Urology Flexible Cystoscopy 2018 Reimbursement Guide Medicare
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Urology 1 Cystoscopes
Urology 1 Cystoscopes 2 Urethrotomes 3 Resectoscopes 4 Uretero-Renoscopes 5 Nephroscopes 6 Lithotripsy (UreTron) 7 Laser Therapy 8 Small Caliber 9 Fluid Management 10 Accessories Richard Wolf Medical Instruments Corporation assumes no responsibility or liability for any errors or omissions in the content of this catalog. The information contained in this catalog is provided on an “as is” basis with no guarantees of completeness, accuracy, usefulness, or timeliness, and without warranties of any kind whatsoever, expressed or implied. 1777- 02.01-1118USA Cysto-Urethroscopes 8650 E-line design CYSTOSCOPES The E-line design guarantees optimum handling and safe, fatigue-free operation as well as a wide range of possible combinations. Basic Set for Cystoscopy Cysto-urethroscope sheath, 19.5 Fr. with obturator 8650.0341 Adapter with 1 instrument port 8650.264 Insert with Albarran deflector, 2 instrument ports 8650.204 Sterile universal sealing valve (pack of 5) 4712348 Viewing obturator 8650.724 Biopsy forceps Marburg 8650.614 Grasping forceps 8650.684 PANOVIEW telescope, 0° 8650.414 PANOVIEW telescope, 70° 8650.415 Otis urethrotome 8517.00 822.31 822.13 822.31 Flexible connector 822.13 Tray 8585030 1777- 02.01-1118USA 2 PANOVIEW Telescopes Overview CYSTOSCOPES Ø Viewing direction Color code Application mm 0° blue Standard 4 8650.414 12° orange Standard 4 8654.431 Standard 4 8654.422 30° red Long sheath 4 8668.433* 70° yellow Standard 4 8650.415 * Only 25° available. 1777- 02.01-1118USA 3 Cysto-Urethroscope 8650 for telescope 4 mm, 0°, 12°, 30°, 70° and adapters CYSTOSCOPES Sheaths and obturators Adapters Sheath incl. -

Cystoscopy to Understand a Cystoscopy, It Is Helpful to Become Familiar with the Urinary System (Figure 1)
Northwestern Memorial Hospital Patient Education TESTS AND PROCEDURES Cystoscopy To understand a cystoscopy, it is helpful to become familiar with the urinary system (Figure 1). The system’s main purpose is to remove urinary waste products from your body. Urine is produced by the kidneys, moves through the ureters and is stored in the bladder. The bladder is a balloon-like organ that stores urine. The urethra is the tube that carries urine from the bladder out of your body. If you have Figure 1. Urinary system any questions or concerns, Kidneys please ask your physician or nurse. Ureters Bladder Urethra A cystoscopy is a procedure that allows your physician to look at the inside of your urethra and bladder. A telescope-like instrument called a cystoscope is passed through your urethra into your bladder. During the procedure, your physician may also do the following, as needed: ■ Remove stones from your bladder or ureters ■ Place or remove a ureteral stent ■ Insert medication into your bladder ■ Remove small pieces of tissue for testing (biopsy) from your urinary tract A cystoscopy may be done in a physician’s office or in the hospital’s operating room (OR). Your physician will discuss which option is best for you. Preparation and procedure If the test is done in the OR, you will be asked to sign a written consent. The OR procedure and any special preparation will be explained to you. There may be some discomfort during the examination. Some patients may require sedation or anesthesia. Depending on the type of medication used for your procedure, you will be told if you need to stop eating and drinking before your procedure. -

Urological Trauma
Guidelines on Urological Trauma D. Lynch, L. Martinez-Piñeiro, E. Plas, E. Serafetinidis, L. Turkeri, R. Santucci, M. Hohenfellner © European Association of Urology 2007 TABLE OF CONTENTS PAGE 1. RENAL TRAUMA 5 1.1 Background 5 1.2 Mode of injury 5 1.2.1 Injury classification 5 1.3 Diagnosis: initial emergency assessment 6 1.3.1 History and physical examination 6 1.3.1.1 Guidelines on history and physical examination 7 1.3.2 Laboratory evaluation 7 1.3.2.1 Guidelines on laboratory evaluation 7 1.3.3 Imaging: criteria for radiographic assessment in adults 7 1.3.3.1 Ultrasonography 7 1.3.3.2 Standard intravenous pyelography (IVP) 8 1.3.3.3 One shot intraoperative intravenous pyelography (IVP) 8 1.3.3.4 Computed tomography (CT) 8 1.3.3.5 Magnetic resonance imaging (MRI) 9 1.3.3.6 Angiography 9 1.3.3.7 Radionuclide scans 9 1.3.3.8 Guidelines on radiographic assessment 9 1.4 Treatment 10 1.4.1 Indications for renal exploration 10 1.4.2 Operative findings and reconstruction 10 1.4.3 Non-operative management of renal injuries 11 1.4.4 Guidelines on management of renal trauma 11 1.4.5 Post-operative care and follow-up 11 1.4.5.1 Guidelines on post-operative management and follow-up 12 1.4.6 Complications 12 1.4.6.1 Guidelines on management of complications 12 1.4.7 Paediatric renal trauma 12 1.4.7.1 Guidelines on management of paediatric trauma 13 1.4.8 Renal injury in the polytrauma patient 13 1.4.8.1 Guidelines on management of polytrauma with associated renal injury 14 1.5 Suggestions for future research studies 14 1.6 Algorithms 14 1.7 References 17 2. -

Urology Services in the ASC
Urology Services in the ASC Brad D. Lerner, MD, FACS, CASC Medical Director Summit ASC President of Chesapeake Urology Associates Chief of Urology Union Memorial Hospital Urologic Consultant NFL Baltimore Ravens Learning Objectives: Describe the numerous basic and advanced urology cases/lines of service that can be provided in an ASC setting Discuss various opportunities regarding clinical, operational and financial aspects of urology lines of service in an ASC setting Why Offer Urology Services in Your ASC? Majority of urologic surgical services are already outpatient Many urologic procedures are high volume, short duration and low cost Increasing emphasis on movement of site of service for surgical cases from hospitals and insurance carriers to ASCs There are still some case types where patients are traditionally admitted or placed in extended recovery status that can be converted to strictly outpatient status and would be suitable for an ASC Potential core of fee-for-service case types (microsurgery, aesthetics, prosthetics, etc.) Increasing Population of Those Aged 65 and Over As of 2018, it was estimated that there were 51 million persons aged 65 and over (15.63% of total population) By 2030, it is expected that there will be 72.1 million persons aged 65 and over National ASC Statistics - 2017 Urology cases represented 6% of total case mix for ASCs Urology cases were 4th in median net revenue per case (approximately $2,400) – behind Orthopedics, ENT and Podiatry Urology comprised 3% of single specialty ASCs (5th behind -

Mimickers of Urothelial Carcinoma and the Approach to Differential Diagnosis
Review Mimickers of Urothelial Carcinoma and the Approach to Differential Diagnosis Claudia Manini 1, Javier C. Angulo 2,3 and José I. López 4,* 1 Department of Pathology, San Giovanni Bosco Hospital, 10154 Turin, Italy; [email protected] 2 Clinical Department, Faculty of Medical Sciences, European University of Madrid, 28907 Getafe, Spain; [email protected] 3 Department of Urology, University Hospital of Getafe, 28905 Getafe, Spain 4 Department of Pathology, Cruces University Hospital, Biocruces-Bizkaia Health Research Institute, 48903 Barakaldo, Spain * Correspondence: [email protected]; Tel.: +34-94-600-6084 Received: 17 December 2020; Accepted: 18 February 2021; Published: 25 February 2021 Abstract: A broad spectrum of lesions, including hyperplastic, metaplastic, inflammatory, infectious, and reactive, may mimic cancer all along the urinary tract. This narrative collects most of them from a clinical and pathologic perspective, offering urologists and general pathologists their most salient definitory features. Together with classical, well-known, entities such as urothelial papillomas (conventional (UP) and inverted (IUP)), nephrogenic adenoma (NA), polypoid cystitis (PC), fibroepithelial polyp (FP), prostatic-type polyp (PP), verumontanum cyst (VC), xanthogranulomatous inflammation (XI), reactive changes secondary to BCG instillations (BCGitis), schistosomiasis (SC), keratinizing desquamative squamous metaplasia (KSM), post-radiation changes (PRC), vaginal-type metaplasia (VM), endocervicosis (EC)/endometriosis (EM) (müllerianosis), -

Clinical Significance of Cystoscopic Urethral Stricture
UCSF UC San Francisco Previously Published Works Title Clinical significance of cystoscopic urethral stricture recurrence after anterior urethroplasty: a multi-institution analysis from Trauma and Urologic Reconstructive Network of Surgeons (TURNS). Permalink https://escholarship.org/uc/item/3f57n621 Journal World journal of urology, 37(12) ISSN 0724-4983 Authors Baradaran, Nima Fergus, Kirkpatrick B Moses, Rachel A et al. Publication Date 2019-12-01 DOI 10.1007/s00345-019-02653-6 Peer reviewed eScholarship.org Powered by the California Digital Library University of California World Journal of Urology https://doi.org/10.1007/s00345-019-02653-6 ORIGINAL ARTICLE Clinical signifcance of cystoscopic urethral stricture recurrence after anterior urethroplasty: a multi‑institution analysis from Trauma and Urologic Reconstructive Network of Surgeons (TURNS) Nima Baradaran1 · Kirkpatrick B. Fergus2 · Rachel A. Moses3 · Darshan P. Patel3 · Thomas W. Gaither2 · Bryan B. Voelzke4 · Thomas G. Smith III5 · Bradley A. Erickson6 · Sean P. Elliott7 · Nejd F. Alsikaf8 · Alex J. Vanni9 · Jill Buckley10 · Lee C. Zhao11 · Jeremy B. Myers3 · Benjamin N. Breyer2 Received: 13 December 2018 / Accepted: 24 January 2019 © Springer-Verlag GmbH Germany, part of Springer Nature 2019 Abstract Purpose To assess the functional Queryoutcome of patients with cystoscopic recurrence of stricture post-urethroplasty and to evaluate the role of cystoscopy as initial screening tool to predict future failure. Methods Cases with cystoscopy data after anterior urethroplasty in a multi-institutional database were retrospectively studied. Based on cystoscopic evaluation, performed within 3-months post-urethroplasty, patients were categorized as small-caliber (SC) stricture recurrence: stricture unable to be passed by standard cystoscope, large-caliber (LC) stricture accommodating a cystoscope, and no recurrence. -

Surgical Treatment of Urinary Incontinence in Men
Committee 13 Surgical Treatment of Urinary Incontinence in Men Chairman S. HERSCHORN (Canada) Members H. BRUSCHINI (Brazil), C.COMITER (USA), P.G RISE (France), T. HANUS (Czech Republic), R. KIRSCHNER-HERMANNS (Germany) 1121 CONTENTS I. INTRODUCTION VIII. TRAUMATIC INJURIES OF THE URETHRA AND PELVIC FLOOR II. EVALUATION PRIOR TO SURGICAL THERAPY IX. CONTINUING PEDIATRIC III. INCONTINENCE AFTER RADICAL PROBLEMS INTO ADULTHOOD: THE PROSTATECTOMY FOR PROSTATE EXSTROPHY-EPISPADIAS COMPLEX CANCER X. DETRUSOR OVERACTIVITY AND IV. INCONTINENCE AFTER REDUCED BLADDER CAPACITY PROSTATECTOMY FOR BENIGN DISEASE XI. URETHROCUTANEOUS AND V. SURGERY FOR INCONTINENCE IN RECTOURETHRAL FISTULAE ELDERLY MEN VI. INCONTINENCE AFTER XII. THE ARTIFICIAL URINARY EXTERNAL BEAM RADIOTHERAPY SPHINCTER (AUS) ALONE AND IN COMBINATION WITH SURGERY FOR PROSTATE CANCER XIII. SUMMARY AND RECOMMENDATIONS VII. INCONTINENCE AFTER OTHER TREATMENT FOR PROSTATE CANCER REFERENCES 1122 Surgical Treatment of Urinary Incontinence in Men S. HERSCHORN, H. BRUSCHINI, C. COMITER, P. GRISE, T. HANUS, R. KIRSCHNER-HERMANNS high-intensity focused ultrasound, other pelvic I. INTRODUCTION operations and trauma is a particularly challenging problem because of tissue damage outside the lower Surgery for male incontinence is an important aspect urinary tract. The artificial sphincter implant is the of treatment with the changing demographics of society most widely used surgical procedure but complications and the continuing large numbers of men undergoing may be more likely than in other areas and other surgery and other treatments for prostate cancer. surgical approaches may be necessary. Unresolved problems from pediatric age and patients with Basic evaluation of the patient is similar to other areas refractory incontinence from overactive bladders may of incontinence and includes primarily a clinical demand a variety of complex reconstructive surgical approach with history, frequency-volume chart or procedures. -

A New Look at the Etiology of Interstitial Cystitis/Bladder Pain Syndrome: Extraordinary Cultivations
International Urology and Nephrology (2019) 51:1961–1967 https://doi.org/10.1007/s11255-019-02248-5 UROLOGY - ORIGINAL PAPER A new look at the etiology of interstitial cystitis/bladder pain syndrome: extraordinary cultivations Tahsin Batuhan Aydogan1 · Oznur Gurpinar2 · Ozgen Koseoglu Eser2 · Begum Aydogan Mathyk3 · Ali Ergen1 Received: 25 April 2019 / Accepted: 24 July 2019 / Published online: 30 July 2019 © Springer Nature B.V. 2019 Abstract Purpose So far, studies have not clearly identifed infectious agents as an etiological factor for interstitial cystitis (IC). Spe- cifc microbiological diagnosis for detecting the pathogen with higher sensitivity in IC may decrease the treatment costs and increase psychosocial health of the patients. Methods A prospective clinical study was performed in 26 IC patients and 20 controls between April and September 2017. All participants were asked to give mid-stream urine sample for routine urine cultures. Followed by the negative results, symptomatic 26 patients were evaluated for L-form pathogen existence by extraordinary cultivation methods. Biopsy sam- ples were taken from 19 patients with ulcerative lesions in the bladder while collecting sterile urine samples from all 26 patients. PG broth, 5% sheep blood agar, EMB, Sabouraud’s dextrose, LEM, and GYPA were used. Followed by the 1st day inoculations, all inoculated PG broths were subcultured into the same solid media at the 2nd and 10th days in case of any growth after incubation of 24 h under 35–37 °C. The “O’Leary Sant Symptom and Problem Index” score forms were used to evaluate response to the appropriate treatment for those patients with documented pathogens. -

Interstitial Cystitis/Painful Bladder Syndrome
What I need to know about Interstitial Cystitis/Painful Bladder Syndrome U.S. Department of Health and Human Services National Kidney and Urologic Diseases NATIONAL INSTITUTES OF HEALTH Information Clearinghouse What I need to know about Interstitial Cystitis/Painful Bladder Syndrome U.S. Department of Health and Human Services National Kidney and Urologic Diseases NATIONAL INSTITUTES OF HEALTH Information Clearinghouse Contents What is interstitial cystitis/painful bladder syndrome (IC/PBS)? ............................................... 1 What are the signs of a bladder problem? ............ 2 What causes bladder problems? ............................ 3 Who gets IC/PBS? ................................................... 4 What tests will my doctor use for diagnosis of IC/PBS? ............................................................... 5 What treatments can help IC/PBS? ....................... 7 Points to Remember ............................................. 14 Hope through Research........................................ 15 Pronunciation Guide ............................................. 16 For More Information .......................................... 17 Acknowledgments ................................................. 18 What is interstitial cystitis/painful bladder syndrome (IC/PBS)? Interstitial cystitis*/painful bladder syndrome (IC/PBS) is one of several conditions that causes bladder pain and a need to urinate frequently and urgently. Some doctors have started using the term bladder pain syndrome (BPS) to describe this condition. Your bladder is a balloon-shaped organ where your body holds urine. When you have a bladder problem, you may notice certain signs or symptoms. *See page 16 for tips on how to say the words in bold type. 1 What are the signs of a bladder problem? Signs of bladder problems include ● Urgency. The feeling that you need to go right now! Urgency is normal if you haven’t been near a bathroom for a few hours or if you have been drinking a lot of fluids. -

Cystoscopy Into the Bladder Via the Urethra, It Is About As Thick As a a Guide for Women
A flexible cystoscope is a thin telescope which is passed Cystoscopy into the bladder via the urethra, it is about as thick as a A Guide for Women pencil. As the cystoscope is flexible, it usually passes easily 1. What is a Cystoscopy? moved so the doctor can look at all the inside lining of the along the curves of the urethra. The flexible tip can also be 2. Why is a Cystoscopy performed? bladder and the opening of the ureters. 3. Preparation for the test 4. About the test 5. Are there any risks? A rigid cystoscope is a shorter rigid telescope, it allows 6. What to expect afterwards? a greater variety of devices to pass down side channels so that the doctor can for example take samples or inject into the bladder. Sometimes, it is necessary to perform a rigid What is a Cystoscopy? Cystoscopy is the name for a procedure allowing a doctor to look into your bladder and urethra with a special telescope cystoscopy at a later date after a flexible cystoscopy. called a cystoscope. Preparation for the test If you are having an outpatient procedure in most cases you When you have a bladder problem, your doctor may use a will be able to eat and drink normally prior to the test. If you cystoscope to see inside your bladder and urethra. The ure- are having general anesthesia, you should refrain from eat- thra is the tube that carries urine from the bladder to the ing and drinking for 6 to 8 hours prior to your cystoscopy. -

Symptoms of Overactive Bladder and Interstitial Cystitis – How Different?
183 Homma Y1, Tanaka M1, Niimi A1 1. Japan Red Cross Medical Centre SYMPTOMS OF OVERACTIVE BLADDER AND INTERSTITIAL CYSTITIS – HOW DIFFERENT? Hypothesis / aims of study Overactive bladder (OAB) is a symptom syndrome of urgency, frequency or urgency incontinence [1]. Interstitial cystitis (IC) is a bladder disease with a symptom syndrome of urgency, frequency, or bladder pain. Difference in symptoms of these confusable disorders is to be examined. Study design, materials and methods Female patients with OAB or IC and asymptomatic controls were recruited for the study. Diagnosis of OAB is based on 1) OAB symptom score [2] larger than 5 and/or urgency incontinence, and 2) exclusion of stress urinary incontinence and other obvious diseases. IC was diagnosed by 1) O’Leary & Sant’s symptom score [3] larger than 7 and/or bladder pain, 2) exclusion of other obvious diseases, and 3) Hunner’s ulcer or bladder bleeding at hydrodistension under anesthesia. The subjects recorded, in 3-day bladder diary, time voided, voided volume and intensity (0: none, 1: slightly, 2: moderately, 3: a lot) of 6 sensations or symptoms (urge to void, fear of leakage, amount of leakage, bladder discomfort, bladder pain and feeling of incomplete emptying) for each micturition. Additionally the urge questionnaire of 5 questions addressing the conditions during the last week was administered: 1) Did you feel urge to void that was not followed by voiding? (Response: yes, no), 2) Did you feel strong urge to void? (yes, no), 3) In case of yes in question 2, did you feel strong urge to void suddenly? (yes, no), 4) What happened or might happen, if you held strong urge to void for a long time, 1 hour for example ? (Response: leak urine, feel discomfort and/or pain, both), 5) In case of discomfort and/or pain in question 4, could you tell these 2 sensations apart? (yes, no). -
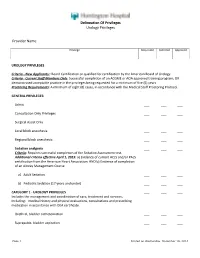
Delineation of Privileges Urology Privileges Provider Name
Delineation Of Privileges Urology Privileges Provider Name: Privilege Requested Deferred Approved UROLOGY PRIVILEGES Criteria - New Applicants:: Board Certification or qualified for certification by the American Board of Urology. Criteria - Current Staff Members Only: Successful completion of an ACGME or AOA approved training program; OR demonstrated acceptable practice in the privileges being requested for a minimum of five (5) years. Proctoring Requirements: A minimum of eight (8) cases, in accordance with the Medical Staff Proctoring Protocol. GENERAL PRIVILEGES: Admit ___ ___ ___ Consultation Only Privileges ___ ___ ___ Surgical Assist Only ___ ___ ___ Local block anesthesia ___ ___ ___ Regional block anesthesia ___ ___ ___ Sedation analgesia ___ ___ ___ Criteria: Requires successful completion of the Sedation Assessment test. Additional criteria effective April 1, 2015: a) Evidence of current ACLS and/or PALS certification from the American Heart Association; AND b) Evidence of completion of an Airway Management Course a) Adult Sedation ___ ___ ___ b) Pediatric Sedation (17 years and under) ___ ___ ___ CATEGORY 1 - UROLOGY PRIVILEGES ___ ___ ___ Includes the management and coordination of care, treatment and services, including: medical history and physical evaluations, consultations and prescribing medication in accordance with DEA certificate. Urethral, bladder catheterization ___ ___ ___ Suprapubic, bladder aspiration ___ ___ ___ Page 1 Printed on Wednesday, December 10, 2014 Delineation Of Privileges Urology Privileges Provider