Meeting Report
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Part Ii Metro Manila and Its 200Km Radius Sphere
PART II METRO MANILA AND ITS 200KM RADIUS SPHERE CHAPTER 7 GENERAL PROFILE OF THE STUDY AREA CHAPTER 7 GENERAL PROFILE OF THE STUDY AREA 7.1 PHYSICAL PROFILE The area defined by a sphere of 200 km radius from Metro Manila is bordered on the northern part by portions of Region I and II, and for its greater part, by Region III. Region III, also known as the reconfigured Central Luzon Region due to the inclusion of the province of Aurora, has the largest contiguous lowland area in the country. Its total land area of 1.8 million hectares is 6.1 percent of the total land area in the country. Of all the regions in the country, it is closest to Metro Manila. The southern part of the sphere is bound by the provinces of Cavite, Laguna, Batangas, Rizal, and Quezon, all of which comprise Region IV-A, also known as CALABARZON. 7.1.1 Geomorphological Units The prevailing landforms in Central Luzon can be described as a large basin surrounded by mountain ranges on three sides. On its northern boundary, the Caraballo and Sierra Madre mountain ranges separate it from the provinces of Pangasinan and Nueva Vizcaya. In the eastern section, the Sierra Madre mountain range traverses the length of Aurora, Nueva Ecija and Bulacan. The Zambales mountains separates the central plains from the urban areas of Zambales at the western side. The region’s major drainage networks discharge to Lingayen Gulf in the northwest, Manila Bay in the south, the Pacific Ocean in the east, and the China Sea in the west. -
1623400766-2020-Sec17a.Pdf
COVER SHEET 2 0 5 7 3 SEC Registration Number M E T R O P O L I T A N B A N K & T R U S T C O M P A N Y (Company’s Full Name) M e t r o b a n k P l a z a , S e n . G i l P u y a t A v e n u e , U r d a n e t a V i l l a g e , M a k a t i C i t y , M e t r o M a n i l a (Business Address: No. Street City/Town/Province) RENATO K. DE BORJA, JR. 8898-8805 (Contact Person) (Company Telephone Number) 1 2 3 1 1 7 - A 0 4 2 8 Month Day (Form Type) Month Day (Fiscal Year) (Annual Meeting) NONE (Secondary License Type, If Applicable) Corporation Finance Department Dept. Requiring this Doc. Amended Articles Number/Section Total Amount of Borrowings 2,999 as of 12-31-2020 Total No. of Stockholders Domestic Foreign To be accomplished by SEC Personnel concerned File Number LCU Document ID Cashier S T A M P S Remarks: Please use BLACK ink for scanning purposes. 2 SEC Number 20573 File Number______ METROPOLITAN BANK & TRUST COMPANY (Company’s Full Name) Metrobank Plaza, Sen. Gil Puyat Avenue, Urdaneta Village, Makati City, Metro Manila (Company’s Address) 8898-8805 (Telephone Number) December 31 (Fiscal year ending) FORM 17-A (ANNUAL REPORT) (Form Type) (Amendment Designation, if applicable) December 31, 2020 (Period Ended Date) None (Secondary License Type and File Number) 3 SECURITIES AND EXCHANGE COMMISSION SEC FORM 17-A ANNUAL REPORT PURSUANT TO SECTION 17 OF THE SECURITIES REGULATION CODE AND SECTION 141 OF CORPORATION CODE OF THE PHILIPPINES 1. -

Study on Medium Capacity Transit System Project in Metro Manila, the Republic of the Philippines
Study on Economic Partnership Projects in Developing Countries in FY2014 Study on Medium Capacity Transit System Project in Metro Manila, The Republic of The Philippines Final Report February 2015 Prepared for: Ministry of Economy, Trade and Industry Ernst & Young ShinNihon LLC Japan External Trade Organization Prepared by: TOSTEMS, Inc. Oriental Consultants Global Co., Ltd. Mitsubishi Heavy Industries, Ltd. Japan Transportation Planning Association Reproduction Prohibited Preface This report shows the result of “Study on Economic Partnership Projects in Developing Countries in FY2014” prepared by the study group of TOSTEMS, Inc., Oriental Consultants Global Co., Ltd., Mitsubishi Heavy Industries, Ltd. and Japan Transportation Planning Association for Ministry of Economy, Trade and Industry. This study “Study on Medium Capacity Transit System Project in Metro Manila, The Republic of The Philippines” was conducted to examine the feasibility of the project which construct the medium capacity transit system to approximately 18km route from Sta. Mesa area through Mandaluyong City, Ortigas CBD and reach to Taytay City with project cost of 150 billion Yen. The project aim to reduce traffic congestion, strengthen the east-west axis by installing track-guided transport system and form the railway network with connecting existing and planning lines. We hope this study will contribute to the project implementation, and will become helpful for the relevant parties. February 2015 TOSTEMS, Inc. Oriental Consultants Global Co., Ltd. Mitsubishi Heavy -
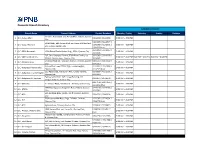
Domestic Branch Directory BANKING SCHEDULE
Domestic Branch Directory BANKING SCHEDULE Branch Name Present Address Contact Numbers Monday - Friday Saturday Sunday Holidays cor Gen. Araneta St. and Aurora Blvd., Cubao, Quezon 1 Q.C.-Cubao Main 911-2916 / 912-1938 9:00 AM – 4:00 PM City 912-3070 / 912-2577 / SRMC Bldg., 901 Aurora Blvd. cor Harvard & Stanford 2 Q.C.-Cubao-Harvard 913-1068 / 912-2571 / 9:00 AM – 4:00 PM Sts., Cubao, Quezon City 913-4503 (fax) 332-3014 / 332-3067 / 3 Q.C.-EDSA Roosevelt 1024 Global Trade Center Bldg., EDSA, Quezon City 9:00 AM – 4:00 PM 332-4446 G/F, One Cyberpod Centris, EDSA Eton Centris, cor. 332-5368 / 332-6258 / 4 Q.C.-EDSA-Eton Centris 9:00 AM – 4:00 PM 9:00 AM – 4:00 PM 9:00 AM – 4:00 PM EDSA & Quezon Ave., Quezon City 332-6665 Elliptical Road cor. Kalayaan Avenue, Diliman, Quezon 920-3353 / 924-2660 / 5 Q.C.-Elliptical Road 9:00 AM – 4:00 PM City 924-2663 Aurora Blvd., near PSBA, Brgy. Loyola Heights, 421-2331 / 421-2330 / 6 Q.C.-Katipunan-Aurora Blvd. 9:00 AM – 4:00 PM Quezon City 421-2329 (fax) 335 Agcor Bldg., Katipunan Ave., Loyola Heights, 929-8814 / 433-2021 / 7 Q.C.-Katipunan-Loyola Heights 9:00 AM – 4:00 PM Quezon City 433-2022 February 07, 2014 : G/F, Linear Building, 142 8 Q.C.-Katipunan-St. Ignatius 912-8077 / 912-8078 9:00 AM – 4:00 PM Katipunan Road, Quezon City 920-7158 / 920-7165 / 9 Q.C.-Matalino 21 Tempus Bldg., Matalino St., Diliman, Quezon City 9:00 AM – 4:00 PM 924-8919 (fax) MWSS Compound, Katipunan Road, Balara, Quezon 927-5443 / 922-3765 / 10 Q.C.-MWSS 9:00 AM – 4:00 PM City 922-3764 SRA Building, Brgy. -

Battling Congestion in Manila: the Edsa Problem
Transport and Communications Bulletin for Asia and the Pacific No. 82, 2013 BATTLING CONGESTION IN MANILA: THE EDSA PROBLEM Yves Boquet ABSTRACT The urban density of Manila, the capital of the Philippines, is one the highest of the world and the rate of motorization far exceeds the street capacity to handle traffic. The setting of the city between Manila Bay to the West and Laguna de Bay to the South limits the opportunities to spread traffic from the south on many axes of circulation. Built in the 1940’s, the circumferential highway EDSA, named after historian Epifanio de los Santos, seems permanently clogged by traffic, even if the newer C-5 beltway tries to provide some relief. Among the causes of EDSA perennial difficulties, one of the major factors is the concentration of major shopping malls and business districts alongside its course. A second major problem is the high number of bus terminals, particularly in the Cubao area, which provide interregional service from the capital area but add to the volume of traffic. While authorities have banned jeepneys and trisikel from using most of EDSA, this has meant that there is a concentration of these vehicles on side streets, blocking the smooth exit of cars. The current paper explores some of the policy options which may be considered to tackle congestion on EDSA . INTRODUCTION Manila1 is one of the Asian megacities suffering from the many ills of excessive street traffic. In the last three decades, these cities have experienced an extraordinary increase in the number of vehicles plying their streets, while at the same time they have sprawled into adjacent areas forming vast megalopolises, with their skyline pushed upwards with the construction of many high-rises. -

Chapter 16 Bridge Replacement Outline Design of Selected Bridges
CHAPTER 16 BRIDGE REPLACEMENT OUTLINE DESIGN OF SELECTED BRIDGES 16.1 Design Criteria and Conditions for Bridge Replacement 16.1.1 Design Criteria and Conditions for Bridge Replacement The following items show design criteria and conditions utilized for outline design of new bridges. (1) Design Standards utilized for Outline Design of New Bridges The Design standards utilized for outline design of new bridges shall be given as follows: Table 16.1.1-1 Design Standards Utilized for Outline Design of New Bridges Item Design Condition Specification 1) General Design Load Combination LV2 Seismic Design: Extreme Event I LRFD (2012) Seismic Design Design Spectrum (1,000year) JICA Study Team Response Spectrum Analysis JICA Study Team 2) Superstructure 3350 mm (Pack and Guadalupe) Design Lane Width DPWH, AASHTO 3000 mm (Lambingan) Dead Load LRFD (2012) Live Load HL-93 and Lane Loads LRFD (2012) 3) Substructure Seismic Earth Pressure LRFD(2012) Column Section Design R-factor method LRFD(2012) 4) Foundation Pile Foundation Analysis JICA Study Team (JRA) Soil Type JICA Study Team (JRA) Liquefaction design JICA Study Team (JRA) Pile Bearing L1: FS=2, L2: FS=1 JICA Study Team (JRA) Pile Section Design M-N chart (=1.0) LRFD(2012) 16-1 (2) Load Factors and Combination The outline design calculation shall be carried out based on LRFD methodology given in AASHTO LRFD 2012 as follows: 1) Loads Table 16.1.1-2 Permanent and Transient Loads Permanent Loads DD = Down drag DC = Dead load of structural components and nonstructural attachment DW = Dead load of -

Private Schools
DEPED - NATIONAL CAPITAL REGION LIST OF PRIVATE PRESCHOOL & ELEMENTARY SCHOOLS AS OF MAY, 2012 NURSERY / KINDERGATEN COURSE ELEMENTARY COURSE SCHOOL E- E-SCHOOL No. DIVISION SCHOOL ADDRESS STATUS-P NUMBER-P SERIES-P DATE-P REMARK-P GRADE E-STATUS E-SERIES E-DATE REMARK YEAR-P NUMBER YEAR 89 P. Cruz St., Mandaluyong City (formerly at 458 Malaya St., Mandaluyong ANGELS INSTITUTE OF LEARNING, INC. Recognized P-005 2006 3/3/06 2005-2006 - Gr. 1-6 Recognized E-010 2008 05/26/08 2007-2008 - Plainview, Mandaluyong City) Mandaluyong CASA ROMANA PRE-SCHOOL LEARNING CENTER #33 Bulusan Street, Brgy. Mauway, Mandaluyong City Permit P-361 2011 12/9/11 2011-2012 - - - Mandaluyong CHILDREN'S PRE-SCHOOL HOUSE 654 Boni Avenue, Mandaluyong City Recognized - - - 285 Connecticut cor Misouti Sts., Greenhills East, Mandaluyong CHIRLDREN'S TALENT EDUCATIONAL CENTER Recognized - - - Mandaluyong City #429 Shaw Boulevard corner A. Mabini Street, Mandaluyong Mandaluyong CLAYTON LEARNING CENTER PHILIPPINES INC. Permit P-056 2012 3/1/12 2011-2012 - City Mandaluyong CURUM CHRISTIAN SCHOOL, INC. 186 San Rafael St., Plainview, Mandaluyong City Recognized P-033 2011 5/25/11 2010-2011 - - - Mandaluyong DON BOSCO TECHNICAL COLLEGE 733 Gen. Kalentong, Mandaluyong City Recognized P-043 2008 9/29/08 2008-2009 - Gr. 1-6 Recognized E-018 2006 06/22/06 2006-2007 - EXPLORATIONS: A DEVELOPMENTAL INTERACTION Mandaluyong 928 Luna Mencias St., Addition Hills, Mandaluyong City Permit P-302 2011 9/26/11 2011-2012 - - - EDUCATIONAL CENTER, INC. Mandaluyong GODD SHEPHERD CHRISTIAN SCHOOL 71 I. Lopez St., Mandaluyong City Recognized - Gr. 1-6 Recognized - Mandaluyong GROWING SEED CHILD DEVELOPMENT CENTER INC. -

Welcome Pack Urban WASH.Pdf
A Red Cross Red Crescent Movement Technical Working Group Meeting Manila, Philippines May 30 to June 1, 2018 Organized and Hosted by RCRC Urban WASH Technical Working Group Meeting Manila 30th May – 1st June, 2018 The Philippine Red Cross and the IFRC is pleased to welcome you to Philippines for the 2018 Urban WASH Technical Working Group Meeting which will be held in Manila from 30th May to 1st June 2018. We would like to share some useful information to ensure that your stay is a comfortable and memorable one. General Information Dates and Venue The Urban WASH technical working group will be held in Manila from 30th May to 1st June at Philippine Red Cross (PRC) Tower, Mandaluyong City, Metro Manila Philippines. We will have the meeting held in PRC Multipurpose Hall. Accommodation The participants will be billeted in Legend Villas Hotel, Mandaluyong City. The PRC has facilitated the booking reservation of the participants in the Urban WASH TWG and in charge to pay for the accommodation. The Legend Villa Hotel is close to the PRC Tower and can be reached within 20 minutes. PRC has organized the shuttle from Legend Villa Hotel to PRC tower and vice versa. The Legend Villas Hotel: Pioneer Street, Mandaluyong City, 1550 Metro Manila, Philippines. https://www.legendvillas.com.ph/ Transportation and Arrival in Manila The PRC has organized a vehicle to fetch and convey the participants from the airport to the Legend Villas Hotel. There are four airport terminals in Manila. If you want to proceed directly from airport to the Hotel, you may use the airport metered taxi or use Grab as this is widely used in the Philippines. -

Disaster Risk Reduction Through Resilient Public Infrastructure by Dpwh
Republic of the Philippines DEPARTMENT OF PUBLIC WORKS AND HIGHWAYS DISASTER RISK REDUCTION THROUGH RESILIENT PUBLIC INFRASTRUCTURE BY DPWH “Building an integrated, efficient and climate adaptive infrastructure towards a livable, sustainable and resilient communities.” MARIA CATALINA E. CABRAL, PhD. Undersecretary for Planning and Public Private Partnership Service, Department of Public Works and Highways and 2017 National President – Philippine Institute of Civil Engineers (PICE) Building a Disaster Resilient Philippines Manila Polo Club, Makati City 25-26 April 2017 A NATURAL DISASTER CAN PARALYZE TRANSPORTATION SYSTEMS LOSS OF FUNCTION OF A TRANSPORTATION SYSTEM CAN PARALYZE LOCAL, REGIONAL, AND INTERNATIONAL EMERGENCY RESPONSE FEATURES THAT AFFECT RESILIENCY ▪Different modes of trans-portation are interconnected ▪They interact with each other and other elements of a community’s built environ-ment; hence, the name, Lifeline systems”. ❑ HIGHWAY SYSTEMS Flooding from tropical storms, and typhoons, Landslides (rock falls, spreads, slides, flows) Earthquakes Livable, Sustainable and Resilient Communities (Disaster Risk Reduction and Climate Change Adaptation Program) What is being been done so far BY DPWH? 5 2017-2022 Philippine Development Plan Key Principles of Spatial Development Integration of leading and lagging areas and urban-rural linkages through transportation networks Improvement of access to social services Identification of locations of major infrastructure to maximize their benefits Improvement of local, national, and international connectivity Promotion of sustainable development and Source: pdp.neda.gov.ph resiliency 2017-2022 Philippine Development Plan Strategic Framework (Targets) Growth in gross domestic product (GDP) is expected to strengthen at 7 to 8 percent. Growth will be more inclusive as manifested by a lower poverty from 21.6 percent in 2015 to 14.0 percent in 2022. -

List of Approved Sending Organization (The Philippines)
LIST OF APPROVED SENDING ORGANIZATION (THE PHILIPPINES) ※フィリピンの認定送出機関については,フィリピン海外雇用庁(POEA)が運営する以下のURLにて,送出機関の名称を入力することによ Date of receipt: り,同機関の連絡先やライセンスの取得状況等を検索できます。 http://www.poea.gov.ph/cgi-bin/agSearch.asp 22/Jan/2021 Person in charge of Training Contact Point in Japan OTIT List No. Name of Organization Address URL No. Name of Person in Name TEL Email Address TEL Email Charge akananmanpower.corp@ A. KANAN MANPOWER 6/F Metro Lifestyle Complex, F. Torres St., www.akananmanpower. yahoo.com / 1 2 HISANO HORI (053) 482-8451 N/A N/A N/A N/A CORPORATION cor. Jacinto St., Davao City com [email protected] om A.C. SICAT INTERNATIONAL Blk. 5 Lot 9, Villa Lourdes Subd. Brgy. San +63917-1882- WILLABETH C. [email protected] 2 306 N/A ARTURO C. SICAT [email protected] 1-4 Hachiman-cho Miyazaki-ken 080-3229-0555 MANPOWER SERVICES Isidro Bacolor Pampanga 711 TABATA p Unit UG 01 North Podium, Pioneer 8584-8215 / ABBA PERSONNEL SERVICES Corporate Center, Pioneer Highlands Saitama Ken Tokorozawa City [email protected] 3 155 www.abba.ph JENEVIEVE P. ORA 8554-0556 / [email protected] Lalaine Kendo 042-941-4152 INC. Condominium, Pioneer St. Mandaluyong Matsuba Cho 20-23 .jp 8234-5833 City ABD OVERSEAS MANPOWER 23 10 Marconi St. corner Morse St. Brgy. www.abdrecruitment.co ANANIAS B. 843-4757 / 0917- 4 8 [email protected] N/A N/A N/A N/A CORPORATION San Isidro, Makati City m DEVULGADO 529-9569 ACHIEVE UNIVERSAL 2nd & 3rd Floor #302 J.P. Rizal St., Project MA. LOURDES N. 8441-8972 / achieve.universal@gmail 5 5 INTERNATIONAL RECRUITMENT N/A N/A N/A N/A N/A 4, Quezon City MERIA 0917-582-2873 .com SERVICES, INC. -

No. Company Star
Fair Trade Enforcement Bureau-DTI Business Licensing and Accreditation Division LIST OF ACCREDITED SERVICE AND REPAIR SHOPS As of September 30, 2020 Star- Expiry No. Company Classific Address City Contact Person Tel. No. E-mail Category Date ation 1 08 Auto Services 1 Star 4 Boni Serrano cor. William Shaw Caloocan City Edson B. Cachuela - Owner (02)8330 6907 None Automotive (Including 31-Dec-20 Street, Caloocan City Aircon Servicing) 2 1 Stop Battery Shop, Inc. 1 Star 214 Gen. Luis Street, Novaliches, Quezon City Herminio DC. Castillo - (02)936 2262; onestopbattery201 Automotive (Excluding 31-Dec-20 Quezon City President/General Manager (02)419 2859 [email protected] Aircon Servicing) 3 1-29 Car Aircon Service Center 1 Star Blk 1 Lot 1, Sheryll Mirra Street, Parañaque City Ma. Luz M. Reyes - Proprietress (02)8821 1202 maluzreyes129@g Automotive (Including 31-Dec-20 Multinational Village, Parañaque City mail.com Aircon Servicing) 4 1st Corinthean's Appliance Services 1 Star 515-B Quintas Street, CAA BF Int'l. Las Piñas City Felvicenso L. Arguelles - Owner (02)463 0229 vinzarguelles@yah Ref and Airconditioning 31-Dec-20 Village, Las Piñas City oo.com (Type A) 5 2 + 1 Electronics Repair Shop 1 Star Unit 1 MOQ Building, Escoda Street, Parañaque City Emilia L. Manalang - Owner (02)8809 4517 Electronics 31-Dec-20 Phase 1 BF Homes, Parañaque City 6 2539 Cycle Parts Enterprises 1 Star 2539 M. Roxas St., Sta. Ana, Manila Manila Rober C. Quides - Owner (02)7954 4704 Automotive 31-Dec-20 (Motorcycle/Small Engine Servicing) 7 5 Jay Machine Shop 1 Star 2125 G. -

An Assessment of the Absorptive Capacity of Agencies Involved in the Public Works Sector Rosario G
Philippine Institute for Development Studies An Assessment of the Absorptive Capacity of Agencies Involved in the Public Works Sector Rosario G. Manasan and Ruben G. Mercado DISCUSSION PAPER SERIES NO. 2001-17 The PIDS Discussion Paper Series constitutes studies that are preliminary and subject to further revisions. They are be- ing circulated in a limited number of cop- ies only for purposes of soliciting com- ments and suggestions for further refine- ments. The studies under the Series are unedited and unreviewed. The views and opinions expressed are those of the author(s) and do not neces- sarily reflect those of the Institute. Not for quotation without permission from the author(s) and the Institute. August 2001 For comments, suggestions or further inquiries please contact: The Research Information Staff, Philippine Institute for Development Studies 3rd Floor, NEDA sa Makati Building, 106 Amorsolo Street, Legaspi Village, Makati City, Philippines Tel Nos: 8924059 and 8935705; Fax No: 8939589; E-mail: [email protected] Or visit our website at http://www.pids.gov.ph AN ASSESSMENT OF THE ABSORPTIVE CAPACITY OF AGENCIES INVOLVED IN THE PUBLIC WORKS SECTOR* FINAL REPORT Rosario G. Manasan Ruben G. Mercado *This study was jointly undertaken through PIDS Project entitled “An Assessment of the Institutional Capacity and Absorptive Capacity of Agencies Involved in the Public Works Sector” funded by the Japan Bank for Institutional Cooperation (JBIC). Table of Contents Page ABSTRACT EXECUTIVE SUMMARY i-vii 1. INTRODUCTION 1 1.1 Macroeconomic Context 1 1.2 Objectives 5 2. PUBLIC WORKS AND HIGHWAYS SECTOR PERFORMANCE 6 AND CHALLENGES 2.1 Roads 6 2.2 Bridges 8 2.3 Ports 8 2.4 Water Supply 8 2.5 Flood Control 8 3.