevus Mucosal Blue Nevus Conjunctival Blue Nevus Nodal Blue Nevus Combined epithelioid BN Blue Nevus • M Tieche 1906; Virchow Arch Pathol Anat “Blaue Naevus” • B Upshaw 1947; Surgery “Extensive Blue Nevus” (plaque-type BN) • A Allen 1949; Cancer “ Cellular Blue Nevus” Blue Nevus – Mutation Analysis Type of Lesion GNAQ GNA11 Number Common BN 6.7% 65% 60 Cellular BN 8.3% 72.2% 36 Amelanotic BN 0% 70% 10 Nevus of Ota 5% 10% 20 Nevus of Ito 16.7% 0% 7 TOTAL 6.5% 55% 139 Van Raamsdonk et al NEJM 2010; 2191-9 Blue Nevus – Mutation Analysis Type of Blue Nevus GNAQ Number Common Blue Nevus 40% 4/10 Cellular Blue Nevus 44% 4/9 Hypomelanotic