ISSN 1553-9768 Summer 2008 Volume 8, Edition 3
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Managing the Human Weapon System: a Vision for an Air Force Human-Performance Doctrine
Calhoun: The NPS Institutional Archive DSpace Repository Faculty and Researchers Faculty and Researchers Collection 2009 Managing the Human Weapon System: A Vision for an Air Force Human-Performance Doctrine Tvaryanas, A.P. Tvaryanas, A.P., Brown, L., and Miller, N.L. "Managing the Human Weapon System: A Vision for an Air Force Human-Performance Doctrine", Air & Space Power Journal, pp. 34-41, Summer 2009. http://hdl.handle.net/10945/36508 Downloaded from NPS Archive: Calhoun In air combat, “the merge” occurs when opposing aircraft meet and pass each other. Then they usually “mix it up.” In a similar spirit, Air and Space Power Journal’s “Merge” articles present contending ideas. Readers are free to join the intellectual battlespace. Please send comments to [email protected] or [email protected]. Managing the Human Weapon System A Vision for an Air Force Human-Performance Doctrine LT COL ANTHONY P. TVARYANAS, USAF, MC, SFS COL LEX BROWN, USAF, MC, SFS NITA L. MILLER, PHD* The basic planning, development, organization and training of the Air Force must be well rounded, covering every modern means of waging air war. The Air Force doctrines likewise must be !exible at all times and entirely uninhibited by tradition. —Gen Henry H. “Hap” Arnold N A RECENT paper on America’s Air special operations forces’ declaration that Force, Gen T. Michael Moseley asserted “humans are more important than hardware” that we are at a strategic crossroads as a in asymmetric warfare.2 Consistent with this consequence of global dynamics and view, in January 2004, the deputy secretary of Ishifts in the character of future warfare; he defense directed the Joint Staff to “develop also noted that “today’s con!uence of global the next generation of . -
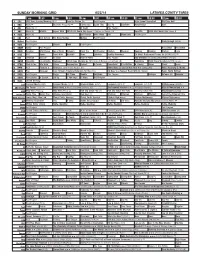
Sunday Morning Grid 6/22/14 Latimes.Com/Tv Times
SUNDAY MORNING GRID 6/22/14 LATIMES.COM/TV TIMES 7 am 7:30 8 am 8:30 9 am 9:30 10 am 10:30 11 am 11:30 12 pm 12:30 2 CBS CBS News Sunday Morning (N) Å Face the Nation (N) Paid Program High School Basketball PGA Tour Golf 4 NBC News Å Meet the Press (N) Å Conference Justin Time Tree Fu LazyTown Auto Racing Golf 5 CW News (N) Å In Touch Paid Program 7 ABC News (N) Wildlife Exped. Wild 2014 FIFA World Cup Group H Belgium vs. Russia. (N) SportCtr 2014 FIFA World Cup: Group H 9 KCAL News (N) Joel Osteen Mike Webb Paid Woodlands Paid Program 11 FOX Paid Joel Osteen Fox News Sunday Midday Paid Program 13 MyNet Paid Program Crazy Enough (2012) 18 KSCI Paid Program Church Faith Paid Program 22 KWHY Como Paid Program RescueBot RescueBot 24 KVCR Painting Wild Places Joy of Paint Wyland’s Paint This Oil Painting Kitchen Mexican Cooking Cooking Kitchen Lidia 28 KCET Hi-5 Space Travel-Kids Biz Kid$ News LinkAsia Healthy Hormones Ed Slott’s Retirement Rescue for 2014! (TVG) Å 30 ION Jeremiah Youssef In Touch Hour of Power Paid Program Into the Blue ›› (2005) Paul Walker. (PG-13) 34 KMEX Conexión En contacto Backyard 2014 Copa Mundial de FIFA Grupo H Bélgica contra Rusia. (N) República 2014 Copa Mundial de FIFA: Grupo H 40 KTBN Walk in the Win Walk Prince Redemption Harvest In Touch PowerPoint It Is Written B. Conley Super Christ Jesse 46 KFTR Paid Fórmula 1 Fórmula 1 Gran Premio Austria. -

New Equipping Strategies for Combat Support Hospitals
ARROYO CENTER and RAND HEALTH Center for Military Health Policy Research THE ARTS This PDF document was made available from www.rand.org as CHILD POLICY a public service of the RAND Corporation. CIVIL JUSTICE EDUCATION Jump down to document ENERGY AND ENVIRONMENT 6 HEALTH AND HEALTH CARE INTERNATIONAL AFFAIRS The RAND Corporation is a nonprofit institution that NATIONAL SECURITY POPULATION AND AGING helps improve policy and decisionmaking through PUBLIC SAFETY research and analysis. SCIENCE AND TECHNOLOGY SUBSTANCE ABUSE TERRORISM AND HOMELAND SECURITY Support RAND TRANSPORTATION AND INFRASTRUCTURE Purchase this document WORKFORCE AND WORKPLACE Browse Books & Publications Make a charitable contribution For More Information Visit RAND at www.rand.org Explore the RAND Arroyo Center RAND Health View document details Limited Electronic Distribution Rights This document and trademark(s) contained herein are protected by law as indicated in a notice appearing later in this work. This electronic representation of RAND intellectual property is provided for non-commercial use only. Unauthorized posting of RAND PDFs to a non-RAND Web site is prohibited. RAND PDFs are protected under copyright law. Permission is required from RAND to reproduce, or reuse in another form, any of our research documents for commercial use. For information on reprint and linking permissions, please see RAND Permissions. This product is part of the RAND Corporation monograph series. RAND monographs present major research findings that address the challenges facing the public and private sectors. All RAND monographs undergo rigorous peer review to ensure high standards for research quality and objectivity. New Equipping Strategies for Combat Support Hospitals Matthew W. -

Medical Professionals in Remote and Extreme Environments: a Mission to Mars
Title: Medical Professionals in Remote and Extreme Environments: A Mission to Mars Authors: Hsu, Michael M., Coffey, Christanne H., Witucki, Peter and Sloane, Christian. Abstract: To give a representative overview of medical professionals working in today’s remote and extreme environments, we consider the following teams and organizations: • Expeditions on 8000m peaks led by accredited guides of the American Mountain Guides Association (AMGA) or International Federation of Mountain Guides Association (IFMGA) • Everest Base Camp Medical Clinic (Everest ER) in Nepal • US Antarctic Program (USAP) • Medical Departments aboard US Navy ships and submarines • US Special Operations Command (SOCOM) Corpsmen and Medics • US Navy Diving Medical Officers • Crew Medical Officers (CMO’s) aboard the International Space Station After reviewing the practice environments and medical training of the various teams, we consider the medical qualifications of a hypothetical future team embarking on a mission to a particularly remote and extreme environment, a human spaceflight mission to the surface of Mars. Introduction: This article explores the qualifications and training of current practitioners of medicine operating in remote and extreme environments. Remote environments have limited access to rescue and hospital care. Extreme environments have exposure to temperature and pressure extremes, radiation, as well as exposure to significant mechanical hazards, including from enemy action during military operations. Several environments combine these descriptions. A prospective human spaceflight to Mars would operate within remote and extreme environments through the entirety of the mission. As observed by Dr. HD Backer, MD, “Wilderness medicine not only overlaps with sports medicine, but also emergency medicine, military, occupational, and travel medicine and international health” and “It shares with military medicine an intense interest in environmental stresses and hazards, field management and mobile response” (Backer, 1995). -

Swordplay Through the Ages Daniel David Harty Worcester Polytechnic Institute
Worcester Polytechnic Institute Digital WPI Interactive Qualifying Projects (All Years) Interactive Qualifying Projects April 2008 Swordplay Through The Ages Daniel David Harty Worcester Polytechnic Institute Drew Sansevero Worcester Polytechnic Institute Jordan H. Bentley Worcester Polytechnic Institute Timothy J. Mulhern Worcester Polytechnic Institute Follow this and additional works at: https://digitalcommons.wpi.edu/iqp-all Repository Citation Harty, D. D., Sansevero, D., Bentley, J. H., & Mulhern, T. J. (2008). Swordplay Through The Ages. Retrieved from https://digitalcommons.wpi.edu/iqp-all/3117 This Unrestricted is brought to you for free and open access by the Interactive Qualifying Projects at Digital WPI. It has been accepted for inclusion in Interactive Qualifying Projects (All Years) by an authorized administrator of Digital WPI. For more information, please contact [email protected]. IQP 48-JLS-0059 SWORDPLAY THROUGH THE AGES Interactive Qualifying Project Proposal Submitted to the Faculty of the WORCESTER POLYTECHNIC INSTITUTE in partial fulfillment of the requirements for graduation by __ __________ ______ _ _________ Jordan Bentley Daniel Harty _____ ________ ____ ________ Timothy Mulhern Drew Sansevero Date: 5/2/2008 _______________________________ Professor Jeffrey L. Forgeng. Major Advisor Keywords: 1. Swordplay 2. Historical Documentary Video 3. Higgins Armory 1 Contents _______________________________ ........................................................................................0 Abstract: .....................................................................................................................................2 -

Adrian Maher
ADRIAN MAHER WRITER/DIRECTOR/SUPERVISING PRODUCER Los Angeles, CA Cell: (310) 922-3080 Email: [email protected] Website: www.maherproductions.com ____________________________________________________________________________________________________________ PROFESSIONAL EXPERIENCE – REALITY AND DOCUMENTARY TELEVISION More than two decades of experience as a writer/director of documentary television programs, print journalist, on-air reporter, book author and private investigator. Strong writing, directing, producing, voiceover, investigative, digital media, and managerial skills. UNSUNG HOLLYWOOD: HARLEM GLOBETROTTERS: (TV ONE NETWORK) (ASmith and Company) Wrote, Directed and Produced a one -hour episode on the history of the Harlem Globetrotters from their founding in Chicago in 1927 to their present-day status as one of the most recognizable sports brands in the world. SPLIT-SECOND DECISION: (MSNBC) (The Gurin Company) Wrote, Directed and Produced three one-hour documentaries about people caught in catastrophic situations and the instant decisions they make to survive. UNSUNG HOLLYWOOD: RICHARD ROUNDTREE: (TV ONE NETWORK) (ASmith and Company) Wrote, and Produced a one-hour episode/biography on America’s first black-action movie star – Richard Roundtree – (star of “Shaft”) and the “blaxploitation” era in Hollywood films. TRIGGERS: WEAPONS THAT CHANGED THE WORLD (MILITARY CHANNEL) (Morningstar Entertainment) Wrote and Produced several episodes on history’s most fearsome weapons including “Gatling Guns,” “Tanks” and “Light Machine Guns.” -

SFU Thesis Template Files
“To Fight the Battles We Never Could”: The Militarization of Marvel’s Cinematic Superheroes by Brett Pardy B.A., The University of the Fraser Valley, 2013 Thesis Submitted in Partial Fulfillment of the Requirements for the Degree of Master of Arts in the School of Communication Faculty of Communication, Art, and Technology Brett Pardy 2016 SIMON FRASER UNIVERSITY Summer 2016 Approval Name: Brett Pardy Degree: Master of Arts Title: “To Fight the Battles We Never Could”: The Militarization of Marvel’s Cinematic Superheroes Examining Committee: Chair: Frederik Lesage Assistant Professor Zoë Druick Senior Supervisor Associate Professor Adel Iskander Supervisor Assistant Professor Michael Ma External Examiner Faculty Member Department of Criminology Kwantlen Polytechnic University Date Defended/Approved: June 16, 2016 ii Abstract The Marvel comics film adaptations have been some of the most successful Hollywood products of the post 9/11 period, bringing formerly obscure cultural texts into the mainstream. Through an analysis of the adaptation process of Marvel Entertainment’s superhero franchise from comics to film, I argue that a hegemonic American model of militarization has been used by Hollywood as a discursive formation with which to transform niche properties into mass market products. I consider the locations of narrative ambiguities in two key comics texts, The Ultimates (2002-2007) and The New Avengers (2005-2012), as well as in the film The Avengers (2012), and demonstrate the significant reorientation of the film franchise towards the American military’s “War on Terror”. While Marvel had attempted to produce film adaptations for decades, only under the new “militainment” discursive formation was it finally successful. -

State, Foreign Operations, and Related Programs Appropriations for Fiscal Year 2018
STATE, FOREIGN OPERATIONS, AND RELATED PROGRAMS APPROPRIATIONS FOR FISCAL YEAR 2018 TUESDAY, MAY 9, 2017 U.S. SENATE, SUBCOMMITTEE OF THE COMMITTEE ON APPROPRIATIONS, Washington, DC. The subcommittee met at 2:30 p.m., in room SD–192, Dirksen Senate Office Building, Hon. Lindsey Graham (chairman) pre- siding. Present: Senators Graham, Moran, Boozman, Daines, Leahy, Durbin, Shaheen, Coons, Murphy and Van Hollen. UNITED STATES DEMOCRACY ASSISTANCE STATEMENTS OF: HON. MADELEINE ALBRIGHT, CHAIRMAN OF THE BOARD, THE NA- TIONAL DEMOCRATIC INSTITUTE HON. STEPHEN HADLEY, CHAIRMAN OF THE BOARD, THE UNITED STATES INSTITUTE OF PEACE HON. VIN WEBER, CO-VICE CHAIRMAN OF THE BOARD, THE NA- TIONAL ENDOWMENT FOR DEMOCRACY HON. JAMES KOLBE, VICE CHAIRMAN OF THE BOARD, THE INTER- NATIONAL REPUBLICAN INSTITUTE TESTIMONY FROM DEMOCRACY PROGRAM BENEFICIARIES OUTSIDE WITNESS TESTIMONY SUBMITTED SUBSEQUENT TO THE HEARING OPENING STATEMENT OF SENATOR LINDSEY GRAHAM Senator GRAHAM. Thank you all. The subcommittee will come to order. Today, our hearing is on United States Democracy Assist- ance. I would like to welcome our witnesses who deserve long, glowing introductions—but you’re not going to get one because we got to get on one with the hearing. We’ve got Madeleine Albright, Chairman of the Board of the Na- tional Democratic Institute and former Secretary of State. Wel- come, Ms. Albright. James Kolbe, Vice-Chairman of the Board of the International Republican Institute. Jim, welcome. Vin Weber, Co-Vice Chairman of the Board of the National En- dowment for Democracy, all around good guy, Republican type. Stephen Hadley, Chairman of the Board of the United States In- stitute of Peace. -
Hypersonic Hyperstitions
HYPERSONIC HYPERSTITIONS Šum #11 HYPERSONIC HYPERSTITIONS Šum #11 HYPERSONIC HYPERSTITIONS Šum #11 Šum #11 HYPERSONIC HYPERSTITIONS There used to be supersonics and superstitions. Then hyper came along. Marko Peljhan invited Šum journal to produce a special issue that would accompany his exhibition Here we go again… SYSTEM 317 in the Slovenian Pavilion at the Venice Biennale. The invitation included, among a lot of referential vectors, this short description: “The exhibition will feature a full-scale model of a hypersonic aircraft system and will appropriate, combine and hack actual US, Russian and Chinese blueprints. The cockpit will be done in the style of a West Coast lowrider … how to light a match and keep it lit during a hurricane.” Šum in turn approached theory-fiction and hard sci-fi, that is, mobilised their agents, to provide overlaps with Peljhan’s exhibition and his work in general. War. Evolution. Tech. Escape/Exit. The Arctic. Conversion/Convergence. Transpiercement. Surrationality. Shadow-subsuming. Intelligent Battlespace. UGO. Godspeed. 10.851735 1447 1448 10.851735 1451 SURRATIONAL FUGITIVES LUCIANA PARISI 1467 ETERNAL PHENOTYPE MIROSLAV GRIŠKO 1499 AN EXEGETICAL INCURSION OF THE EMERGENT “INTELLIGENT BATTLESPACE” MANABRATA GUHA 1531 CAPITAL, WAR AND LOVE PRIMOŽ KRAŠOVEC 1563 THE WISDOM OF CROWDS PETER WATTS 1595 DIRECTORATE OF CELESTIAL SURVEILLANCE, 1665 ANDREJ TOMAŽIN 1627 UNIDENTIFIED GLIDING OBJECT: THE DAY THE EARTH WAS UNMOORED REZA NEGARESTANI Appendix: 1659 YAMAL EVENTS REPORT 2071 EDMUND BERGER, KEVIN ROGAN 10.851735 1449 1450 10.851735 Surrational Fugitives LUCIANA PARISI 10.851735 1451 SURRATIONAL FUGITIVES 1452 10.851735 In an attempt to contain the human exodus from planet earth, today at 09:09 am, the Planetary Security Council has ordered a shutdown of celestial borders: gateways of hypersonic vessels that pierce the terrestrial atmosphere and fly 9 million light years away from planetary existence. -

Contextualising Legal Reviews for Autonomous Weapon Systems
Missing Man: Contextualising Legal Reviews for Autonomous Weapon Systems DISSERTATION of the University of St. Gallen, School of Management, Economics, Law, Social Sciences and International Affairs to obtain the title of Doctor of Philosophy in Law submitted by Fredrik von Bothmer from Germany Approved on the application of Prof. Dr. Thomas Burri and Prof. Dirk Lehmkuhl, PhD Dissertation no. 4804 Difo-Druck GmbH, Bamberg 2018 The University of St. Gallen, School of Management, Economics, Law, Social Sciences and International Affairs hereby consents to the printing of the present dissertation, without hereby expressing any opinion on the views herein expressed. St. Gallen, May 22, 2018 The President: Prof. Dr. Thomas Bieger II Table of Contents I. Introduction: Key Categories and Terminology ............................................. 7 A. Just another New Emerging Weapon Technology? ................................... 12 B. Terminology and Definition ....................................................................... 18 II. Legal Challenges posed by AWS: IHL and Responsibility .......................... 27 A. AWS as Means and Methods of Warfare ................................................... 33 B. Illegality of AWS per se .............................................................................. 34 1. Basic rules for inherent illegality of weapon systems ............................ 34 a) Indiscriminate weapon by nature ........................................................ 34 b) Unnecessary suffering or superfluous injury -

The Value of Live Tissue Training for Combat Casualty Care: a Survey of Canadian Combat Medics with Battlefield Experience in Afghanistan
CAN UNCLASSIFIED The Value of Live Tissue Training for Combat Casualty Care: A Survey of Canadian Combat Medics With Battlefield Experience in Afghanistan Michael Kim * Ian Torrie † Robert Poisson ‡ Nicholas Withers ‡ Stephen Bjarnason § Luis Teodoro DaLuz * Dylan Pannell *‡ Andrew Beckett ‡∥ Homer C. Tien *‡ * Tory Regional Trauma Centre, Sunnybrook Health Sciences Centre, Toronto † Embassy of Canada, 501 Pennsylvania Avenue NW, Washington, DC ‡ Canadian Forces Health Services Group, Ottawa § Defence Research Development Canada – Suffield Research Centre ∥ Montreal General Hospital, Montreal External Publisher: Association of Military Surgeons of the United States (AMSUS) MILITARY MEDICINE, 182, 9/10:e1834, 2017 doi: 10.7205/MILMED-D-16-00271 Date of Publication from Ext Publisher: Sep/Oct 2017 Defence Research and Development Canada External Literature (P) DRDC-RDDC-2018-P001 February 2018 CAN UNCLASSIFIED CAN UNCLASSIFIED IMPORTANT INFORMATIVE STATEMENTS Disclaimer: This document is not published by the Editorial Office of Defence Research and Development Canada, an agency of the Department of National Defence of Canada, but is to be catalogued in the Canadian Defence Information System (CANDIS), the national repository for Defence S&T documents. Her Majesty the Queen in Right of Canada (Department of National Defence) makes no representations or warranties, expressed or implied, of any kind whatsoever, and assumes no liability for the accuracy, reliability, completeness, currency or usefulness of any information, product, process or material included in this document. Nothing in this document should be interpreted as an endorsement for the specific use of any tool, technique or process examined in it. Any reliance on, or use of, any information, product, process or material included in this document is at the sole risk of the person so using it or relying on it. -

The Crucible of Military Medical Ethics
Medical Ethics on the Battlefield: The Crucible of Military Medical Ethics MILITARY MEDICAL ETHICS VOLUME 2 SECTION IV: MEDICAL ETHICS IN THE MILITARY Section Editor: THOMAS E. BEAM, MD Formerly Director, Borden Institute Formerly, Medical Ethics Consultant to The Surgeon General, United States Army Robert Benney Shock Tent circa World War II Art: Courtesy of Army Art Collection, US Army Center of Military History, Washington, DC. 367 Military Medical Ethics, Volume 2 368 Medical Ethics on the Battlefield: The Crucible of Military Medical Ethics Chapter 13 MEDICAL ETHICS ON THE BATTLEFIELD: THE CRUCIBLE OF MILITARY MEDICAL ETHICS THOMAS E. BEAM, MD* INTRODUCTION RETURN TO DUTY CONSIDERATIONS IN A THEATER OF OPERATIONS Getting Minimally Wounded Soldiers Back to Duty Combat Stress Disorder “Preserve the Fighting Strength” Informed Consent Beneficence for the Soldier in Combat Enforced Treatment for Individual Soldiers BATTLEFIELD TRIAGE The Concept of Triage Establishing and Maintaining Prioritization of Treatment Models of Triage Examining the Extreme Conditions Model EUTHANASIA ON THE BATTLEFIELD Understanding the Dynamics of the Battlefield: The Swann Scenario A Brief History of Battlefield Euthanasia A Civilian Example From a “Battlefield” Setting Available Courses of Action: The Swann Scenario Ethical Analysis of Options PARTICIPATION IN INTERROGATION OF PRISONERS OF WAR Restrictions Imposed by the Geneva Conventions “Moral Distancing” Developing and Participating in Torture Battlefield Cases of Physician Participation in Torture CONCLUSION *Colonel (Retired), Medical Corps, United States Army; formerly, Director, Borden Institute, Walter Reed Army Medical Center, Washington, DC 20307-5001 and Medical Ethics Consultant to The Surgeon General, United States Army; formerly, Director, Operating Room, 28th Combat Support Hospital (deployed to Saudi Arabia and Iraq, Persian Gulf War) 369 Military Medical Ethics, Volume 2 Robert Benney The Battle of the Caves Anzio, 1944 The painting depicts battlefield medicine in the Mediterranean theater in World War II.