Hdl 43384.Pdf
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

A Computational Approach for Defining a Signature of Β-Cell Golgi Stress in Diabetes Mellitus
Page 1 of 781 Diabetes A Computational Approach for Defining a Signature of β-Cell Golgi Stress in Diabetes Mellitus Robert N. Bone1,6,7, Olufunmilola Oyebamiji2, Sayali Talware2, Sharmila Selvaraj2, Preethi Krishnan3,6, Farooq Syed1,6,7, Huanmei Wu2, Carmella Evans-Molina 1,3,4,5,6,7,8* Departments of 1Pediatrics, 3Medicine, 4Anatomy, Cell Biology & Physiology, 5Biochemistry & Molecular Biology, the 6Center for Diabetes & Metabolic Diseases, and the 7Herman B. Wells Center for Pediatric Research, Indiana University School of Medicine, Indianapolis, IN 46202; 2Department of BioHealth Informatics, Indiana University-Purdue University Indianapolis, Indianapolis, IN, 46202; 8Roudebush VA Medical Center, Indianapolis, IN 46202. *Corresponding Author(s): Carmella Evans-Molina, MD, PhD ([email protected]) Indiana University School of Medicine, 635 Barnhill Drive, MS 2031A, Indianapolis, IN 46202, Telephone: (317) 274-4145, Fax (317) 274-4107 Running Title: Golgi Stress Response in Diabetes Word Count: 4358 Number of Figures: 6 Keywords: Golgi apparatus stress, Islets, β cell, Type 1 diabetes, Type 2 diabetes 1 Diabetes Publish Ahead of Print, published online August 20, 2020 Diabetes Page 2 of 781 ABSTRACT The Golgi apparatus (GA) is an important site of insulin processing and granule maturation, but whether GA organelle dysfunction and GA stress are present in the diabetic β-cell has not been tested. We utilized an informatics-based approach to develop a transcriptional signature of β-cell GA stress using existing RNA sequencing and microarray datasets generated using human islets from donors with diabetes and islets where type 1(T1D) and type 2 diabetes (T2D) had been modeled ex vivo. To narrow our results to GA-specific genes, we applied a filter set of 1,030 genes accepted as GA associated. -
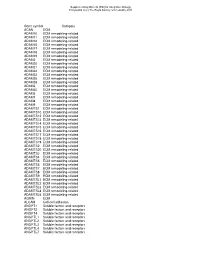
Gene Symbol Category ACAN ECM ADAM10 ECM Remodeling-Related ADAM11 ECM Remodeling-Related ADAM12 ECM Remodeling-Related ADAM15 E
Supplementary Material (ESI) for Integrative Biology This journal is (c) The Royal Society of Chemistry 2010 Gene symbol Category ACAN ECM ADAM10 ECM remodeling-related ADAM11 ECM remodeling-related ADAM12 ECM remodeling-related ADAM15 ECM remodeling-related ADAM17 ECM remodeling-related ADAM18 ECM remodeling-related ADAM19 ECM remodeling-related ADAM2 ECM remodeling-related ADAM20 ECM remodeling-related ADAM21 ECM remodeling-related ADAM22 ECM remodeling-related ADAM23 ECM remodeling-related ADAM28 ECM remodeling-related ADAM29 ECM remodeling-related ADAM3 ECM remodeling-related ADAM30 ECM remodeling-related ADAM5 ECM remodeling-related ADAM7 ECM remodeling-related ADAM8 ECM remodeling-related ADAM9 ECM remodeling-related ADAMTS1 ECM remodeling-related ADAMTS10 ECM remodeling-related ADAMTS12 ECM remodeling-related ADAMTS13 ECM remodeling-related ADAMTS14 ECM remodeling-related ADAMTS15 ECM remodeling-related ADAMTS16 ECM remodeling-related ADAMTS17 ECM remodeling-related ADAMTS18 ECM remodeling-related ADAMTS19 ECM remodeling-related ADAMTS2 ECM remodeling-related ADAMTS20 ECM remodeling-related ADAMTS3 ECM remodeling-related ADAMTS4 ECM remodeling-related ADAMTS5 ECM remodeling-related ADAMTS6 ECM remodeling-related ADAMTS7 ECM remodeling-related ADAMTS8 ECM remodeling-related ADAMTS9 ECM remodeling-related ADAMTSL1 ECM remodeling-related ADAMTSL2 ECM remodeling-related ADAMTSL3 ECM remodeling-related ADAMTSL4 ECM remodeling-related ADAMTSL5 ECM remodeling-related AGRIN ECM ALCAM Cell-cell adhesion ANGPT1 Soluble factors and receptors -

Anti-Matrix Metalloproteinase-25, Propeptide Region Developed in Rabbit Affinity Isolated Antibody
Anti-Matrix Metalloproteinase-25, Propeptide Region Developed in Rabbit Affinity Isolated Antibody Product Number M 5067 Product Description structurally. They fall within the matrixin subfamily and Anti-Matrix Metalloproteinase-25 (MMP-25), Propeptide are EC designated 3.4.24.x. This group also contains Region is developed in rabbit using a synthetic peptide astacin, reprolysin, and serralysin, as well as other corresponding to the propeptide region of human matrix more divergent metalloproteinases. All MMPs are metalloproteinase-25 (MMP-25), also known as synthesized as proenzymes, and most of them are membrane-type matrix metalloproteinase-6 (MT6-MMP) secreted from the cells as proenzymes. Thus, the as immunogen. Affinity isolated antigen specific activation of these proenzymes is a critical step that antibody is obtained from rabbit anti-MMP-25 antiserum leads to extracellular matrix breakdown. by immuno-specific purification which removes essentially all rabbit serum proteins, including MMPs are considered to play an important role in immunoglobulins, which do not specifically bind to the wound healing, apoptosis, bone elongation, embryo peptide. development, uterine involution, angiogenesis, 4 and tissue remodeling, and in diseases such as multiple Anti-Matrix Metalloproteinase-25, Propeptide Region sclerosis, 2, 5 Alzheimer’s, 2 malignant gliomas, 2 lupus, may be used for the detection and localization of arthritis, periodontis, glumerulonephritis, human and murine matrix metalloproteinase-25 atherosclerosis, tissue ulceration, and in cancer cell (MMP-25, MT6-MMP). The antibody binds to the invasion and metastasis.6 Numerous studies have propeptide domain of MMP-25 and does not cross react shown that there is a close association between with the other MMP family members (MMP-1, MMP-2, expression of various members of the MMP family by MMP-3, MMP-9, etc.). -

Ivtigation of the Effects of Mechanical Strain in Human Tenocytes
Investigation of the effects of Mechanical Strain in Human Tenocytes Eleanor Rachel Jones In partial fulfilment of the requirements for the Degree of Doctor of Philosophy University of East Anglia, Biological Sciences September 2012 This copy of the thesis has been supplied on condition that anyone who consults it is understood to recognise that its copyright rests with the author and that use of any information derived there from must be in accordance with current UK Copyright Law. In addition, any quotation or extract must be included full attribution. Abstract Tendinopathies are a range of diseases characterised by pain and insidious degeneration. Although poorly understood, onset is often associated with physical activity. Metalloproteinases are regulated differentially in tendinopathy causing disruptions in extracellular matrix (ECM) homeostasis. An increase in the anti-inflammatory cytokine TGFβ has also been documented. This project aims to investigate the effect of cyclic tensile strain loading and TGFβ stimulation on protease and ECM protein expression by human tenocytes and begin to characterise the pathway of mechanotransduction. Human tenocytes were seeded at 1.5x106 cells/ml into collagen gels (rat tail type I, 1mg/ml) and stretched using a sinusoidal waveform of 0-5% at 1Hz using the Flexcell FX4000T™ system. Cultures were treated with or without 1ng/ml TGFβ1 or inhibitors of TGFβRI, metalloproteinases, RGD, Mannose-6-phosphate, integrin β1 and a thrombospondin as appropriate. qRT-PCR and a cell based luciferase assay were used to assess RNA and TGFβ activity respectively. The prolonged application of 5% cyclic mechanical strain in a 3D culture system induced an anabolic response in protease and matrix genes. -

Matrix Metalloproteinase-11 Promotes Mouse Mammary Gland Tumor Progression Bing Tan
Matrix metalloproteinase-11 promotes mouse mammary gland tumor progression Bing Tan To cite this version: Bing Tan. Matrix metalloproteinase-11 promotes mouse mammary gland tumor progression. Ge- nomics [q-bio.GN]. Université de Strasbourg, 2018. English. NNT : 2018STRAJ047. tel-02870898 HAL Id: tel-02870898 https://tel.archives-ouvertes.fr/tel-02870898 Submitted on 17 Jun 2020 HAL is a multi-disciplinary open access L’archive ouverte pluridisciplinaire HAL, est archive for the deposit and dissemination of sci- destinée au dépôt et à la diffusion de documents entific research documents, whether they are pub- scientifiques de niveau recherche, publiés ou non, lished or not. The documents may come from émanant des établissements d’enseignement et de teaching and research institutions in France or recherche français ou étrangers, des laboratoires abroad, or from public or private research centers. publics ou privés. UNIVERSITÉ DE STRASBOURG ÉCOLE DOCTORALE DES SCIENCES DE LA VIE ET DE LA SANTÉ Thèse présentée par Bing TAN Pour obtenir le grade de Docteur de l’Université de Strasbourg Sciences du Vivant Aspects Moléculaires et Cellulaires de la Biologie La métalloprotéase matricielle-11 facilite la progression des tumeurs de la glande mammaire murine Matrix metalloproteinase-11 promotes mouse mammary gland tumor progression Soutenue publiquement le 13 septembre 2018 Devant le jury composé de: Examinateur: Madame le Docteur Isabelle GRILLIER-VUISSOZ Rapporteurs Externe: Madame le Docteur Emmanuelle LIAUDET-COOPMAN Monsieur le Docteur Stéphane DEDIEU Rapporteur Interne: Monsieur le Docteur Olivier LEFEBVRE Directeur de Thèse: Madame le Docteur Catherine-Laure TOMASETTO Acknowledgements The completion of my PhD thesis is attributed to many people’s support. -

The Pharmacological TAILS of Matrix Metalloproteinases and Their Inhibitors
pharmaceuticals Review The Pharmacological TAILS of Matrix Metalloproteinases and Their Inhibitors Nabangshu Das 1,2,†, Colette Benko 2,3,†, Sean E. Gill 4,5 and Antoine Dufour 1,2,3,* 1 Faculty of Kinesiology, University of Calgary, Calgary, AB T2N 4N1, Canada; [email protected] 2 McCaig Institute for Bone and Join Healthy, 3280 Hospital Drive NW, Calgary, AB T2N 4Z6, Canada; [email protected] 3 Department of Physiology and Pharmacology, Cumming School of Medicine, Foothills Hospital, 3330 Hospital Dr, Calgary, AB T2N 4N1, Canada 4 Centre for Critical Illness Research, Victoria Research Labs, Lawson Health Research Institute, A6-134, London, ON N6A 5W9, Canada; [email protected] 5 Division of Respirology, Department of Medicine, Western University, London, ON N6A 5W9, Canada * Correspondence: [email protected] † These authors contributed equally. Abstract: Matrix metalloproteinases (MMPs) have been demonstrated to have both detrimental and protective functions in inflammatory diseases. Several MMP inhibitors, with the exception of Periostat®, have failed in Phase III clinical trials. As an alternative strategy, recent efforts have been focussed on the development of more selective inhibitors or targeting other domains than their active sites through specific small molecule inhibitors or monoclonal antibodies. Here, we present some examples that aim to better understand the mechanisms of conformational changes/allosteric control of MMPs functions. In addition to MMP inhibitors, we discuss unbiased global approaches, such as proteomics and N-terminomics, to identify new MMP substrates. We present some examples of new MMP substrates and their implications in regulating biological functions. By characterizing the roles and substrates of individual MMP, MMP inhibitors could be utilized more effectively in the optimal disease context or in diseases never tested before where MMP activity is elevated and contributing to disease progression. -

Expression of the Matrix Metalloproteases 2, 14, 24, and 25 and Tissue Inhibitor 3 As Potential Molecular Markers in Advanced Human Gastric Cancer
Hindawi Publishing Corporation Disease Markers Volume 2014, Article ID 285906, 9 pages http://dx.doi.org/10.1155/2014/285906 Research Article Expression of the Matrix Metalloproteases 2, 14, 24, and 25 and Tissue Inhibitor 3 as Potential Molecular Markers in Advanced Human Gastric Cancer Sol de la Peña,1 Clara Luz Sampieri,2 Mariana Ochoa-Lara,3 Kenneth León-Córdoba,4 and José María Remes-Troche5 1 Biomedical Sciences Doctoral Program, Biomedical Research Center, University of Veracruz, 91190 Xalapa, Veracruz, Mexico 2 Institute of Public Health, University of Veracruz, 91190 Xalapa, Veracruz, Mexico 3 Public Health Master Program, University of Veracruz, 91190 Xalapa, Veracruz, Mexico 4 Dr. Miguel Dorantes Mesa Hospital, 91130 Xalapa, Veracruz, Mexico 5 Medical-Biological Research Institute, University of Veracruz, 91700 Veracruz, Veracruz, Mexico Correspondence should be addressed to Clara Luz Sampieri; [email protected] Received 9 February 2013; Accepted 27 November 2013; Published 11 February 2014 Academic Editor: Stamatios Theocharis Copyright © 2014 Sol de la Pena˜ et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Background. During progression of gastric cancer (GC), degradation of the extracellular matrix is mediated by the matrix metalloproteases (MMPs) and their tissue inhibitors (TIMPs): changes in the expression of these have been related to unfavorable prognosis in GC. Objective. To analyze the expression of certain MMPs and TIMPs in chronic superficial gastritis (SG) and GC. Methods. The expression of MMPs and TIMPs was determined using qRT-PCR; the expression was classified, using threshold cycle () values, as very high ( ≤25), high ( =26–30), moderate ( =31–35), low ( =36–39), or not detected ( =40). -

MMP25 Polyclonal Antibody
MMP25 polyclonal antibody processes, such as embryonic development, reproduction, and tissue remodeling, as well as in Catalog Number: PAB4790 disease processes, such as arthritis and metastasis. Most MMPs are secreted as inactive proproteins which Regulatory Status: For research use only (RUO) are activated when cleaved by extracellular proteinases. However, the protein encoded by this gene is a member Product Description: Rabbit polyclonal antibody raised of the membrane-type MMP (MT-MMP) subfamily, against synthetic peptide of MMP25. attached to the plasma membrane via a glycosylphosphatidyl inositol anchor. In response to Immunogen: A synthetic peptide (conjugated with KLH) bacterial infection or inflammation, the encoded protein corresponding to C-terminus of human MMP25. is thought to inactivate alpha-1 proteinase inhibitor, a major tissue protectant against proteolytic enzymes Host: Rabbit released by activated neutrophils, facilitating the Reactivity: Human,Mouse transendothelial migration of neutrophils to inflammatory sites. The encoded protein may also play a role in tumor Applications: ELISA, WB invasion and metastasis through activation of MMP2. (See our web site product page for detailed applications The gene has previously been referred to as MMP20 but information) has been renamed MMP25. [provided by RefSeq] Protocols: See our web site at References: http://www.abnova.com/support/protocols.asp or product 1. Clusterin, an abundant serum factor, is a possible page for detailed protocols negative regulator of MT6-MMP/MMP-25 produced by neutrophils. Matsuda A, Itoh Y, Koshikawa N, Akizawa Form: Liquid T, Yana I, Seiki M. J Biol Chem. 2003 Sep 19;278(38):36350-7. Epub 2003 Jul 14. Purification: Protein G purification 2. -

Expression Profiles and Clinical Correlations of Degradome Components in the Tumor Microenvironment of Head and Neck Squamous Cell Carcinoma
Published OnlineFirst March 21, 2010; DOI: 10.1158/1078-0432.CCR-09-2525 Clinical Human Cancer Biology Cancer Research Expression Profiles and Clinical Correlations of Degradome Components in the Tumor Microenvironment of Head and Neck Squamous Cell Carcinoma Angela Stokes1, Juho Joutsa6,7,8,9, Risto Ala-aho6,8, Mark Pitchers1, Caroline J. Pennington1, Craig Martin2, Don J. Premachandra3, Yasunori Okada10, Juha Peltonen4, Reidar Grénman5,7, Helen A. James1, Dylan R. Edwards1, and Veli-Matti Kähäri6,7,8 Abstract Purpose: Head and neck squamous cell carcinomas (HNSCC) are characterized by high morbidity and mortality, largely due to the high invasive and metastatic potential of these tumors, high recurrence rates, and low treatment responses. Proteinases have been implicated in several aspects of tumor growth and metastasis in a broad range of tumors including HNSCC. Experimental Design: Comprehensive expression profiling of proteinases [matrix metalloproteinases (MMPs), A disintegrin and metalloproteinase (ADAMs), and ADAMs with thrombospondin motif (ADAMTSs)] and their inhibitors [tissue inhibitor of metalloproteinases (TIMPs)] was done using quanti- tative real-time reverse transcription-PCR analysis of a large cohort of tissue samples representing the tumor (n = 83), the invasive margin (n = 41), and the adjacent tissue (n = 41) from 83 HNSCC patients, along with normal tissue controls (n = 13), as well as cell lines established from tumors of 34 HNSCC patients. Results: The results show specifically elevated gene expression of several proteinases, including MMP1, MMP3, MMP10, and MMP13 within tumor tissue and peritumoral adjacent tissue. In addition, the results identify several novel HNSCC-associated proteinases, including ADAM8, ADAM9, ADAM17, ADAM28, ADAMTS1, ADAMTS8, and ADAMTS15. -

MMP14 in Sarcoma: a Regulator of Tumor Microenvironment Communication in Connective Tissues
cells Review MMP14 in Sarcoma: A Regulator of Tumor Microenvironment Communication in Connective Tissues Jordi Gonzalez-Molina 1,2,*, Silvia Gramolelli 3, Zehuan Liao 1,4 , Joseph W. Carlson 2, Päivi M. Ojala 3,5 and Kaisa Lehti 1,6,* 1 Department of Microbiology, Tumor and Cell Biology (MTC), Karolinska Institutet, 17177 Stockholm, Sweden 2 Department of Oncology-Pathology, Karolinska Institutet, 17176 Stockholm, Sweden 3 Translational Cancer Medicine Research Program, Faculty of Medicine, University of Helsinki, 00014 Helsinki, Finland 4 School of Biological Sciences, Nanyang Technological University Singapore, 60 Nanyang Drive, Singapore 637551, Singapore 5 Section of Virology, Division of Infectious Diseases, Department of Medicine, Imperial College London, London W2 1NY, UK 6 Individualized Drug Therapy Research Program, Faculty of Medicine, University of Helsinki, 00014 Helsinki, Finland * Correspondence: [email protected] (J.G.-M.); [email protected] (K.L.); Tel.: +46-(0)8-5248-6427 (J.G.-M.); +46-(0)8-5248-5254 (K.L.) Received: 31 July 2019; Accepted: 27 August 2019; Published: 28 August 2019 Abstract: Sarcomas are deadly malignant tumors of mesenchymal origin occurring at all ages. The expression and function of the membrane-type matrix metalloproteinase MMP14 is closely related to the mesenchymal cell phenotype, and it is highly expressed in most sarcomas. MMP14 regulates the activity of multiple extracellular and plasma membrane proteins, influencing cell–cell and cell–extracellular matrix (ECM) communication. This regulation mediates processes such as ECM degradation and remodeling, cell invasion, and cancer metastasis. Thus, a comprehensive understanding of the biology of MMP14 in sarcomas will shed light on the mechanisms controlling the key processes in these diseases. -

Lineage-Specific Effector Signatures of Invariant NKT Cells Are Shared Amongst Δγ T, Innate Lymphoid, and Th Cells
Downloaded from http://www.jimmunol.org/ by guest on September 26, 2021 δγ is online at: average * The Journal of Immunology , 10 of which you can access for free at: 2016; 197:1460-1470; Prepublished online 6 July from submission to initial decision 4 weeks from acceptance to publication 2016; doi: 10.4049/jimmunol.1600643 http://www.jimmunol.org/content/197/4/1460 Lineage-Specific Effector Signatures of Invariant NKT Cells Are Shared amongst T, Innate Lymphoid, and Th Cells You Jeong Lee, Gabriel J. Starrett, Seungeun Thera Lee, Rendong Yang, Christine M. Henzler, Stephen C. Jameson and Kristin A. Hogquist J Immunol cites 41 articles Submit online. Every submission reviewed by practicing scientists ? is published twice each month by Submit copyright permission requests at: http://www.aai.org/About/Publications/JI/copyright.html Receive free email-alerts when new articles cite this article. Sign up at: http://jimmunol.org/alerts http://jimmunol.org/subscription http://www.jimmunol.org/content/suppl/2016/07/06/jimmunol.160064 3.DCSupplemental This article http://www.jimmunol.org/content/197/4/1460.full#ref-list-1 Information about subscribing to The JI No Triage! Fast Publication! Rapid Reviews! 30 days* Why • • • Material References Permissions Email Alerts Subscription Supplementary The Journal of Immunology The American Association of Immunologists, Inc., 1451 Rockville Pike, Suite 650, Rockville, MD 20852 Copyright © 2016 by The American Association of Immunologists, Inc. All rights reserved. Print ISSN: 0022-1767 Online ISSN: 1550-6606. This information is current as of September 26, 2021. The Journal of Immunology Lineage-Specific Effector Signatures of Invariant NKT Cells Are Shared amongst gd T, Innate Lymphoid, and Th Cells You Jeong Lee,* Gabriel J. -

Autocrine IFN Signaling Inducing Profibrotic Fibroblast Responses By
Downloaded from http://www.jimmunol.org/ by guest on September 23, 2021 Inducing is online at: average * The Journal of Immunology , 11 of which you can access for free at: 2013; 191:2956-2966; Prepublished online 16 from submission to initial decision 4 weeks from acceptance to publication August 2013; doi: 10.4049/jimmunol.1300376 http://www.jimmunol.org/content/191/6/2956 A Synthetic TLR3 Ligand Mitigates Profibrotic Fibroblast Responses by Autocrine IFN Signaling Feng Fang, Kohtaro Ooka, Xiaoyong Sun, Ruchi Shah, Swati Bhattacharyya, Jun Wei and John Varga J Immunol cites 49 articles Submit online. Every submission reviewed by practicing scientists ? is published twice each month by Receive free email-alerts when new articles cite this article. Sign up at: http://jimmunol.org/alerts http://jimmunol.org/subscription Submit copyright permission requests at: http://www.aai.org/About/Publications/JI/copyright.html http://www.jimmunol.org/content/suppl/2013/08/20/jimmunol.130037 6.DC1 This article http://www.jimmunol.org/content/191/6/2956.full#ref-list-1 Information about subscribing to The JI No Triage! Fast Publication! Rapid Reviews! 30 days* Why • • • Material References Permissions Email Alerts Subscription Supplementary The Journal of Immunology The American Association of Immunologists, Inc., 1451 Rockville Pike, Suite 650, Rockville, MD 20852 Copyright © 2013 by The American Association of Immunologists, Inc. All rights reserved. Print ISSN: 0022-1767 Online ISSN: 1550-6606. This information is current as of September 23, 2021. The Journal of Immunology A Synthetic TLR3 Ligand Mitigates Profibrotic Fibroblast Responses by Inducing Autocrine IFN Signaling Feng Fang,* Kohtaro Ooka,* Xiaoyong Sun,† Ruchi Shah,* Swati Bhattacharyya,* Jun Wei,* and John Varga* Activation of TLR3 by exogenous microbial ligands or endogenous injury-associated ligands leads to production of type I IFN.