The Role of Matrix Metalloproteinases in Osteoarthritis Pathogenesis An
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Role of Cyclosporine in Gingival Hyperplasia: an in Vitro Study on Gingival Fibroblasts
International Journal of Molecular Sciences Article Role of Cyclosporine in Gingival Hyperplasia: An In Vitro Study on Gingival Fibroblasts 1, , 2, 3 3 Dorina Lauritano * y , Annalisa Palmieri y, Alberta Lucchese , Dario Di Stasio , Giulia Moreo 1 and Francesco Carinci 4 1 Department of Medicine and Surgery, Centre of Neuroscience of Milan, University of Milano-Bicocca, 20126 Milan, Italy; [email protected] 2 Department of Experimental, Diagnostic and Specialty Medicine, University of Bologna, via Belmoro 8, 40126 Bologna, Italy; [email protected] 3 Multidisciplinary Department of Medical and Dental Specialties, University of Campania-Luigi Vanvitelli, 80138 Naples, Italy; [email protected] (A.L.); [email protected] (D.D.S.) 4 Department of Morphology, Surgery and Experimental Medicine, University of Ferrara, 44121 Ferrara, Italy; [email protected] * Correspondence: [email protected]; Tel.: +39-335-679-0163 These authors contributed equally to this work. y Received: 25 November 2019; Accepted: 13 January 2020; Published: 16 January 2020 Abstract: Background: Gingival hyperplasia could occur after the administration of cyclosporine A. Up to 90% of the patients submitted to immunosuppressant drugs have been reported to suffer from this side effect. The role of fibroblasts in gingival hyperplasia has been widely discussed by literature, showing contrasting results. In order to demonstrate the effect of cyclosporine A on the extracellular matrix component of fibroblasts, we investigated the gene expression profile of human fibroblasts after cyclosporine A administration. Materials and methods: Primary gingival fibroblasts were stimulated with 1000 ng/mL cyclosporine A solution for 16 h. Gene expression levels of 57 genes belonging to the “Extracellular Matrix and Adhesion Molecules” pathway were analyzed using real-time PCR in treated cells, compared to untreated cells used as control. -

Inflammation-Mediated Skin Tumorigenesis Induced by Epidermal C-Fos
Downloaded from genesdev.cshlp.org on September 29, 2021 - Published by Cold Spring Harbor Laboratory Press Inflammation-mediated skin tumorigenesis induced by epidermal c-Fos Eva M. Briso,1 Juan Guinea-Viniegra,1 Latifa Bakiri,1 Zbigniew Rogon,2 Peter Petzelbauer,3 Roland Eils,2 Ronald Wolf,4 Mercedes Rinco´ n,5 Peter Angel,6 and Erwin F. Wagner1,7 1BBVA Foundation-Spanish National Cancer Research Center (CNIO) Cancer Cell Biology Program, CNIO, 28029 Madrid, Spain; 2Division of Theoretical Bioinformatics, German Cancer Research Center (DKFZ), 69120 Heidelberg, Germany; 3Skin and Endothelium Research Division (SERD), Department of Dermatology, Medical University of Vienna, A-1090 Vienna, Austria; 4Department of Dermatology and Allergology, Ludwig-Maximilian University, Munich, Germany; 5Division of Immunobiology, Department of Medicine, University of Vermont, 05405 Burlington, Vermont, USA; 6Division of Signal Transduction and Growth Control, DKFZ, DKFZ-Center for Molecular Biology of the University of Heidelberg (ZMBH) Alliance, 69120 Heidelberg, Germany Skin squamous cell carcinomas (SCCs) are the second most prevalent skin cancers. Chronic skin inflammation has been associated with the development of SCCs, but the contribution of skin inflammation to SCC development remains largely unknown. In this study, we demonstrate that inducible expression of c-fos in the epidermis of adult mice is sufficient to promote inflammation-mediated epidermal hyperplasia, leading to the development of preneoplastic lesions. Interestingly, c-Fos transcriptionally controls mmp10 and s100a7a15 expression in keratinocytes, subsequently leading to CD4 T-cell recruitment to the skin, thereby promoting epidermal hyperplasia that is likely induced by CD4 T-cell-derived IL-22. Combining inducible c-fos expression in the epidermis with a single dose of the carcinogen 7,12-dimethylbenz(a)anthracene (DMBA) leads to the development of highly invasive SCCs, which are prevented by using the anti-inflammatory drug sulindac. -

High Serum Levels of Matrix Metalloproteinase-9 and Matrix
Imaging, Diagnosis, Prognosis High Serum Levels of Matrix Metalloproteinase-9 and Matrix Metalloproteinase-1Are Associated with Rapid Progression in Patients with Metastatic Melanoma Johanna Nikkola,1, 3 PiaVihinen,1, 3 Meri-SiskoVuoristo,4 Pirkko Kellokumpu-Lehtinen,4 Veli-Matti Ka« ha« ri,2 and Seppo Pyrho« nen1, 3 Abstract Purpose: Matrixmetalloproteinases (MMP) are proteolytic enzymes that play an important role in various aspects of cancer progression. In the present work, we have studied the prognostic significance of serum levels of gelatinase B (MMP-9), collagenase-1 (MMP-1), and collagenase- 3 (MMP-13) in patients with advanced melanoma. Experimental Design:Total pretreatment serum levels of MMP-9 in 71patients and MMP-1and MMP-13 in 48 patients were determined by an assay system based on ELISA. Total MMP levels were also assessed in eight healthy controls. The active and latent forms of MMPs were defined by usingWestern blot analysis and gelatin zymography. Results: Patients with high serum levels of MMP-9 (z376.6 ng/mL; n = 19) had significantly poorer overall survival (OS) than patients with lower serum MMP-9 levels (n =52;medianOS, 29.1versus 45.2 months; P = 0.033). High MMP-9 levels were also associated with visceral or bone metastasis (P = 0.027), elevated serum alkaline phosphatase level (P = 0.0009), and presence of liver metastases (P =0.032).SerumlevelsofMMP-1andMMP-13didnotcorrelate with OS. MMP-1and MMP-9 were found mainly in latent forms in serum, whereas the majority of MMP-13 in serum was active (48 kDa) form. MMP-13 was found more often in active form in patients (mean, 99% of the total MMP-13 level) than in controls (mean, 84% of the total MMP-13 level; P < 0.0001). -

Discovery and Optimization of Selective Inhibitors of Meprin Α (Part II)
pharmaceuticals Article Discovery and Optimization of Selective Inhibitors of Meprin α (Part II) Chao Wang 1,2, Juan Diez 3, Hajeung Park 1, Christoph Becker-Pauly 4 , Gregg B. Fields 5 , Timothy P. Spicer 1,6, Louis D. Scampavia 1,6, Dmitriy Minond 2,7 and Thomas D. Bannister 1,2,* 1 Department of Molecular Medicine, Scripps Research, Jupiter, FL 33458, USA; [email protected] (C.W.); [email protected] (H.P.); [email protected] (T.P.S.); [email protected] (L.D.S.) 2 Department of Chemistry, Scripps Research, Jupiter, FL 33458, USA; [email protected] 3 Rumbaugh-Goodwin Institute for Cancer Research, Nova Southeastern University, 3321 College Avenue, CCR r.605, Fort Lauderdale, FL 33314, USA; [email protected] 4 The Scripps Research Molecular Screening Center, Scripps Research, Jupiter, FL 33458, USA; [email protected] 5 Unit for Degradomics of the Protease Web, Institute of Biochemistry, University of Kiel, Rudolf-Höber-Str.1, 24118 Kiel, Germany; fi[email protected] 6 Department of Chemistry & Biochemistry and I-HEALTH, Florida Atlantic University, 5353 Parkside Drive, Jupiter, FL 33458, USA 7 Dr. Kiran C. Patel College of Allopathic Medicine, Nova Southeastern University, 3301 College Avenue, Fort Lauderdale, FL 33314, USA * Correspondence: [email protected] Abstract: Meprin α is a zinc metalloproteinase (metzincin) that has been implicated in multiple diseases, including fibrosis and cancers. It has proven difficult to find small molecules that are capable Citation: Wang, C.; Diez, J.; Park, H.; of selectively inhibiting meprin α, or its close relative meprin β, over numerous other metzincins Becker-Pauly, C.; Fields, G.B.; Spicer, which, if inhibited, would elicit unwanted effects. -

2335 Roles of Molecules Involved in Epithelial/Mesenchymal Transition
[Frontiers in Bioscience 13, 2335-2355, January 1, 2008] Roles of molecules involved in epithelial/mesenchymal transition during angiogenesis Giulio Ghersi Dipartimento di Biologia Cellulare e dello Sviluppo, Universita di Palermo, Italy TABLE OF CONTENTS 1. Abstract 2. Introduction 3. Extracellular matrix 3.1. ECM and integrins 3.2. Basal lamina components 4. Cadherins. 4.1. Cadherins in angiogenesis 5. Integrins. 5.1. Integrins in angiogenesis 6. Focal adhesion molecules 7. Proteolytic enzymes 7.1. Proteolytic enzymes inhibitors 7.2. Proteolytic enzymes in angiogenesis 8. Perspective 9. Acknowledgements 10. References 1.ABSTRACT 2. INTRODUCTION Formation of vessels requires “epithelial- Growth of new blood vessels (angiogenesis) mesenchymal” transition of endothelial cells, with several plays a key role in several physiological processes, such modifications at the level of endothelial cell plasma as vascular remodeling during embryogenesis and membranes. These processes are associated with wound healing tissue repair in the adult; as well as redistribution of cell-cell and cell-substrate adhesion pathological processes, including rheumatoid arthritis, molecules, cross talk between external ECM and internal diabetic retinopathy, psoriasis, hemangiomas, and cytoskeleton through focal adhesion molecules and the cancer (1). Vessel formation entails the “epithelial- expression of several proteolytic enzymes, including matrix mesenchymal” transition of endothelial cells (ECs) “in metalloproteases and serine proteases. These enzymes with vivo”; a similar phenotypic exchange can be induced “in their degradative action on ECM components, generate vitro” by growing ECs to low cell density, or in “wound molecules acting as activators and/or inhibitors of healing” experiments or perturbing cell adhesion and angiogenesis. The purpose of this review is to provide an associated molecule functions. -

Transmembrane/Cytoplasmic, Rather Than Catalytic, Domains of Mmp14
RESEARCH ARTICLE 343 Development 140, 343-352 (2013) doi:10.1242/dev.084236 © 2013. Published by The Company of Biologists Ltd Transmembrane/cytoplasmic, rather than catalytic, domains of Mmp14 signal to MAPK activation and mammary branching morphogenesis via binding to integrin 1 Hidetoshi Mori1,*, Alvin T. Lo1, Jamie L. Inman1, Jordi Alcaraz1,2, Cyrus M. Ghajar1, Joni D. Mott1, Celeste M. Nelson1,3, Connie S. Chen1, Hui Zhang1, Jamie L. Bascom1, Motoharu Seiki4 and Mina J. Bissell1,* SUMMARY Epithelial cell invasion through the extracellular matrix (ECM) is a crucial step in branching morphogenesis. The mechanisms by which the mammary epithelium integrates cues from the ECM with intracellular signaling in order to coordinate invasion through the stroma to make the mammary tree are poorly understood. Because the cell membrane-bound matrix metalloproteinase Mmp14 is known to play a key role in cancer cell invasion, we hypothesized that it could also be centrally involved in integrating signals for mammary epithelial cells (MECs) to navigate the collagen 1 (CL-1)-rich stroma of the mammary gland. Expression studies in nulliparous mice that carry a NLS-lacZ transgene downstream of the Mmp14 promoter revealed that Mmp14 is expressed in MECs at the tips of the branches. Using both mammary organoids and 3D organotypic cultures, we show that MMP activity is necessary for invasion through dense CL-1 (3 mg/ml) gels, but dispensable for MEC branching in sparse CL-1 (1 mg/ml) gels. Surprisingly, however, Mmp14 without its catalytic activity was still necessary for branching. Silencing Mmp14 prevented cell invasion through CL-1 and disrupted branching altogether; it also reduced integrin 1 (Itgb1) levels and attenuated MAPK signaling, disrupting Itgb1- dependent invasion/branching within CL-1 gels. -

Smooth Muscle-Specific MMP17 (MT4-MMP) Defines the Intestinal ECM Niche 2 3 Mara Martín-Alonso1*, Håvard T
bioRxiv preprint doi: https://doi.org/10.1101/2020.06.18.147769; this version posted June 18, 2020. The copyright holder for this preprint (which was not certified by peer review) is the author/funder. All rights reserved. No reuse allowed without permission. 1 Smooth muscle-specific MMP17 (MT4-MMP) defines the intestinal ECM niche 2 3 Mara Martín-Alonso1*, Håvard T. Lindholm1,# , Sharif Iqbal2,3,#, Pia Vornewald1#, Sigrid Hoel1, 4 Mirjam J. Damen4, A.F.Maarten Altelaar4, Pekka Katajisto2,3,5, Alicia G. Arroyo6,7, Menno J. 5 Oudhoff1* 6 7 1CEMIR – Centre of Molecular Inflammation Research, Department of Clinical and Molecular 8 Medicine, NTNU – Norwegian University of Science and Technology, 7491 Trondheim, 9 Norway 10 2Institute of Biotechnology, HiLIFE, University of Helsinki, Finland 11 3Molecular and Integrative Bioscience Research Programme, Faculty of Biological and 12 Environmental Sciences, University of Helsinki, Helsinki, Finland 13 4Biomolecular Mass Spectrometry and Proteomics, Utrecht University, Utrecht, The 14 Netherlands 15 5Department of Biosciences and Nutrition, Karolinska Institutet, Stockholm, Sweden 16 6Centro de Investigaciones Biológicas Margarita Salas (CIB-CSIC), Madrid, Spain 17 7Vascular Pathophysiology Area, Centro Nacional de Investigaciones Cardiovasculares 18 (CNIC), Madrid, Spain.CNIC, Madrid, Spain 19 20 #These authors contributed equally to this work 21 *corresponding authors, e-mail: [email protected], [email protected] 22 bioRxiv preprint doi: https://doi.org/10.1101/2020.06.18.147769; this version posted June 18, 2020. The copyright holder for this preprint (which was not certified by peer review) is the author/funder. All rights reserved. No reuse allowed without permission. -

TACI:Fc Scavenging B Cell Activating Factor (BAFF) Alleviates Ovalbumin-Induced Bronchial Asthma in Mice
EXPERIMENTAL and MOLECULAR MEDICINE, Vol. 39, No. 3, 343-352, June 2007 TACI:Fc scavenging B cell activating factor (BAFF) alleviates ovalbumin-induced bronchial asthma in mice 1,2,3 2 Eun-Yi Moon and Sook-Kyung Ryu the percentage of non-lymphoid cells and no changes were detected in lymphoid cell population. 1 Department of Bioscience and Biotechnology Hypodiploid cell formation in BALF was decreased Sejong University by OVA-challenge but it was recovered by TACI:Fc Seoul 143-747, Korea treatment. Collectively, data suggest that asthmatic 2 Laboratory of Human Genomics symptom could be alleviated by scavenging BAFF Korea Research Institute of Bioscience and Biotechnology (KRIBB) and then BAFF could be a novel target for the Daejeon 305-806, Korea develpoment of anti-asthmatic agents. 3 Corresponding author: Tel, 82-2-3408-3768; Fax, 82-2-466-8768; E-mail, [email protected] Keywords: asthma; B-cell activating factor; ovalbu- and [email protected] min; transmembrane activator and CAML interactor protein Accepted 28 March 2007 Introduction Abbreviations: BAFF, B cell activating factor belonging to TNF- family; BALF, bronchoalveolar lavage fluid; OVA, ovalbumin; PAS, Mature B cell generation and maintenance are regu- periodic acid-Schiff; Prx, peroxiredoxin; TACI, transmembrane lated by B-cell activating factor (BAFF). BAFF is pro- activator and calcium modulator and cyclophilin ligand interactor duced by macrophages or dendritic cells upon stim- ulation with LPS or IFN- . BAFF belongs to the TNF family. Its biological role is mediated by the specific Abstract receptors, B-cell maturation antigen (BCMA), trans- membrane activator and calcium modulator and cy- Asthma was induced by the sensitization and chal- clophilin ligand interactor (TACI) and BAFF receptor, lenge with ovalbumin (OVA) in mice. -

Nuclear Matrix Metalloproteinases: Functions Resemble the Evolution from the Intracellular to the Extracellular Compartment
OPEN Citation: Cell Death Discovery (2017) 3, 17036; doi:10.1038/cddiscovery.2017.36 Official journal of the Cell Death Differentiation Association www.nature.com/cddiscovery REVIEW Nuclear matrix metalloproteinases: functions resemble the evolution from the intracellular to the extracellular compartment Yingqiu Xie1,2,5, Aidana Mustafa1,5, Adina Yerzhan1,5, Dalmira Merzhakupova1, Perizat Yerlan1, Askarbek N Orakov1, Xiao Wang3, Yi Huang4 and Lixia Miao2 Matrix metalloproteinase (MMP) is defined as an endopeptidase in the extracellular matrix (ECM), which plays essential roles in physiological processes such as organogenesis, wound healing, angiogenesis, apoptosis and motility. MMPs are produced and assembled in the cytoplasm as proenzymes with a cytoplasmic domain and require extracellular activation. MMPs can degrade receptors, extracellular matrix proteins, PARPs and release apoptotic substances. MMPs have been found in the cytosol, organelles and extracellular compartments and recently many types of MMPs have been found in the nucleus. However, the mechanisms and roles of MMPs inside the cell nucleus are still poorly understood. Here we summarized the nuclear localization mechanisms of MMPs and their functions in the nucleus such as apoptosis, tissue remodeling upon injury and cancer progression. Most importantly, we found that nuclear MMPs have evolved to translocate to membrane and target ECM possibly through evolution of nuclear localization signal (NLS), natural selection and anti-apoptotic survival. Thus, the knowledge about the evolution and regulation of nuclear MMPs appears to be essential in understanding a variety of cellular processes along with the development of MMP-targeted therapeutic drugs against the progression of certain diseases. Cell Death Discovery (2017) 3, 17036; doi:10.1038/cddiscovery.2017.36; published online 14 August 2017 KEY FACTS MMP-10, MMP-13 and MMP-14. -

Aggrecan (A1960)
Aggrecan from bovine articular cartilage Catalog Number A1960 Storage Temperature –20 °C Product Description References Aggrecan is the major structural proteoglycan found in 1. Hardingham, T.E., and Muir, H., Biochim. Biophys. the extracellular matrix of cartilage. It has a molecular Acta, 279, 401-405 (1972). mass >2,500 kDa. The core protein (210–250 kDa) has 2. Hedlund, H., et al., Association of the aggrecan 100–150 glycosaminoglycan (GAG) chains attached to keratan sulfate-rich region with collagen in bovine it. The majority of the GAG chains are chondroitin/ articular cartilage. J. Biol. Chem., 274, 5777-5781 dermatan sulfate with the remainder being keratan (1999). sulfate. This structural molecule produces a rigid, 3. Cao, L., and Yang, B.B., Chondrocyte apoptosis reversibly deformable gel that resists compression. It induced by aggrecan G1 domain as a result of combines with hyaluronic acid to form very large decreased cell adhesion. Exp. Cell Res., 246, 527- macromolecular complexes. Addition of small amounts 537 (1999). (0.1–2% w/w) of hyaluronic acid to a solution of 4. Bolton, M.C., et al., Age-related changes in the aggrecan (2 mg/ml) results in the formation of a synthesis of link protein and aggrecan in human complex with an increased hydrodynamic volume and articular cartilage: implications for aggregate in a significant increase (30–40%) in the relative stability. Biochem. J., 337, 77-82 (1999). viscosity of the solution. 5. Arner, E.C., et al., Generation and Characterization of Aggrecanase. A soluble, cartilage-derived Aggrecan is a critical component for cartilage structure aggrecan-degrading activity. -

On and Polymorphisms in Q Fever
Matrix metalloproteinase expression, produc3on and polymorphisms in Q fever Anne F.M. Jansen1,2, Teske Schoffelen1,2, Julien Textoris3, Jean Louis Mege3, Chantal P. Bleeker-Rovers1,2, Esther van de Vosse4, Hendrik Jan Roest5, Marcel van Deuren1,2 1. Department of Internal Medicine, Division of Experimental Medicine, Radboud university medical center, Nijmegen, The Netherlands 2. Radboud Expert Centre for Q fever, Radboud university medical center, Nijmegen, the Netherlands, 3. URMITE, CNRS UMR 7278, IRD 198, INSERM 1095 Aix-Marseille University, Marseille, France 4. Department of Infec3ous Diseases, Leiden University Medical Center, Leiden, The Netherlands 5. Department of Bacteriology and TSEs, Central Veterinary Instute, part of Wageningen UR, Lelystad, the Netherlands Background C. burnei induces MMP-1 and MMP-9 produc3on in PBMCs Chronic Q fever is a life threatening condi3on caused by the Gram-negave bacterium Coxiella burnei, manifes3ng as an infec3on of aneurysms, aor3c prosthesis or heart valves. Matrix metalloproteinases (MMPs) are proteoly3c enzymes that cleave extracellular matrix and are implicated in the pathology of aneurysms and endocardi3s. Currently, the contribu3on of MMPs to the pathogenesis of chronic Q fever is unknown. Methods We inves3gated the C. burnei specific gene expression of MMPs in PBMCs and protein produc3on by ELISA in chronic Q fever paents (n=6, n=10, respec3vely), cardiovascular paents with a history of Q fever (n=10) and healthy controls (n=4, n=10, respec3vely), in some experiments, the controls had vascular disease (n=10). Circulang MMP levels were assessed with Luminex technology and these groups were also genotyped for 20 SNPs in MMP and Tissue Inhibitor of MMP (TIMP) genes. -
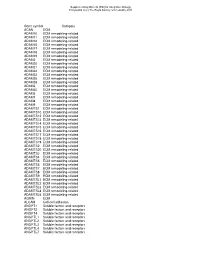
Gene Symbol Category ACAN ECM ADAM10 ECM Remodeling-Related ADAM11 ECM Remodeling-Related ADAM12 ECM Remodeling-Related ADAM15 E
Supplementary Material (ESI) for Integrative Biology This journal is (c) The Royal Society of Chemistry 2010 Gene symbol Category ACAN ECM ADAM10 ECM remodeling-related ADAM11 ECM remodeling-related ADAM12 ECM remodeling-related ADAM15 ECM remodeling-related ADAM17 ECM remodeling-related ADAM18 ECM remodeling-related ADAM19 ECM remodeling-related ADAM2 ECM remodeling-related ADAM20 ECM remodeling-related ADAM21 ECM remodeling-related ADAM22 ECM remodeling-related ADAM23 ECM remodeling-related ADAM28 ECM remodeling-related ADAM29 ECM remodeling-related ADAM3 ECM remodeling-related ADAM30 ECM remodeling-related ADAM5 ECM remodeling-related ADAM7 ECM remodeling-related ADAM8 ECM remodeling-related ADAM9 ECM remodeling-related ADAMTS1 ECM remodeling-related ADAMTS10 ECM remodeling-related ADAMTS12 ECM remodeling-related ADAMTS13 ECM remodeling-related ADAMTS14 ECM remodeling-related ADAMTS15 ECM remodeling-related ADAMTS16 ECM remodeling-related ADAMTS17 ECM remodeling-related ADAMTS18 ECM remodeling-related ADAMTS19 ECM remodeling-related ADAMTS2 ECM remodeling-related ADAMTS20 ECM remodeling-related ADAMTS3 ECM remodeling-related ADAMTS4 ECM remodeling-related ADAMTS5 ECM remodeling-related ADAMTS6 ECM remodeling-related ADAMTS7 ECM remodeling-related ADAMTS8 ECM remodeling-related ADAMTS9 ECM remodeling-related ADAMTSL1 ECM remodeling-related ADAMTSL2 ECM remodeling-related ADAMTSL3 ECM remodeling-related ADAMTSL4 ECM remodeling-related ADAMTSL5 ECM remodeling-related AGRIN ECM ALCAM Cell-cell adhesion ANGPT1 Soluble factors and receptors