Nevus of Ota – an Intraoral Presentation: a Case Report Jennifer Maguire1* and Deborah Holt2
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
A Case of Intradermal Melanocytic Nevus with Ossification (Nevus of Nanta)
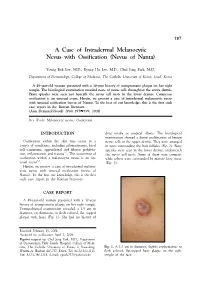
197 A Case of Intradermal Melanocytic Nevus with Ossification (Nevus of Nanta) Young Bok Lee, M.D., Kyung Ho Lee, M.D., Chul Jong Park, M.D. Department of Dermatology, College of Medicine, The Catholic University of Korea, Seoul, Korea A 49-year-old woman presented with a 30-year history of asymptomatic plaque on her right temple. The histological examination revealed nests of nevus cells throughout the entire dermis. Bony spicules were seen just beneath the nevus cell nests in the lower dermis. Cutaneous ossification is an unusual event. Herein, we present a case of intradermal melanocytic nevus with unusual ossification (nevus of Nanta). To the best of our knowledge, this is the first such case report in the Korean literature. (Ann Dermatol (Seoul) 20(4) 197∼199, 2008) Key Words: Melanocytic nevus, Ossification INTRODUCTION drug intake or medical illness. The histological examination showed a dense proliferation of benign Ossification within the skin may occur in a nevus cells in the upper dermis. They were arranged variety of conditions, including pilomatricoma, basal in nests surrounding the hair follicles (Fig. 2). Bony cell carcinoma, appendageal and fibrous prolifera- spicules were seen in the lower dermis, underneath 1,2 tion, inflammation and trauma . The occurrence of the nevus cell nests. Some of them were compact ossification within a melanocytic nevus is an un- while others were surrounded by mature fatty tissue 3-5 usual event . (Fig. 3). Herein, we present a case of intradermal melano- cytic nevus with unusual ossification (nevus of Nanta). To the best our knowledge, this is the first such case report in the Korean literature. -

Acquired Bilateral Nevus of Ota–Like Macules (Hori's Nevus): a Case
Acquired Bilateral Nevus of Ota–like Macules (Hori’s Nevus): A Case Report and Treatment Update Jamie Hale, DO,* David Dorton, DO,** Kaisa van der Kooi, MD*** *Dermatology Resident, 2nd year, Largo Medical Center/NSUCOM, Largo, FL **Dermatologist, Teaching Faculty, Largo Medical Center/NSUCOM, Largo, FL ***Dermatopathologist, Teaching Faculty, Largo Medical Center/NSUCOM, Largo, FL Abstract This is a case of a 71-year-old African American female who presented with bilateral periorbital hyperpigmentation. After failing treatment with a topical retinoid and hydroquinone, a biopsy was performed and was consistent with acquired bilateral nevus of Ota-like macules, or Hori’s nevus. A review of histopathology, etiology, and treatment is discussed below. cream and tretinoin 0.05% gel. At this visit, a Introduction Figure 2 Acquired nevus of Ota-like macules (ABNOM), punch biopsy of her left zygoma was performed. or Hori’s nevus, clinically presents as bilateral, Histopathology reported sparse proliferation blue-gray to gray-brown macules of the zygomatic of irregularly shaped, haphazardly arranged melanocytes extending from the superficial area. It less often presents on the forehead, upper reticular dermis to mid-deep reticular dermis outer eyelids, and nose.1 It is most common in women of Asian descent and has been reported Figure 4 in ages 20 to 70. Classically, the eye and oral mucosa are uninvolved. This condition is commonly misdiagnosed as melasma.1 The etiology of this condition is not fully understood, and therefore no standardized treatment has been Figure 3 established. Case Report A 71-year-old African American female initially presented with a two week history of a pruritic, flaky rash with discoloration of her face. -

Short Course 11 Pigmented Lesions of the Skin
Rev Esp Patol 1999; Vol. 32, N~ 3: 447-453 © Prous Science, SA. © Sociedad Espafiola de Anatomfa Patol6gica Short Course 11 © Sociedad Espafiola de Citologia Pigmented lesions of the skin Chairperson F Contreras Spain Ca-chairpersons S McNutt USA and P McKee, USA. Problematic melanocytic nevi melanin pigment is often evident. Frequently, however, the lesion is solely intradermal when it may be confused with a fibrohistiocytic RH. McKee and F.R.C. Path tumor, particularly epithelloid cell fibrous histiocytoma (4). It is typi- cally composed of epitheliold nevus cells with abundant eosinophilic Brigham and Women’s Hospital, Harvard Medical School, Boston, cytoplasm and large, round, to oval vesicular nuclei containing pro- USA. minent eosinophilic nucleoli. Intranuclear cytoplasmic pseudoinclu- sions are common and mitotic figures are occasionally present. The nevus cells which are embedded in a dense, sclerotic connective tis- Whether the diagnosis of any particular nevus is problematic or not sue stroma, usually show maturation with depth. Less frequently the nevus is composed solely of spindle cells which may result in confu- depends upon a variety of factors, including the experience and enthusiasm of the pathologist, the nature of the specimen (shave vs. sion with atrophic fibrous histiocytoma. Desmoplastic nevus can be distinguished from epithelloid fibrous histiocytoma by its paucicellu- punch vs. excisional), the quality of the sections (and their staining), larity, absence of even a focal storiform growth pattern and SiQO pro- the hour of the day or day of the week in addition to the problems relating to the ever-increasing range of histological variants that we tein/HMB 45 expression. -

Oral Pathology
Oral Pathology Palatal blue nevus in a child Catherine M. Flaitz DDS, MS Georgeanne McCandless DDS Dr. Flaitz is professor, Oral and Maxillofacial Pathology and Pediatric Dentistry, Department of Stomatology, University of Texas at Houston Health Science Center Dental Branch; Dr. McCandless has a private practice in The Woodlands, TX. Correspond with Dr. Flaitz at [email protected] Abstract The intraoral blue nevus occurs infrequently in children. This by the labial mucosa (1). Intraoral lesions have a predilection case report describes the clinical features of an acquired blue ne- for females in the third and fourth decades, in contrast to cu- vus in a 7 year-old girl that involved the palatal mucosa. A taneous lesions that normally develop in children. In large differential diagnosis and justification for surgical excision of this biopsy series, only 2% of the oral blue nevi are diagnosed in oral lesion are discussed. (Pediatr Dent 23:354-355, 2001) children and adolescents (1). Similar to their cutaneous coun- terpart, most oral lesions are acquired; however, there are ith the exception of vascular entities, neoplastic isolated reports of congenital examples. lesions with a blue discoloration are an unusual find Clinically, most lesions present as a solitary blue, gray or Wing in children. Although the blue nevus is a blue-black macule or slightly raised nodule that measures less relatively common finding of the skin in the pediatric popula- than 6 mm in size. The margins are often regular but indis- tion, only a few intraoral examples are documented in the tinct and the surface is smooth. -

Optimal Management of Common Acquired Melanocytic Nevi (Moles): Current Perspectives
Clinical, Cosmetic and Investigational Dermatology Dovepress open access to scientific and medical research Open Access Full Text Article REVIEW Optimal management of common acquired melanocytic nevi (moles): current perspectives Kabir Sardana Abstract: Although common acquired melanocytic nevi are largely benign, they are probably Payal Chakravarty one of the most common indications for cosmetic surgery encountered by dermatologists. With Khushbu Goel recent advances, noninvasive tools can largely determine the potential for malignancy, although they cannot supplant histology. Although surgical shave excision with its myriad modifications Department of Dermatology and STD, Maulana Azad Medical College and has been in vogue for decades, the lack of an adequate histological sample, the largely blind Lok Nayak Hospital, New Delhi, Delhi, nature of the procedure, and the possibility of recurrence are persisting issues. Pigment-specific India lasers were initially used in the Q-switched mode, which was based on the thermal relaxation time of the melanocyte (size 7 µm; 1 µsec), which is not the primary target in melanocytic nevus. The cluster of nevus cells (100 µm) probably lends itself to treatment with a millisecond laser rather than a nanosecond laser. Thus, normal mode pigment-specific lasers and pulsed ablative lasers (CO2/erbium [Er]:yttrium aluminum garnet [YAG]) are more suited to treat acquired melanocytic nevi. The complexities of treating this disorder can be overcome by following a structured approach by using lasers that achieve the appropriate depth to treat the three subtypes of nevi: junctional, compound, and dermal. Thus, junctional nevi respond to Q-switched/normal mode pigment lasers, where for the compound and dermal nevi, pulsed ablative laser (CO2/ Er:YAG) may be needed. -

Identification of HRAS Mutations and Absence of GNAQ Or GNA11
Modern Pathology (2013) 26, 1320–1328 1320 & 2013 USCAP, Inc All rights reserved 0893-3952/13 $32.00 Identification of HRAS mutations and absence of GNAQ or GNA11 mutations in deep penetrating nevi Ryan P Bender1, Matthew J McGinniss2, Paula Esmay1, Elsa F Velazquez3,4 and Julie DR Reimann3,4 1Caris Life Sciences, Phoenix, AZ, USA; 2Genoptix Medical Laboratory, Carlsbad, CA, USA; 3Dermatopathology Division, Miraca Life Sciences Research Institute, Newton, MA, USA and 4Department of Dermatology, Tufts Medical Center, Boston, MA, USA HRAS is mutated in B15% of Spitz nevi, and GNAQ or GNA11 is mutated in blue nevi (46–83% and B7% respectively). Epithelioid blue nevi and deep penetrating nevi show features of both blue nevi (intradermal location, pigmentation) and Spitz nevi (epithelioid morphology). Epithelioid blue nevi and deep penetrating nevi can also show overlapping features with melanoma, posing a diagnostic challenge. Although epithelioid blue nevi are considered blue nevic variants, no GNAQ or GNA11 mutations have been reported. Classification of deep penetrating nevi as blue nevic variants has also been proposed, however, no GNAQ or GNA11 mutations have been reported and none have been tested for HRAS mutations. To better characterize these tumors, we performed mutational analysis for GNAQ, GNA11, and HRAS, with blue nevi and Spitz nevi as controls. Within deep penetrating nevi, none demonstrated GNAQ or GNA11 mutations (0/38). However, 6% revealed HRAS mutation (2/32). Twenty percent of epithelioid blue nevi contained a GNAQ mutation (2/10), while none displayed GNA11 or HRAS mutation. Eighty-seven percent of blue nevi contained a GNAQ mutation (26/30), 4% a GNA11 mutation (1/28), and none an HRAS mutation. -

Dermatopathology
Dermatopathology Clay Cockerell • Martin C. Mihm Jr. • Brian J. Hall Cary Chisholm • Chad Jessup • Margaret Merola With contributions from: Jerad M. Gardner • Talley Whang Dermatopathology Clinicopathological Correlations Clay Cockerell Cary Chisholm Department of Dermatology Department of Pathology and Dermatopathology University of Texas Southwestern Medical Center Central Texas Pathology Laboratory Dallas , TX Waco , TX USA USA Martin C. Mihm Jr. Chad Jessup Department of Dermatology Department of Dermatology Brigham and Women’s Hospital Tufts Medical Center Boston , MA Boston , MA USA USA Brian J. Hall Margaret Merola Department of Dermatology Department of Pathology University of Texas Southwestern Medical Center Brigham and Women’s Hospital Dallas , TX Boston , MA USA USA With contributions from: Jerad M. Gardner Talley Whang Department of Pathology and Dermatology Harvard Vanguard Medical Associates University of Arkansas for Medical Sciences Boston, MA Little Rock, AR USA USA ISBN 978-1-4471-5447-1 ISBN 978-1-4471-5448-8 (eBook) DOI 10.1007/978-1-4471-5448-8 Springer London Heidelberg New York Dordrecht Library of Congress Control Number: 2013956345 © Springer-Verlag London 2014 This work is subject to copyright. All rights are reserved by the Publisher, whether the whole or part of the material is concerned, specifi cally the rights of translation, reprinting, reuse of illustrations, recitation, broadcasting, reproduction on microfi lms or in any other physical way, and transmission or information storage and retrieval, electronic adaptation, computer software, or by similar or dissimilar methodology now known or hereafter developed. Exempted from this legal reservation are brief excerpts in connection with reviews or scholarly analysis or material supplied specifi cally for the purpose of being entered and executed on a computer system, for exclusive use by the purchaser of the work. -

Melanomas Are Comprised of Multiple Biologically Distinct Categories
Melanomas are comprised of multiple biologically distinct categories, which differ in cell of origin, age of onset, clinical and histologic presentation, pattern of metastasis, ethnic distribution, causative role of UV radiation, predisposing germ line alterations, mutational processes, and patterns of somatic mutations. Neoplasms are initiated by gain of function mutations in one of several primary oncogenes, typically leading to benign melanocytic nevi with characteristic histologic features. The progression of nevi is restrained by multiple tumor suppressive mechanisms. Secondary genetic alterations override these barriers and promote intermediate or overtly malignant tumors along distinct progression trajectories. The current knowledge about pathogenesis, clinical, histological and genetic features of primary melanocytic neoplasms is reviewed and integrated into a taxonomic framework. THE MOLECULAR PATHOLOGY OF MELANOMA: AN INTEGRATED TAXONOMY OF MELANOCYTIC NEOPLASIA Boris C. Bastian Corresponding Author: Boris C. Bastian, M.D. Ph.D. Gerson & Barbara Bass Bakar Distinguished Professor of Cancer Biology Departments of Dermatology and Pathology University of California, San Francisco UCSF Cardiovascular Research Institute 555 Mission Bay Blvd South Box 3118, Room 252K San Francisco, CA 94158-9001 [email protected] Key words: Genetics Pathogenesis Classification Mutation Nevi Table of Contents Molecular pathogenesis of melanocytic neoplasia .................................................... 1 Classification of melanocytic neoplasms -

A Nevus of OTA with Intraoral Involvement: a Rare Case Report
Shivare P. et al.: Nevus of OTA- a rare entity CASE REPORT A Nevus of OTA with Intraoral Involvement: A Rare Case Report Peeyush Shivhare1, Lata S.2, Monu Yadav3, Naqoosh Haidry4, Shruthi T. Patil5 1,5- Senior lecturer department of oral medicine and radiology, Narsinhbhai patel dental college and hospital, Visnagar, Gujarat. 2- Professor and head of the department, Rungta Correspondence to: College Of Dental Sciences And Research, Bhilai, Chhattisgarh. 3- PG student. Dr. Peeyush Shivhare Senior lecturer department of Department Of Oral Medicine And Radiology, Carrier Dental College And Hospital. oral medicine and radiology, Narsinhbhai patel dental Lucknow. 4- Senior lecturer department of maxillofacial surgery, Narsinhbhai patel college and hospital, Visnagar, Gujarat. dental college and hospital, Visnagar, Gujarat. Contact Us: www.ijohmr.com ABSTRACT Nevus of Ota, which originally was described by Ota and Tanino in 1939. It is characterized as congenital or acquired hamartoma of dermal melanocytes, presents clinically as a blue or gray patch on the face within the distribution of the ophthalmic and maxillary branches of the fifth cranial (trigeminal) nerve. Involvement of the palatal mucosa occurs rarely in nevus of Ota, when it occurs, it usually blends with the oral mucosa and is typically irregular, ill defined and often present as a mottled patch. Nevus of Ota is rare in the Indian subcontinent. So far very less cases of nevus of ota with intraoral involvement have been documented in the English literature. We report a rare case of intraoral nevus of Ota in a 20 year-old female patient. KEYWORDS: Nevus of Ota, Melanoma, Hamartoma, Glaucoma AA aaaasasasss INTRODUCTION The nevus of Ota (nevus fuscoceruleus ophthal- momaxillaris” or oculodermal melanocytosis) is a macular discoloration of the face, found most commonly in the Japanese people.1 Nevus of ota develops when the melanocyte get entrapped in the upper third of the dermis. -

Superficial Melanocytic Pathology Melanocytic Superficial Atypical Melanocytic Proliferations Pathology Superficial Atypical David E
Consultant Consultant Pathology Series Editor ■ David E. Elder, MB, ChB Series Editor ■ David E. Elder, MB, ChB ■ Pathology7 Consultant Pathology 7 MelanocyticSuperficial Pathology 7 Superficial Superficial Melanocytic Pathology Melanocytic Superficial Atypical Melanocytic Proliferations Pathology Superficial Atypical David E. Elder, MB, ChB • Sook Jung Yun, MD, PhD Melanocytic Proliferations Add Expert Analysis of Difficult Cases to Your Practice With Consultant Pathology Superficial Melanocytic Pathology provides expert guidance for resolving the real world problems pathologists face when diagnosing melanomas and other atypical pigmented lesions. It reviews each major category of atypical melanocytic lesions, including the pathology of the superficial categories of melanoma followed by a discussion of the major simulants David E. Elder of melanoma. The book provides an overview of the morphologic description and diagnostic issues for each lesion, followed by 60 detailed, Sook Jung Yun abundantly illustrated case presentations, offering an expert approach to diagnosis for a range of challenging cases. Five hundred high-quality color images support the case presentations. Of special interest is a chapter on “ambiguous” lesions of uncertain significance. The book’s thorough analysis of challenging lesions will aid pathologists in differentiating between benign superficial proliferations and malignant melanocytic tumors. All Consultant Pathology Titles Provide: Elder • Yun ■ ACTUAL consultation cases and expert analysis ■ EXPERT analysis -

Nevus of Ota in Children
PEDIATRIC DERMATOLOGY Series Editor: Camila K. Janniger, MD Nevus of Ota in Children Smeeta Sinha, MD; Philip J. Cohen, MD; Robert A. Schwartz, MD, MPH Nevus of Ota, synonymously termed oculodermal seen most commonly in individuals of Japanese melanosis, is an uncommon dermal melanosis descent, and is less likely to present in individuals most commonly seen at birth in children of of Chinese or Korean descent, though individuals Japanese descent, though it can affect individu- descending from the Indian subcontinent, Africa, als of any age or ethnicity. The disease tends to and Europe also may be affected.7 In early sur- persist and extend locally, becoming increasingly veys of Japanese patients at dermatology clinics, prominent with age, puberty, and postmenopausal the incidence of nevus of Ota was determined to state. Treatment should begin early after diagno- be 0.4% (110/27,500).4 Cowan and Balistocky8 sis using multiple sessions of laser photother- calculated the incidence of oculodermal melano- molysis to avoid darkening and extension of the cytosis in black patients to be 0.016%. A study of lesion. Important associated disorders include 2914 Chinese children in Calgary, Alberta, Canada, ipsilateral glaucoma; intracranial melanocyto- reported an incidence of oculodermal melanocytosis sis; and rarely cutaneous, ocular, or intracranial of 0.034% (1/2914).9 melanoma. Recommendations are discussed for managing nevus of Ota in children. Clinical Manifestation Cutis. 2008;82:25-29. The typical nevus of Ota is a unilateral facial dis- coloration that is macular, speckled, and bluish gray or brown, with edges that blend with bordering skin evus of Ota is a rare disorder characterized (Figure).10 The dermatomal distribution of pigment by melanocytic pigmentation of the sclera characterizes this diagnosis in most cases. -

Blue Nevi and Melanomas Natural Blue BLUE NEVUS Blue Nevus (BN)
KJ Busam, M.D. Paris, 2017 Blue Nevi and Melanomas Natural Blue BLUE NEVUS Blue Nevus (BN) • Spectrum of blue nevi – Common, Sclerosing, Epithelioid, Cellular, Plaque type blue nevi • Differential diagnosis – Melanoma ex BN or simulating BN – BN vs other tumors – Biphenotypic/collision lesions Common Blue Nevus Clinical: - Circumscribed small bluish macule/papule - Preferred sites: Scalp, wrist, foot Pathology: - Predominantly reticular dermal lesion - Pigmented fusiform and dendritic cells - Admixed melanophages - Bland cytology Common Blue Nevus Blue Nevus Sclerosing Blue Nevus Pigm BN Cellular Blue Nevus - 49 yo woman - Buttock nodule CBN Cellular Blue Nevus Thrombi and stromal edema Multinucleated giant melanocytes Cellular Blue Nevus Hemorrhagic cystic (“aneurysmal”) change Amelanotic Cellular Blue Nevus 19 yo man with buttock lesion Atypical CBN Plaque-Type Blue Nevus Plaque-type Blue Nevus Plaque Type Blue Nevus Mucosal Blue Nevus Conjunctival Blue Nevus Nodal Blue Nevus Combined epithelioid BN Blue Nevus • M Tieche 1906; Virchow Arch Pathol Anat “Blaue Naevus” • B Upshaw 1947; Surgery “Extensive Blue Nevus” (plaque-type BN) • A Allen 1949; Cancer “ Cellular Blue Nevus” Blue Nevus – Mutation Analysis Type of Lesion GNAQ GNA11 Number Common BN 6.7% 65% 60 Cellular BN 8.3% 72.2% 36 Amelanotic BN 0% 70% 10 Nevus of Ota 5% 10% 20 Nevus of Ito 16.7% 0% 7 TOTAL 6.5% 55% 139 Van Raamsdonk et al NEJM 2010; 2191-9 Blue Nevus – Mutation Analysis Type of Blue Nevus GNAQ Number Common Blue Nevus 40% 4/10 Cellular Blue Nevus 44% 4/9 Hypomelanotic