Nevus Spilus
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Clinical Features of Benign Tumors of the External Auditory Canal According to Pathology
Central Annals of Otolaryngology and Rhinology Research Article *Corresponding author Jae-Jun Song, Department of Otorhinolaryngology – Head and Neck Surgery, Korea University College of Clinical Features of Benign Medicine, 148 Gurodong-ro, Guro-gu, Seoul, 152-703, South Korea, Tel: 82-2-2626-3191; Fax: 82-2-868-0475; Tumors of the External Auditory Email: Submitted: 31 March 2017 Accepted: 20 April 2017 Canal According to Pathology Published: 21 April 2017 ISSN: 2379-948X Jeong-Rok Kim, HwibinIm, Sung Won Chae, and Jae-Jun Song* Copyright Department of Otorhinolaryngology-Head and Neck Surgery, Korea University College © 2017 Song et al. of Medicine, South Korea OPEN ACCESS Abstract Keywords Background and Objectives: Benign tumors of the external auditory canal (EAC) • External auditory canal are rare among head and neck tumors. The aim of this study was to analyze the clinical • Benign tumor features of patients who underwent surgery for an EAC mass confirmed as a benign • Surgical excision lesion. • Recurrence • Infection Methods: This retrospective study involved 53 patients with external auditory tumors who received surgical treatment at Korea University, Guro Hospital. Medical records and evaluations over a 10-year period were examined for clinical characteristics and pathologic diagnoses. Results: The most common pathologic diagnoses were nevus (40%), osteoma (13%), and cholesteatoma (13%). Among the five pathologic subgroups based on the origin organ of the tumor, the most prevalent pathologic subgroup was the skin lesion (47%), followed by the epithelial lesion (26%), and the bony lesion (13%). No significant differences were found in recurrence rate, recurrence duration, sex, or affected side between pathologic diagnoses. -

CASE REPORT Intradermal Nevus of the External Auditory Canal
Int. Adv. Otol. 2009; 5:(3) 401-403 CASE REPORT Intradermal Nevus of the External Auditory Canal: A Case Report Sedat Ozturkcan, Ali Ekber, Riza Dundar, Filiz Gulustan, Demet Etit, Huseyin Katilmis Department of Otorhinolaryngology and Head and Neck Surgery ‹zmir Atatürk Research and Training Hospital, Ministry of Health, ‹ZM‹R-TURKEY (SO, AE, FG, DE, HK) Department of Otorhinolaryngology and Head and Neck Surgery Etimesgut Military Hospital , ANKARA-TURKEY (RD) Intradermal nevus is the most common skin tumor in humans; however, its occurrence in the external auditory canal (EAC) is uncommon. The clinical manifestations of pigmented nevus of the EAC have been reported to include ear fullness, foreign body sensation, hearing impairment, and otalgia, but some cases were asymptomatic and were found incidentally. The treatment of choice for a symptomatic intradermal nevus in the EAC is complete excision. There has been no recurrence reported in the literature . A pedunculated, papillomatous hair-bearing lesion was detected in the external auditory canal of the patient who was on follow-up for pruritus. Clinical and pathologic features of an intradermal nevus of the external auditory canal are presented, and the literature reviewed. Submitted : 14 October 2008 Revised : 01 July 2009 Accepted : 09 July 2009 Intradermal nevus is the most common skin tumor in left external auditory canal. Otomicroscopic humans; however, its occurrence in the external examination revealed a pedunculated, papillomatous auditory canal (EAC) is uncommon [1-4]. Intradermal hair-bearing lesion in the postero-inferior cartilaginous nevus is considered to be a form of benign cutaneous portion of the external auditory canal (Figure 1). -

Critical Evaluation of the So-Called “Junction Nevus”
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Elsevier - Publisher Connector CRITICAL EVALUATION OF THE SO-CALLED "JUNCTION NEVUS* S. WILLIAM BECKER, MS., M.D. The serious study of pigmented nevi was undertaken by many workers in the closing years of the 19th Century. All recognized that the microscopic picture of nevi differed from anything seen in other organs. The presence of nevus cells in both the epidermis and dermis led to concepts of origin at one or the other site, or at both sites. Dermal Origin: Demieville (1) believed that the nevus cells arose from adven- titial and endothelial cells of blood vessels. Bauer (2) and vonRecklinghausen (3) thought that the origin was from endothelium of lymph vessels rather than of blood vessels. Epidermal Origin: According to Abesser (4), Duranti, in 1871, was the first to suggest an epidermal origin of nevus cells. Kromayer (5) stated that the endo- thelium-like cells originate in the basal portion of the epidermis as "Bläschen- zellen", migrate to the dermis and develop connective tissue and elastic fibers, a change which he called "desmoplasia". Abesser (4) agreed that the cells origi- ated in the epithelium and lost their intercellular bridges, but migrated into the dermis as epithelium-like cells, and remained such. Unna (6) advanced the concept that the epithelial cells changed by losing their intercellular bridges and multiplied in groups, a process which he called "Ab- sonderung", then migrated as groups to the dermis, which he called "Abtrop- fung", thus forming pigmented nevi. -

Acral Compound Nevus SJ Yun S Korea
University of Pennsylvania, Founded by Ben Franklin in 1740 Disclosures Consultant for Myriad Genetics and for SciBase (might try to sell you a book, as well) Multidimensional Pathway Classification of Melanocytic Tumors WHO 4th Edition, 2018 Epidemiologic, Clinical, Histologic and Genomic Aspects of Melanoma David E. Elder, MB ChB, FRCPA University of Pennsylvania, Philadelphia, PA, USA Napa, May, 2018 3rd Edition, 2006 Malignant Melanoma • A malignant tumor of melanocytes • Not all melanomas are the same – variation in: – Epidemiology – risk factors, populations – Cell/Site of origin – Precursors – Clinical morphology – Microscopic morphology – Simulants – Genomic abnormalities Incidence of Melanoma D.M. Parkin et al. CSD/Site-Related Classification • Bastian’s CSD/Site-Related Classification (Taxonomy) of Melanoma – “The guiding principles for distinguishing taxa are genetic alterations that arise early during progression; clinical or histologic features of the primary tumor; characteristics of the host, such as age of onset, ethnicity, and skin type; and the role of environmental factors such as UV radiation.” Bastian 2015 Epithelium associated Site High UV Low UV Glabrous Mucosa Benign Acquired Spitz nevus nevus Atypical Dysplastic Spitz Borderline nevus tumor High Desmopl. Low-CSD Spitzoid Acral Mucosal Malignant CSD melanoma melanoma melanoma melanoma melanoma 105 Point mutations 103 Structural Rearrangements 2018 WHO Classification of Melanoma • Integrates Epidemiologic, Genomic, Clinical and Histopathologic Features • Assists -
A Case of Intradermal Melanocytic Nevus with Ossification (Nevus of Nanta)
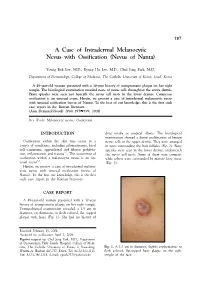
197 A Case of Intradermal Melanocytic Nevus with Ossification (Nevus of Nanta) Young Bok Lee, M.D., Kyung Ho Lee, M.D., Chul Jong Park, M.D. Department of Dermatology, College of Medicine, The Catholic University of Korea, Seoul, Korea A 49-year-old woman presented with a 30-year history of asymptomatic plaque on her right temple. The histological examination revealed nests of nevus cells throughout the entire dermis. Bony spicules were seen just beneath the nevus cell nests in the lower dermis. Cutaneous ossification is an unusual event. Herein, we present a case of intradermal melanocytic nevus with unusual ossification (nevus of Nanta). To the best of our knowledge, this is the first such case report in the Korean literature. (Ann Dermatol (Seoul) 20(4) 197∼199, 2008) Key Words: Melanocytic nevus, Ossification INTRODUCTION drug intake or medical illness. The histological examination showed a dense proliferation of benign Ossification within the skin may occur in a nevus cells in the upper dermis. They were arranged variety of conditions, including pilomatricoma, basal in nests surrounding the hair follicles (Fig. 2). Bony cell carcinoma, appendageal and fibrous prolifera- spicules were seen in the lower dermis, underneath 1,2 tion, inflammation and trauma . The occurrence of the nevus cell nests. Some of them were compact ossification within a melanocytic nevus is an un- while others were surrounded by mature fatty tissue 3-5 usual event . (Fig. 3). Herein, we present a case of intradermal melano- cytic nevus with unusual ossification (nevus of Nanta). To the best our knowledge, this is the first such case report in the Korean literature. -

Nevus Spilus: Is the Presence of Hair Associated with an Increased Risk for Melanoma?
Nevus Spilus: Is the Presence of Hair Associated With an Increased Risk for Melanoma? Robert Milton Gathings, MD; Raveena Reddy, MD; Ashish C. Bhatia, MD; Robert T. Brodell, MD PRACTICE POINTS • Nevus spilus (NS) appears as a café au lait macule studded with darker brown “moles.” • Although melanoma has been described in NS, it is rare. • There is no evidence that hairy NS are predisposed to melanoma. copy not Nevus spilus (NS), also known as speckled len- he term nevus spilus (NS), also known as tiginous nevus, is characterized by background speckled lentiginous nevus, was first used café au lait–like lentiginous melanocytic hyperpla- Tin the 19th century to describe lesions with sia speckled with small, 1- to 3-mm, darker foci.Do background café au lait–like lentiginous melanocytic Nevus spilus occurs in 1.3% to 2.3% of the adult hyperplasia speckled with small, 1- to 3-mm, darker population worldwide. Reports of melanoma aris- foci. The dark spots reflect lentigines; junctional, ing within hypertrichotic NS suggest that hyper- compound, and intradermal nevus cell nests; and trichosis may be a marker for the development of more rarely Spitz and blue nevi. Both macular and melanoma. We present a case of a hypertrichotic papular subtypes have been described.1 This birth- NS without melanoma and also provide a review of mark is quite common, occurring in 1.3% to 2.3% previously reported cases of hypertrichosis in NS. of the adult population worldwide.2 Hypertrichosis We believe that NS has aCUTIS lower risk for malignant has been described in NS.3-9 Two subsequent cases degeneration than congenital melanocytic nevi of malignant melanoma in hairy NS suggested that (CMN) of the same size, and it is unlikely that lesions may be particularly prone to malignant hypertrichosis is a marker for melanoma in NS. -

Short Course 11 Pigmented Lesions of the Skin
Rev Esp Patol 1999; Vol. 32, N~ 3: 447-453 © Prous Science, SA. © Sociedad Espafiola de Anatomfa Patol6gica Short Course 11 © Sociedad Espafiola de Citologia Pigmented lesions of the skin Chairperson F Contreras Spain Ca-chairpersons S McNutt USA and P McKee, USA. Problematic melanocytic nevi melanin pigment is often evident. Frequently, however, the lesion is solely intradermal when it may be confused with a fibrohistiocytic RH. McKee and F.R.C. Path tumor, particularly epithelloid cell fibrous histiocytoma (4). It is typi- cally composed of epitheliold nevus cells with abundant eosinophilic Brigham and Women’s Hospital, Harvard Medical School, Boston, cytoplasm and large, round, to oval vesicular nuclei containing pro- USA. minent eosinophilic nucleoli. Intranuclear cytoplasmic pseudoinclu- sions are common and mitotic figures are occasionally present. The nevus cells which are embedded in a dense, sclerotic connective tis- Whether the diagnosis of any particular nevus is problematic or not sue stroma, usually show maturation with depth. Less frequently the nevus is composed solely of spindle cells which may result in confu- depends upon a variety of factors, including the experience and enthusiasm of the pathologist, the nature of the specimen (shave vs. sion with atrophic fibrous histiocytoma. Desmoplastic nevus can be distinguished from epithelloid fibrous histiocytoma by its paucicellu- punch vs. excisional), the quality of the sections (and their staining), larity, absence of even a focal storiform growth pattern and SiQO pro- the hour of the day or day of the week in addition to the problems relating to the ever-increasing range of histological variants that we tein/HMB 45 expression. -

Oral Pathology
Oral Pathology Palatal blue nevus in a child Catherine M. Flaitz DDS, MS Georgeanne McCandless DDS Dr. Flaitz is professor, Oral and Maxillofacial Pathology and Pediatric Dentistry, Department of Stomatology, University of Texas at Houston Health Science Center Dental Branch; Dr. McCandless has a private practice in The Woodlands, TX. Correspond with Dr. Flaitz at [email protected] Abstract The intraoral blue nevus occurs infrequently in children. This by the labial mucosa (1). Intraoral lesions have a predilection case report describes the clinical features of an acquired blue ne- for females in the third and fourth decades, in contrast to cu- vus in a 7 year-old girl that involved the palatal mucosa. A taneous lesions that normally develop in children. In large differential diagnosis and justification for surgical excision of this biopsy series, only 2% of the oral blue nevi are diagnosed in oral lesion are discussed. (Pediatr Dent 23:354-355, 2001) children and adolescents (1). Similar to their cutaneous coun- terpart, most oral lesions are acquired; however, there are ith the exception of vascular entities, neoplastic isolated reports of congenital examples. lesions with a blue discoloration are an unusual find Clinically, most lesions present as a solitary blue, gray or Wing in children. Although the blue nevus is a blue-black macule or slightly raised nodule that measures less relatively common finding of the skin in the pediatric popula- than 6 mm in size. The margins are often regular but indis- tion, only a few intraoral examples are documented in the tinct and the surface is smooth. -

Optimal Management of Common Acquired Melanocytic Nevi (Moles): Current Perspectives
Clinical, Cosmetic and Investigational Dermatology Dovepress open access to scientific and medical research Open Access Full Text Article REVIEW Optimal management of common acquired melanocytic nevi (moles): current perspectives Kabir Sardana Abstract: Although common acquired melanocytic nevi are largely benign, they are probably Payal Chakravarty one of the most common indications for cosmetic surgery encountered by dermatologists. With Khushbu Goel recent advances, noninvasive tools can largely determine the potential for malignancy, although they cannot supplant histology. Although surgical shave excision with its myriad modifications Department of Dermatology and STD, Maulana Azad Medical College and has been in vogue for decades, the lack of an adequate histological sample, the largely blind Lok Nayak Hospital, New Delhi, Delhi, nature of the procedure, and the possibility of recurrence are persisting issues. Pigment-specific India lasers were initially used in the Q-switched mode, which was based on the thermal relaxation time of the melanocyte (size 7 µm; 1 µsec), which is not the primary target in melanocytic nevus. The cluster of nevus cells (100 µm) probably lends itself to treatment with a millisecond laser rather than a nanosecond laser. Thus, normal mode pigment-specific lasers and pulsed ablative lasers (CO2/erbium [Er]:yttrium aluminum garnet [YAG]) are more suited to treat acquired melanocytic nevi. The complexities of treating this disorder can be overcome by following a structured approach by using lasers that achieve the appropriate depth to treat the three subtypes of nevi: junctional, compound, and dermal. Thus, junctional nevi respond to Q-switched/normal mode pigment lasers, where for the compound and dermal nevi, pulsed ablative laser (CO2/ Er:YAG) may be needed. -

Identification of HRAS Mutations and Absence of GNAQ Or GNA11
Modern Pathology (2013) 26, 1320–1328 1320 & 2013 USCAP, Inc All rights reserved 0893-3952/13 $32.00 Identification of HRAS mutations and absence of GNAQ or GNA11 mutations in deep penetrating nevi Ryan P Bender1, Matthew J McGinniss2, Paula Esmay1, Elsa F Velazquez3,4 and Julie DR Reimann3,4 1Caris Life Sciences, Phoenix, AZ, USA; 2Genoptix Medical Laboratory, Carlsbad, CA, USA; 3Dermatopathology Division, Miraca Life Sciences Research Institute, Newton, MA, USA and 4Department of Dermatology, Tufts Medical Center, Boston, MA, USA HRAS is mutated in B15% of Spitz nevi, and GNAQ or GNA11 is mutated in blue nevi (46–83% and B7% respectively). Epithelioid blue nevi and deep penetrating nevi show features of both blue nevi (intradermal location, pigmentation) and Spitz nevi (epithelioid morphology). Epithelioid blue nevi and deep penetrating nevi can also show overlapping features with melanoma, posing a diagnostic challenge. Although epithelioid blue nevi are considered blue nevic variants, no GNAQ or GNA11 mutations have been reported. Classification of deep penetrating nevi as blue nevic variants has also been proposed, however, no GNAQ or GNA11 mutations have been reported and none have been tested for HRAS mutations. To better characterize these tumors, we performed mutational analysis for GNAQ, GNA11, and HRAS, with blue nevi and Spitz nevi as controls. Within deep penetrating nevi, none demonstrated GNAQ or GNA11 mutations (0/38). However, 6% revealed HRAS mutation (2/32). Twenty percent of epithelioid blue nevi contained a GNAQ mutation (2/10), while none displayed GNA11 or HRAS mutation. Eighty-seven percent of blue nevi contained a GNAQ mutation (26/30), 4% a GNA11 mutation (1/28), and none an HRAS mutation. -

Case Report of Giant Congenital Melanocytic Nevus
PEDIATRIC DERMATOLOGY Series Editor: Camila K. Janniger, MD Bathing Trunks Nevus: Case Report of Giant Congenital Melanocytic Nevus Ronald Russ, DO; Lisa Light, MS-IV Bathing trunks nevi, a subtype of giant congeni- 34 years. All maternal and prenatal history was unre- tal melanocytic nevi (CMN), are skin tumors that markable. Upon initial physical examination as a new- present by 2 years of age and occur in a low born (1 hour following delivery), the infant had a large percentage of all births. We report a case of (≥5% body surface area), circumferentially pigmented bathing trunks nevus that was initially suspected area from the umbilicus to mid thigh bilaterally to be melanoma, and describe the history, patho- (Figure 1). Interposed darkened lesions were pres- physiology, and treatment options for CMN. We ent, with 3 distinct, raised, lipomatous-type nodules also discuss the risk for neurocutaneous melano- (2 cm, 1.3 cm, and 3 cm in diameter from left to right) sis (NCM), which is a rare syndrome in patients over the lower lumbar spine (Figure 2). There were no with giant CMN. signs of jaundice, hemolysis, meningomyelocele, or Cutis. 2009;83:69-72. abnormal hair growth. The rest of the physical exami- nation was unremarkable, including cardiovascular, pulmonary, and abdominal systems, and genitourinary athing trunks nevus is a specific subtype of functioning was normal. Cord blood testing revealed giant congenital melanocytic nevus (CMN) A Rh-positive blood type, and a direct Coombs test B with spread resembling bathing trunks. This was negative for antibodies. Complete blood cell rare variant is clinically significant because of the count was within reference range, with the excep- increased risk for progression to melanoma and its tion of a low platelet count of 2343103/µL (reference association with neurocutaneous melanosis (NCM).1 range, 250–4503103/µL). -

Lumps & Bumps: Approach to Common Dermatologic Neoplasms
Case-Based Approach to Common Dermatologic Neoplasms Patrick Retterbush, MD, FAAD Mohs Surgery & Dermatologic Oncology Associate Member of the American College of Mohs Surgery Private Practice: Lockman Dermatology January 27th 2018 Disclosure of Relevant Financial Relationships • I do not have any relevant financial relationships, commercial interests, and/or conflicts of interest regarding the content of this presentation. Goals/Objectives • Recognize common benign growths • Recognize common malignant growths • Useful clues & examination for evaluating melanocytic nevi and when to be concerned for melanoma/atypical moles • How to perform a basic skin biopsy and which method/type to choose • Basic treatment/when to refer Key Questions & Physical Examination Findings for a Growth History Physical Examination • How long has the lesion been • Describing a growth present? – flat or raised? • flat – macule (<1cm) or patch (>1cm) – years, months, weeks • raised – papule (<1cm) or plaque (>1cm) – nodule if deep (majority of lesion in • Has it changed? dermis/SQ) – Size – secondary descriptive features • scaly (hyperkeratosis, retention of strateum – Shape corneum) – Color • crusty (dried serum, blood, or pus on surface) • eroded or ulcerated (partial vs. full thickness – Symptoms – pain, bleeding, itch? epidermal loss) – Over what time frame? • color (skin colored, red, pigmented, pearly) • feel (hard or soft, mobile or fixed) • PMH: • size: i.e. 6 x 4mm – prior skin cancers • Look at the rest of the skin/region of skin • SCC/BCCs vs. melanoma