A Randomised Study of Dabigatran in Elective Percutaneous Coronary
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Dabigatran, Rivaroxaban, and Warfarin in the Oldest Adults With
CLINICAL INVESTIGATION Dabigatran, Rivaroxaban, and Warfarin in the Oldest Adults with Atrial Fibrillation in Taiwan Chao-Lun Lai, MD, PhD,*†‡§ Ho-Min Chen, MS,† Min-Tsun Liao, MD,* and Ting-Tse Lin, MD* mortality and cardiovascular mortality than those who OBJECTIVES: To compare the effectiveness and safety of used warfarin. Reduced-dose dabigatran was also associ- reduced-dose dabigatran, reduced-dose rivaroxaban, and warfa- ated with lower risk of intracranial hemorrhage than war- rin in individuals aged 85 and older with atrial fibrillation (AF). farin. J Am AmGeriatr GeriatrSoc Soc66:1567–1574, 2018. 2018. DESIGN: Retrospective cohort study. SETTING: Taiwan National Health Insurance claims database, 20112015. Key words: dabigatran; rivaroxaban; warfarin; effec- PARTICIPANTS: Individuals with AF aged 85 and older tiveness; safety; octogenarian (mean 88.6) with incident use of oral anticoagulants between June 1, 2012 and May 31, 2015 (N54,722; dabi- gatran 110 mg, n51,489; rivaroxaban 15 mg/10 mg, n51,736; warfarin, n51,497). MEASUREMENTS: Clinical outcomes included all-cause death, cardiovascular death, ischemic stroke, acute myocardial he risk of ischemic stroke is 5 times as high in individ- infarction, arterial embolism or thrombosis, intracranial hem- T uals with atrial fibrillation (AF) than in those with- orrhage, and gastrointestinal hemorrhage needing transfusion. out.1 Warfarin, the classic vitamin K antagonist, can reduce 2 Propensity score–matched analysis was performed, and the the risk of ischemic stroke by approximately 60%, but the marginal proportional hazards model was used to estimate the narrow therapeutic window and risk of bleeding complica- relative risk of various clinical outcomes in a matched tions associated with warfarin therapy have led to its being 1 dabigatran-warfarin cohort (n51,180 in each group) and a underused. -

DOACS COMPARISON and Faqs
NOACS/DOACS*: PRACTICAL ISSUES AND FREQUENTLY-ASKED QUESTIONS OBJECTIVES: • To summarize characteristics of the direct oral anticoagulants (DOACs) currently available in Canada. • To address common practical issues related to DOAC use. • To address frequently asked questions regarding DOACs. BACKGROUND: The DOACs, which consist of apixaban, dabigatran, edoxaban, and rivaroxaban are used for the prevention and treatment of venous thromboembolism (VTE) and for stroke prevention in atrial fibrillation (AF). Practical advantages of DOACs over warfarin include fixed once- or twice-daily oral dosing without the need for coagulation test monitoring, relatively fewer known drug interactions and no known food interactions. Like warfarin, DOACs increase the risk for bleeding and should be administered under close clinical monitoring. Practical issues regarding the everyday use of DOACs will be addressed in this guide. PRACTICAL AND LIFESTYLE ISSUES: Can DOACs be taken with meals? Rivaroxaban should be taken with meals to enhance absorption; the tablet can be crushed and taken with soft foods such as applesauce. Apixaban, dabigatran, edoxaban can be taken with or without meals. However, taking dabigatran with meals can reduce dyspepsia. Dabigatran capsules should not be opened, broken or chewed before swallowing. Are there any foods or beverages that need to be avoided with DOACs? Unlike with warfarin, there are no known food interactions with DOACs, so there are no food restrictions when taking these medications. In addition, there is no evidence that drinking grapefruit juice affects the effectiveness or safety of DOACs. In general, it is acceptable for patients taking a DOAC to drink alcoholic beverages in moderation (e.g. a glass of wine with a meal) as it is for patients on warfarin. -

Atrial Fibrillation
CONFIDENTIAL NATIONAL INSTITUTE FOR HEALTH AND CLINICAL EXCELLENCE Premeeting briefing Dabigatran for the prevention of stroke and systemic embolism in atrial fibrillation This briefing presents the key issues arising from the manufacturer’s submission, Evidence Review Group (ERG) report and statements made by consultees and their nominated clinical specialists and patient experts. Please note that this briefing is a summary of the information available and should be read with the full supporting documents. The manufacturer was asked to…. provide justification for reducing the dabigatran treatment dose from 150 mg to 110 mg at 80 years of age comment on the impact of being unable to utilise P-glycoprotein inhibitors on the use of dabigatran and the management of atrial fibrillation provide a justification for choosing the mixed treatment comparison (MTC) (SAS) for the base case instead of the results from the MTC (WinBUGs) provide a comparison of the different hazard ratios from the MTC (SAS), MTC (WinBUGS) analyses and the direct pairwise results and justify any discrepancies justify the exclusion of trials with zero event arms from the MTC provide a revised model with the ability to choose any of the included treatments (dabigatran or warfarin) as either a first-line or a second-line treatment option provide base-case cost-effectiveness results comparing dabigatran 110 mg and 150 mg when used as either first-line treatment or as a second-line treatment following warfarin analyse and provide base-case cost-effectiveness comparing the results of the following treatment sequences: dabigatran → warfarin → aspirin → no treatment and warfarin → aspirin → no treatment. -

Laboratory Monitoring of Direct Oral Anticoagulants (Doacs)
biomedicines Review Laboratory Monitoring of Direct Oral Anticoagulants (DOACs) Claire Dunois HYPHEN BioMed, Sysmex Group, 95000 Neuville sur Oise, France; [email protected] Abstract: The introduction of direct oral anticoagulants (DOACs), such as dabigatran, rivaroxaban, apixaban, edoxaban, and betrixaban, provides safe and effective alternative to previous anticoagulant therapies. DOACs directly, selectively, and reversibly inhibit factors IIa or Xa. The coagulation effect follows the plasma concentration–time profile of the respective anticoagulant. The short half-life of a DOAC constrains the daily oral intake. Because DOACs have predictable pharmacokinetic and pharmacodynamic responses at a fixed dose, they do not require monitoring. However in specific clinical situations and for particular patient populations, testing may be helpful for patient management. The effect of DOACs on the screening coagulation assays such as prothrombin time (PT), activated partial thromboplastin time (APTT), and thrombin time (TT) is directly linked to reagent composition, and clotting time can be different from reagent to reagent, depending on the DOAC’s reagent sensitivity. Liquid chromatography–mass spectrometry (LC-MS/MS) is considered the gold standard method for DOAC measurement, but it is time consuming and requires expensive equipment. The general consensus for the assessment of a DOAC is clotting or chromogenic assays using specific standard calibrators and controls. This review provides a short summary of DOAC properties and an update on laboratory methods for measuring DOACs. Keywords: DOAC; monitoring; screening assays; quantitative assays Citation: Dunois, C. Laboratory Monitoring of Direct Oral Anticoagulants (DOACs). 1. Introduction Biomedicines 2021, 9, 445. https:// Direct oral anticoagulants (DOACs) constitute first-line therapy used for many throm- doi.org/10.3390/biomedicines9050445 boembolic indications, such as prevention and treatment of venous thromboembolism (VTE) and stroke prevention in atrial fibrillation (AF) [1,2]. -

Anticoagulant Pradaxa (Dabigatran Etexilate Mesylate) Savaysa (Edoxaban) Xarelto 2.5Mg (Rivaroxaban) Effective 01/01/2021
Anticoagulant Pradaxa (dabigatran etexilate mesylate) Savaysa (edoxaban) Xarelto 2.5mg (rivaroxaban) Effective 01/01/2021 ☒ MassHealth Plan ☒ ☐Commercial/Exchange Prior Authorization Program Type ☒ Quantity Limit ☒ Pharmacy Benefit Benefit ☐ Step Therapy ☐ Medical Benefit (NLX) Specialty N/A Limitations Specialty Medications All Plans Phone: 866-814-5506 Fax: 866-249-6155 Non-Specialty Medications Contact MassHealth Phone: 877-433-7643 Fax: 866-255-7569 Information Commercial Phone: 800-294-5979 Fax: 888-836-0730 Exchange Phone: 855-582-2022 Fax: 855-245-2134 Medical Specialty Medications (NLX) All Plans Phone: 844-345-2803 Fax: 844-851-0882 Exceptions N/A Overview Xarelto and Savaysa are factor Xa inhibitors which inhibit platelet activation and fibrin clot formation. Pradaxa is a thrombin inhibitor which blocks free and fibrin bound thrombin. These medications are indicated for: . Treatment of deep venous thrombosis (DVT) and pulmonary embolism (PE) – Pradaxa and Savaysa . Prevention of stroke and systemic embolism in patients with nonvalvular atrial fibrillation. – Pradaxa, Xarelto, and Savaysa . Prophylaxis of DVT and/or PE in patients who have undergone total hip arthroplasty. - Xarelto and Pradaxa . Prophylaxis of venous thromboembolism (VTE) – Xarelto . Reduction in the risk of recurrence of deep vein thrombosis (DVT) and pulmonary embolism (PE) – Xarelto . Reduction of risk of major cardiovascular (CV) events (CV death, myocardial infarction, and stroke) in patients with coronary artery disease (chronic) or peripheral artery disease. - Xarelto No PA PA required Pradaxa® (dabigatran etexilate mesylate 110 mg) ≤ 70 Pradaxa® (dabigatran etexilate mesylate 75 mg, 150 capsules/365 days mg) Pradaxa® (dabigatran etexilate mesylate 110 mg) > 70 Eliquis® (apixaban) PD capsules/365 days ® ® Xarelto (rivaroxaban 10 mg, 15 mg, 20 mg, starter pack) Savaysa (edoxaban) ® Xarelto (rivaroxaban 2.5 mg tablet) PD Preferred Drug. -

Estonian Statistics on Medicines 2016 1/41
Estonian Statistics on Medicines 2016 ATC code ATC group / Active substance (rout of admin.) Quantity sold Unit DDD Unit DDD/1000/ day A ALIMENTARY TRACT AND METABOLISM 167,8985 A01 STOMATOLOGICAL PREPARATIONS 0,0738 A01A STOMATOLOGICAL PREPARATIONS 0,0738 A01AB Antiinfectives and antiseptics for local oral treatment 0,0738 A01AB09 Miconazole (O) 7088 g 0,2 g 0,0738 A01AB12 Hexetidine (O) 1951200 ml A01AB81 Neomycin+ Benzocaine (dental) 30200 pieces A01AB82 Demeclocycline+ Triamcinolone (dental) 680 g A01AC Corticosteroids for local oral treatment A01AC81 Dexamethasone+ Thymol (dental) 3094 ml A01AD Other agents for local oral treatment A01AD80 Lidocaine+ Cetylpyridinium chloride (gingival) 227150 g A01AD81 Lidocaine+ Cetrimide (O) 30900 g A01AD82 Choline salicylate (O) 864720 pieces A01AD83 Lidocaine+ Chamomille extract (O) 370080 g A01AD90 Lidocaine+ Paraformaldehyde (dental) 405 g A02 DRUGS FOR ACID RELATED DISORDERS 47,1312 A02A ANTACIDS 1,0133 Combinations and complexes of aluminium, calcium and A02AD 1,0133 magnesium compounds A02AD81 Aluminium hydroxide+ Magnesium hydroxide (O) 811120 pieces 10 pieces 0,1689 A02AD81 Aluminium hydroxide+ Magnesium hydroxide (O) 3101974 ml 50 ml 0,1292 A02AD83 Calcium carbonate+ Magnesium carbonate (O) 3434232 pieces 10 pieces 0,7152 DRUGS FOR PEPTIC ULCER AND GASTRO- A02B 46,1179 OESOPHAGEAL REFLUX DISEASE (GORD) A02BA H2-receptor antagonists 2,3855 A02BA02 Ranitidine (O) 340327,5 g 0,3 g 2,3624 A02BA02 Ranitidine (P) 3318,25 g 0,3 g 0,0230 A02BC Proton pump inhibitors 43,7324 A02BC01 Omeprazole -

Center for Drug Evaluation and Research Application
CENTER FOR DRUG EVALUATION AND RESEARCH APPLICATION NUMBER: 22-512 PHARMACOLOGY REVIEW(S) Tertiary Pharmacology Review By: Paul C. Brown, Ph.D., ODE Associate Director for Pharmacology and Toxicology OND IO NDA: 22-307 Submission date: 4/19/2010 Drug: Pradaxa™ (Dabigatran etexilate mesylate) Sponsor: Boehringer Ingelheim Pharma GmbH & Co. KG Indication: Prevention of stroke and systemic embolism in patients with atrial fibrillation Reviewing Division: Division of Cardiovascular and Renal Products Comments: The pharm/tox reviewer and supervisor found the nonclinical information submitted for dabigatran to be sufficient to support the proposed use. The reviewer proposes pregnancy category C for the labeling. Dabigatran induced some reproductive toxicity in rats manifest as a decreased number of implantations, decreased number of viable fetuses, increase in the resorption rate, increase in post-implantation loss, and an increase in the number of dead offspring when given at doses of 70 mg/kg (about 2.6 to 3 times the MRHD of 300 mg/day on a mg/m2 basis). Dabigatran also induced some fetal structural variations but did not induce fetal malformations in rats or rabbits. Dabigatran was evaluated for carcinogenicity in 2-year rat and mouse studies. The Executive Carcinogenicity Assessment Committee concluded that these studies were adequate and there were no drug-related tumors in either study. Conclusions: I concur with the Division pharm/tox conclusion that the nonclinical data support approval of this NDA. No additional nonclinical studies are recommended at this time. The proposed Established Pharmacologic Class for dabigatran is "direct thrombin inhibitor". This is appropriate because it is consistent with other moieties of this class. -

Periprocedural Management of Patients on Dabigatran Etexilate
Periprocedural Management of Patients on Dabigatran lation tests are not necessary to monitor the effect of dabigatran. Etexilate Treatment However, there is a need to quantitate the intensity of anticoagulation Dabigatran etexilate is a direct thrombin inhibitor that was initially activity of dabigatran in such settings. Other tests such as the throm- introduced for oral anticoagulation for the prevention or treatment of bin time, activated partial thromboplastin time (aPTT), and ecarin venous thrombosis.1 After the recently concluded phase III trial Ran- clotting time have been reported to correlate with dabigatran serum domized Evaluation of Long-Term Anticoagulation Therapy,2 dab- concentration.3 4 igatran has been approved by the US Food and Drug Administration The Interventional Management of Stroke (IMS) III trial pro- as a potential replacement for warfarin in patients with nonvalvular posed that administration of tissue plasminogen activator or endo- atrial fibrillation to reduce the risk of stroke and systemic embolism. vascular intervention could be considered in patients at 48 hours after Dabigatran was administered, in a blinded fashion, in capsules con- last intake of dabigatran, or within 48 hours of the last intake and with taining either 110 or 150 mg of the drug, to be taken twice daily. normal aPTT in the same way as heparin. Because no guidelines exist With the anticipated increase in dabigatran use, neurointerven- on how to monitor the therapeutic activity effect of dabigatran accu- tionalists will face the challenge of making treatment decisions in rately, emergent neurointerventional procedures in dabigatran- patients on dabigatran. Patients with therapeutic levels of dabigatran treated patients should be approached cautiously. -

PRADAXA Safely and Effectively
HIGHLIGHTS OF PRESCRIBING INFORMATION ----------------------DOSAGE AND ADMINISTRATION---------------------- These highlights do not include all the information needed to use Non-valvular Atrial Fibrillation: PRADAXA safely and effectively. See full prescribing information for o For patients with CrCl >30 mL/min: 150 mg orally, twice daily (2.1) PRADAXA. o For patients with CrCl 15-30 mL/min: 75 mg orally, twice daily (2.1) Treatment of DVT and PE: PRADAXA® (dabigatran etexilate mesylate) capsules, for oral use o For patients with CrCl >30 mL/min: 150 mg orally, twice daily after Initial U.S. Approval: 2010 5-10 days of parenteral anticoagulation (2.1) Reduction in the Risk of Recurrence of DVT and PE: WARNING: (A) PREMATURE DISCONTINUATION OF PRADAXA o For patients with CrCl >30 mL/min: 150 mg orally, twice daily after INCREASES THE RISK OF THROMBOTIC EVENTS, and previous treatment (2.1) (B) SPINAL/EPIDURAL HEMATOMA Prophylaxis of DVT and PE Following Hip Replacement Surgery: See full prescribing information for complete boxed warning o For patients with CrCl >30 mL/min: 110 mg orally first day, then 220 mg once daily (2.1) (A) PREMATURE DISCONTINUATION OF PRADAXA INCREASES Review recommendations for converting to or from other oral or parenteral THE RISK OF THROMBOTIC EVENTS: Premature discontinuation of anticoagulants (2.4, 2.5) any oral anticoagulant, including PRADAXA, increases the risk of Temporarily discontinue PRADAXA before invasive or surgical thrombotic events. To reduce this risk, consider coverage with another procedures when possible, then restart promptly (2.6) anticoagulant if PRADAXA is discontinued for a reason other than pathological bleeding or completion of a course of therapy (2.4, 2.5, 2.6, ---------------------DOSAGE FORMS AND STRENGTHS--------------------- 5.1). -

Estonian Statistics on Medicines 2013 1/44
Estonian Statistics on Medicines 2013 DDD/1000/ ATC code ATC group / INN (rout of admin.) Quantity sold Unit DDD Unit day A ALIMENTARY TRACT AND METABOLISM 146,8152 A01 STOMATOLOGICAL PREPARATIONS 0,0760 A01A STOMATOLOGICAL PREPARATIONS 0,0760 A01AB Antiinfectives and antiseptics for local oral treatment 0,0760 A01AB09 Miconazole(O) 7139,2 g 0,2 g 0,0760 A01AB12 Hexetidine(O) 1541120 ml A01AB81 Neomycin+Benzocaine(C) 23900 pieces A01AC Corticosteroids for local oral treatment A01AC81 Dexamethasone+Thymol(dental) 2639 ml A01AD Other agents for local oral treatment A01AD80 Lidocaine+Cetylpyridinium chloride(gingival) 179340 g A01AD81 Lidocaine+Cetrimide(O) 23565 g A01AD82 Choline salicylate(O) 824240 pieces A01AD83 Lidocaine+Chamomille extract(O) 317140 g A01AD86 Lidocaine+Eugenol(gingival) 1128 g A02 DRUGS FOR ACID RELATED DISORDERS 35,6598 A02A ANTACIDS 0,9596 Combinations and complexes of aluminium, calcium and A02AD 0,9596 magnesium compounds A02AD81 Aluminium hydroxide+Magnesium hydroxide(O) 591680 pieces 10 pieces 0,1261 A02AD81 Aluminium hydroxide+Magnesium hydroxide(O) 1998558 ml 50 ml 0,0852 A02AD82 Aluminium aminoacetate+Magnesium oxide(O) 463540 pieces 10 pieces 0,0988 A02AD83 Calcium carbonate+Magnesium carbonate(O) 3049560 pieces 10 pieces 0,6497 A02AF Antacids with antiflatulents Aluminium hydroxide+Magnesium A02AF80 1000790 ml hydroxide+Simeticone(O) DRUGS FOR PEPTIC ULCER AND GASTRO- A02B 34,7001 OESOPHAGEAL REFLUX DISEASE (GORD) A02BA H2-receptor antagonists 3,5364 A02BA02 Ranitidine(O) 494352,3 g 0,3 g 3,5106 A02BA02 Ranitidine(P) -

PDF Download
Review Article 201 How Do I Reverse Oral and Parenteral Anticoagulants? Wie Reversiere ich die Wirkung von Oralen und Parenteralen Antikoagulanzien? Jürgen Koscielny1 Edita Rutkauskaite1 Christoph Sucker2 Christian von Heymann3 1 Charité, Universitätsmedizin Berlin, Gerinnungsambulanz mit Address for correspondence Jürgen Koscielny, Charité, Hämophiliezentrum im Ambulanten, Gesundheitszentrum (AGZ), Universitätsmedizin Berlin, Gerinnungsambulanz mit Berlin, Germany HämophiliezentrumimAmbulantenGesundheitszentrum(AGZ), 2 Gerinnungszentrum Berlin Dr. Sucker, Berlin, Germany Berlin, Germany (e-mail: [email protected]). 3 Klinik für Anästhesie, Intensivmedizin, Notfallmedizin und Schmerztherapie, Vivantes Klinikum, Im Friedrichshain, Berlin, Germany Hämostaseologie 2020;40:201–213. Abstract An understanding of reversal strategies alone is important to safely and effectively care for patients in cases of bleeding or invasive procedures. The recent diversification in the number of licensed anticoagulants makes an understanding of drug-specific reversal strategies essential. Intravenous or oral vitamin K can reverse the effect of vitamin K antagonists (VKAs) within 12 to 48 hours and is indicated for any bleeding or an international normalized ratio >10 or 4.5 to 10 in patients with additional risk factors for bleeding. Furthermore, an additional administration of prothrombin complex concentrate (PCC) may be necessary in cases of major bleeding related to VKA. Protamine (chloride or sulfate) fully reverses the effect of unfractionated heparin and partially in low-molecular-weight heparin. Idarucizumab has been approved for dabigatran reversal, whereas andexanet alfa is approved for the reversal of some oral factor Xa inhibitors (apixaban, rivaroxaban). PCC seems to enhance the haemo- static potential for the reversal of the effect of FXa-inhibitors. So far, there are promising but only limited data on the efficacy of this approach available. -
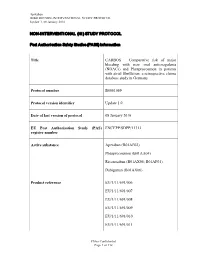
Non-Interventional (Ni) Study Protocol
Apixaban B0661069 NON-INTERVENTIONAL STUDY PROTOCOL Update 1, 08 January 2016 NON-INTERVENTIONAL (NI) STUDY PROTOCOL Post Author isation Safet y St udi es (PA SS) infor mation Title CARBOS – Comparative risk of major bleeding with new oral anticoagulants (NOACs) and Phenprocoumon in patients with atrial fibrillation: a retrospective claims database study in Germany Protocol number B0661069 Protocol version identifier Update 1.0 Date of last version of protocol 08 January 2016 EU Post Authorisation Study (PAS) ENCEPP/SDPP/11313 register number Active substance Apixaban (B01AF02) Phenprocoumon (B01AA04) Rivaroxaban (B01AX06; B01AF01) Dabigatran (B01AX06) Product reference EU/1/11/691/006 EU/1/11/691/007 EU/1/11/691/008 EU/1/11/691/009 EU/1/11/691/010 EU/1/11/691/011 Pfizer Confidential Page 1 of 112 Apixaban B0661069 NON-INTERVENTIONAL STUDY PROTOCOL Update 1, 08 January 2016 EU/1/11/691/012 EU/1/11/691/014 Procedure number Not Available Marketing Authorisation Holder (MAH) Pfizer Pharma GmbH Joint PASS No Research question and objectives The aim of this study is to investigate whether there are differences in the occurrence of major bleeding events in patients with NVAF and prescribed oral anticoagulation therapies in a real-world setting. It will be investigated whether the occurrence of major bleeding events in NVAF patients under anticoagulant therapy differs between patients treated with VKA (e.g. Phenprocoumon) and patients treated with Apixaban, Dabigatran or Rivaroxaban respectively. Country of study Germany Author Fabian Volz Pfizer