Macro-Contextual Determinants of Cancer Screening Participation and Inequalities: a Multilevel Analysis of 29 European Countries
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Nasty Gal Offices to Remain Open in Los Angeles
NEWSPAPER 2ND CLASS $2.99 VOLUME 73, NUMBER 10 MARCH 3–9, 2017 THE VOICE OF THE INDUSTRY FOR 72 YEARS BCBGMaxAzria Files for Chapter 11 Bankruptcy Protection By Deborah Belgum Senior Editor BCBGMaxAzriaGroup, the decades-old Los Angeles apparel company that was one of the first on the contempo- rary fashion scene, filed for Chapter 11 bankruptcy protec- tion in papers submitted Feb. 28 to the U.S. Bankruptcy Court for the Southern District of New York. The company’s Canadian affiliate is beginning a sepa- rate filing for voluntary reorganization proceedings under Canada’s Bankruptcy and Insolvency Act. Steps are being taken to close its freestanding stores in Canada and consoli- date its operations in Europe and Japan. The apparel venture, founded in 1989 by Max Azria, has been navigating through some tough financial waters in the past few years. New executives have been unable to turn the company around fast enough and now hope to finish the bankruptcy process in six months. ➥ BCBG page 9 Mitchell & Ness’ booth at the Agenda trade show in Las Vegas TRADE SHOW REPORT Sports Apparel Maker Mitchell & Ness Moving to Irvine Crowded Trade Show By Andrew Asch Retail Editor Schedule Cuts Into LA The North American licensed sportswear business is esti- tive officer. mated to be a multi-billion-dollar market, and Philadelphia- “This facility will house all of our product under one roof Textile Traffic headquartered brand Mitchell & Ness is making a gambit for and modernize our operations with the goal of providing a bigger chunk of it. It is scheduled to open its first West Coast gold-standard customer service. -

Superbrands 2006
essential for the development of the Jolidon Jolidon believes that underwear and brand. swimwear items are not merely “fashion items”. 2006 saw the launch of a new Jolidon brand - These products need to fit consumers, adapt to Prelude, designed for the most refined and their size, age and contemporary trends, so that sophisticated tastes in lingerie. they feel as comfortable as possible and best The new brand was born with the most express the wearer's personality. demanding customers in mind.To create the Other means of communication and PRELUDE line, designers played with a mix of promotion for Jolidon are the participation in precious accessories and fabrics and enhanced various specialist international fairs and events, the classical beauty of the articles with sophisticated details and daring cuts. PRELUDE is a refined line for the woman who Market Achievements is in love with fashion and luxury.The individuality At the start of the 1990s, the Romanian lingerie The beginning of 2006 saw of the models is created not only through and swimwear market was still an unexplored Jolidon acknowledged as one of particularly original cuts, but also by making use area.The market only offered a scant selection, the most prestigious names in of unusual accessories. made up of limited imports and a single the world lingerie field.This From classic white-black combinations with Romanian brand, Argos. Jolidon was born in confirmation of the Romanian gleaming crystals, romantic filigree laces, 1993 out of a desire to reply to this need and, as brand's reputation and handmade accessories and elegant drapes, to a result, it contributed much to shaping the importance came directly from aggressively cut low-necks and avant-garde lines, lingerie and swimwear market in Romania and to the land of lingerie itself, France. -

The Leading French Magazine for Lingerie and Beachwear
2015 Rates The leading French Magazine for lingerie and beachwear INTIMA CAN BE FOUND PREVIOUSLY FEATURED AT THESE TRADESHOWS IN INTIMA… CurveNY (New York – USA) The Best of Intima/Network Dessous lounge Brands: Affinitas; Agogoa; Aimer; Amoena; Andres Sarda; Anita; Anita Active; CurveNV (Las Vegas – USA) The Best of Intima/Network Dessous booth Antigel; Antinéa; Artimaglia; Aubade; Axami, B&B Creazioni; BBF Gambetti; Fimast (Montichiari (BS) – Italy) Linea Intima/Network Dessous lounge Barbara; Blumarine; Canat; Cheek; Christies; Corin; Cosabella; Cotonella; Cotton Club; Daniel Hechter; Elise Aucouturier; Eminence; Emporio Armani; Empreinte; Galleria Intima - Intimate Apparel Association of India Intima Asia/ Network Dessous Empreinte Bain; Eprise; Etna, Ewa Bien, Exilia; Fantasie , Fashion Forms; Fiore Immagine Italia (Florence – Italy) Linea Intima/Network Dessous lounge Calze; Foemina; Freya; Guess; Gottex; Hanky Panky; Hanro; Hudson; Huit; ID Interfilière Hong Kong (Hong Kong) Intima Asia/Network Dessous booth Sarrieri Bain; Impetus; Implicite; Inès de la Fressange; Jolidon; Joy de Villaret; Julie Interfilière (Paris – France) Intima/Network Dessous lounge France; Kunert ; La Tunisie; Lahco; La Perla; Le Cap; Le Chat; Lionella; Lise Kiev Fashion (Kiev - Ukraine) Intimoda/Network Dessous lounge Charmel; Lou; Madame Supertrash; Madiva; Maison Close; Maison Lejaby; Marie Lingerie Expo (Moscow - Russia) Intimoda/Network Dessous booth Jo; Marie Jo l’Aventure; Marlies Dekkers ; Maryan Mehlhorn; Milavitsa; Millesia; Mura; Naturana; Oscalito; -

Sgs Investor Days 2018 Sgs Investor Bordeaux Days 8-9 November 2018
SGS INVESTOR DAYS 2018 SGS INVESTOR BORDEAUX DAYS 8-9 NOVEMBER 2018 CONTACT Julie Engelen +41786229285 Manéa Pesquet +33632142075 WIFI CODE INTERCONTINENTAL BORDEAUX LE GRAND HÔTEL Login IHG connect Password IHGBORDEAUX AGENDA WEDNESDAY 7 NOVEMBER Afternoon ARRIVAL OF PARTICIPANTS 15:30 – 18:00 ACTIVITY FOR EARLY ARRIVED PARTICIPANTS 18:30 MEETING POINT – LOBBY INTERCONTINENTAL BORDEAUX – LE GRAND HÔTEL 18:45 DEPARTURE FOR THE VISIT 19:00 VISIT CITÉ DU VIN 20:00 OPENING DINNER 7 RESTAURANT – CITÉ DU VIN THURSDAY 8 NOVEMBER ROOM MARGAUX – INTERCONTINENTAL BORDEAUX – 8:00 – 12:00 SGS PRESENTATIONS LE GRAND HÔTEL • TOBY REEKS Format for the day • FRANKIE NG Welcome to SGS Investor Days • FRANKIE NG – CARLA DE GEYSELEER Strategy and finance update • JEFF MCDONALD Shared services – how CBE has benefitted • CARLA DE GEYSELEER Risk intelligence • VINCENZO TORRISI Path to Inorganic Growth • FILIPPO ROTA Operational Excellence • THOMAS KLUKAS World Class Services @SGS L’ORANGERAIE – INTERCONTINENTAL BORDEAUX – 12:00 LUNCH LE GRAND HÔTEL MEETING POINT – LOBBY – INTERCONTINENTAL BORDEAUX – 13:10 MEETING POINT – LOBBY LE GRAND HÔTEL 13:20 DEPARTURE FOR SGS CESTAS 14:30 – 17:30 VISIT OF THE SGS LABS SGS CESTAS 19:00 MEETING POINT – LOBBY INTERCONTINENTAL BORDEAUX – LE GRAND HÔTEL 19:15 DEPARTURE INTERCONTINENTAL BORDEAUX – LE GRAND HÔTEL 19:45 VISIT AND WINE TESTING CHÂTEAU SMITH HAUT LAFITTE 20:30 APERITIVE & DINNER CHÂTEAU SMITH HAUT LAFITTE FRIDAY 9 NOVEMBER 8:00 – 12:00 SGS PRESENTATIONS ROOM MARGAUX – INTERCONTINENTAL BORDEAUX – LE GRAND HÔTEL -

Need Expert Insight?
NOVEMBER 2020 NEED EXPERT INSIGHT? UBP specialists provide you with their economic views and investment convictions, and answer your questions. All questions and queries concerning UBP’s corporate strategy and organisation will be answered by Corporate Communications. EMEA: Maude Hug, Head of Media Relations – [email protected] or Audrey Berladyn, Media Relations Manager – [email protected] ASIA: Jenny Lai, Head of Media Relations Asia and Communications Manager Hong Kong – [email protected] Content ASSET MANAGEMENT 3 Equities 7 Institutional Clients 3 Swiss & Global 7 Investment Strategy 3 European Small- & Mid-Cap 7 Investment Management 3 US / Japan 7 China 3 Research Asia 7 Macroeconomy 3 Research China 7 Investment Services 3 Energy 7 Investment Strategy 3 Responsible Investment 8 Market Heads 4 Responsible Investment AM 8 France 4 Responsible Investment WM 8 Italy 4 Impact Investing 8 United-Kingdom 4 Alternative & Thematic Investments 9 Spain 4 Alternative Investments 9 Germany 4 Forex 9 Dubai 4 Multi-Management & Fund Research 9 Asia 4 WEALTH MANAGEMENT 10 Fixed income 5 Zurich 10 Global & Absolute Return 5 Asia 10 Convertibles 5 Dubai 10 Emerging Markets 6 Wealth Planning 11 Research Asia 6 Discretionary Portfolio Management 11 Multi-Asset 11 Union Bancaire Privée, UBP SA | Speakers list | November 2020 2 | 11 Asset Management INSTITUTIONAL CLIENTS INVESTMENT MANAGEMENT MACROECONOMY INVESTMENT STRATEGY Nicolas Faller Michaël Lok Patrice Gautry Norman Villamin Co-CEO Asset Management Co-CEO Asset Management Chief Economist CIO Wealth Management Head of Institutional Clients Group Chief Investment Officer & Head of Asset Allocation Location: Zurich Location: Geneva Location: Geneva Location: Zurich Speaks: French/English/German Speaks: French/English Speaks: French/English Speaks: English Nicolas joined UBP in 2010 as Michaël joined UBP in 2015 as Patrice has been UBP’s Chief Norman has over 20 years’ Head of Sales Europe. -

International Week: Business Education Without Borders
International Week: Business Education without Borders 3-7 April 2017 SPONSORS International Week: Business Education without Borders 3-7 April 2017 Workshop & Food Tasting The Workshop Mind the Gap: The University he Faculty of Economics and Business Adminis- and the Business Environment took place on tration from Babeș-Bolyai University organized the Wednesday, 5th of April 2017. During this event, T 2nd edition of the International Week between 3rd and 7th of April 2017. The theme of International Week was students had the chance to listen, discuss Business Education without Borders. During the event, over and talk with two young business persons: 100 Romanian and international students from the Facul- Lavinia Florea (HR Operations Manager Office ty of Economics and Business Administration attended Depot SSC) and Rada Sonea (Business Devel- classes taught by guest lecturers from abroad. The spon- opment Manager for OKEY) sors of this year’s event were: Jolidon and Vos Logistics. A very pleasant experience was the Food Tasting Event during which our international students cooked some traditional dishes Courses from their home countries. Courses were taught by international guest lecturers from our partner universities: • Dr. Alena Buchalcevová from • María Nela Seijas Giménez from University of Economics, Prague, Universidad de la Republica, Czech Republic taught the course Uruguay taught the course on on Software Process Improvement; Technical Analysis: How to Forecast • Thierry Keuscher from Chemnitz Market Trends and Make Better University of Technology, Germany Investing Decisions; taught the course on General • Dr. Umesh Raut from Corvinus Management; University of Budapest, Hungary • Prof. dr. József Poór from Szent taught the course on Brand István University, Hungary taught the Relationship Management; course on Management Consulting; • Lucie Vrbova from University of • Dr. -

General Assembly
United Nations A/C.3/71/INF/ 2 Distr.: General General Assembly 25 January 2016 Original: Arabic/Chinese/English/ French/Russian/Spanish ﺃﻋﻀﺎﺀ ﺍﻟﻠﺠﻨﺔ 第三委员会成员 Membership of the Third Committee Membres de la Troisième Commission Члены Третьего комитета Miembros de la Tercera Comisión ﻣﻠﺤﻮﻇﺔ: ﻳﺮﺟﻰ ﻣﻦ ﺍﻟﻮﻓﻮﺩ ﺍﻟﱵ ﺗﺮﻳﺪ ﺇﺩﺧﺎﻝ ﺃﻳﺔ ﺗﺼﺤﻴﺤﺎﺕ ﻋﻠﻰ ﺍﻟﻘﺎﺋﻤﺔ ﺍﻟﺘ ﺎﻟﻴﺔ ﺃﻥ ﺗﺮﺳﻠﻬﺎ، ﻛﺘﺎﺑﺔ، ﺇﱃ ﺃﻣﲔ ﺍﻟﻠﺠﻨﺔ، ﺍﻟﻐﺮﻓﺔ ﺭﻗﻢ S-1279 ، ﻣﺒﲎ Secretariat Building 注意:请各代表团把对以下名单的更正用书面送交 Secretariat Building 大楼 S-1279 室委员会秘书。 Note : Delegations are requested to send their corrections to the following list in writing to the Secretary of the Committee, room S-1279, Secretariat Building. Note: Les délégations sont priées d’envoyer leurs corrections à la présente liste, par écrit, au Secrétaire de la Commission, bureau S-1279, Secretariat Building. Примечание: Делегациям предлагается послать свои исправелния к настоящему списку в письменной форме секретарю Комитета, комната S-1279, здание Secretariat Building. Nota: Se ruega a las delegaciones se sirvan enviar sus correcciones a la siguiente lista, por escrito, a la Secretaria de la Comisión, oficina S-1279, Secretariat Building. ﺍﻟﺮﺋﻴﺲ 主席 Chairman Président Председатель Presidente ﻧﻮﺍﺏ ﺍﻟﺮﺋﻴﺲ (H.E. Mrs. María Emma Mejía (Colombia 副主席 Vice-Chairmen Vice-Présidents Заместители Председателя Vicepresidentes Mr. Masni Eriza (Indonesia) Mrs. Karina Węgrzynowska (Poland) Mr. Andreas Glossner (Germany) ﺍﳌﻘﺮﺭ 报告员 Rapporteur Докладчик Relator Mrs. Cecile Mbala Eyenga (Cameroon) 270117 270117 17-01287 (M) 1701287 A/C.3/71/INF/2 成员 /Members/Membres/Члены/Miembros/ ﺍﻷﻋﻀﺎﺀ ﺍﳌﺴﺘﺸﺎﺭﻭﻥ ﺍﳌﻤﺜﻠﻮﻥ ﺍﳌﻨﺎﻭﺑﻮﻥ ﺍﳌﻤﺜﻞ ﺍﻟﺒﻠﺪ 国家 代表 候补代表 顾问 Country Representative Alternates Advisers Pays Représentant Suppléants Conseillers Страна Представитель Заместители Советники País Representante Suplentes Consejeros Afghanistan Mr. -

Bank Guarantees and Letters of Credit: Time for a Return to the Fold
ARTICLES BANK GUARANTEES AND LETTERS OF CREDIT: TIME FOR A RETURN TO THE FOLD BORIS KOZOLCHYK* TABLE OF CONTENTS Foreword by James E. Byrne ................................ 3 1 Introduction: Bank Guarantees, Standby and Commercial Letters of C redit .................................................... 7 2 The 1978 ICC Uniform Rules for Contract Guarantees (URCG) ................................................... 11 3 The Contemporary European Bank Guarantee: The Practice.. 15 3.1 Types of Issuers ................................... 15 3.2 The Context of Issuance ............................. 16 3.3 The Bank Guarantee Profile ......................... 18 3.4 Customary Bank Guarantee Forms .................... 20 3.4.1 The Causal Section ............................. 21 3.4.2 The Abstract Section: Sources of Abstraction ......... 25 * © 1989, Boris Kozolchyk. Professor of Law, University of Arizona College of Law. This article is dedicated to Henry Harfield, Esq., whose teachings, friendship and wit this author has enjoyed for many years, on the occasion of his retirementfrom the hyperactive practice of law. (Henry will never retire from active practice.) This article contains segments of two chapters of B. KOZOLCHYK, COMMERCIAL LETTERS OF CREDIT IN THE AMERICAS (2d ed.), to be published by Little, Brown and Co. The author wishes to thank Professor James E. Byrne of the George Mason University School of Law for his thoughtful comments and suggestions, and acknowledges the helpful assistance of Harold S. Burman, Esq. of the Office of the Legal Advisor, United States Department of State, for facilitating access to helpful documentation; Mark Wayne for the preparation of Appendices A-C and the litigation chart (in con- junction with Anne Hunnycut); Mark Richter, a Harvard-Zurich doctoral candidate for supplying some of the European bank guarantee forms; and Angela P. -

CWIHP Publication Index - Article Keywords
CWIHP Publication Index - Article Keywords Keyword 1948 "Prague coup" Publication Page number Title Author Bulletin 11 141 The Polish Contribution to the Victory of the "Prague Coup" in February 1948 Andrzej Paczkowski Keyword 1956 "Polish October" Publication Page number Title Author Working Paper 17 4 The Soviet-Polish Confrontation of October 1956: The Situation in the Polish Internal Leszek Gluchowski and Edward Jan Nalepa Keyword 1956 North Korean Opposition Movement Publication Page number Title Author Working Paper 52 1 "We Need Help From the Outside": The North Korean Opposition Movement of 1956 James F. Person Keyword 1956 Polish and Hungarian Crises Publication Page number Title Author Bulletin 05 1 Khrushchev's CPSU CC Presidium Meeting on East European Crises, 24 October 1956 Mark Kramer Bulletin 06-07 280 Response: More on the 1956 Polish Crisis Milton Leitenberg and L.W. Gluchowski Bulletin 06-07 283 Response: More on the 1956 Hungarian Crisis Charles Gati and Raymond Garthoff Bulletin 08-09 355 Conferences in Budapest, Potsdam Spoltlight Cold War Flashpoints Malcolm Byrne, James Hershberg, Christian Ostermann Bulletin 08-09 358 New Evidence on Soviet Decision-Making and the 1956 Polish and Hungarian Crises Mark Kramer Bulletin 08-09 385 The "Malin Notes" on the Crises in Hungary and Poland, 1956 Mark Kramer Keyword Afghanistan - Soviet Invasion Publication Page number Title Author Bulletin 03 67 Soviet Policy in Afghanistan, 1979: A Grim Assessment Robert Litwak Bulletin 04 70 From Hesitation to Intervention: Soviet Decisions -

I Dolores '~Lilso-Nin "The Merryu Widow'' August 8Th Through August 13Th, 1961
"Central Illinois ' Only Professional Equity Music Theatre " Fifth Season A July 7th Through Aupust 27th. 1961 Air- Conditioned Grand Theatre * On the Square * Sullivan I 1 6uy S. Little, Jr. Presents I Dolores '~lilso-nin "The Merryu Widow'' August 8th through August 13th, 1961 -- . 4 Who's Who in the Cast . DOLORES WILSON (Sonia) has had JEFF WARREN (Danilo) directed all the many attributes accorded her by some of the product~ons at the Grand last summer and IS foremost critics of Italy. France, Spain, Portu- workin in the same capacity this season. gal and Germany--critics like Andrea della Mr. garren got his first theatre job as tenor Corte, G!useppe Pu !iese, Guido Pannain, Clave, soloist with the touring company of Kurt Weill's etc., saylng thmgs %ke "Sensational revelation" LADY IN THE DARK which starred Gertrude -"Stupendous"-"Complete virtuosity"-"Flair, Lawrence. A month afjer the opening of Kurt youth ele ance and beautyw-"Exceptional tech- Weill's next Broadway success, ONE TOUCH nique''-"610fious singingu-"One of the best OF VENUS he had the opportunity that all coloraturas In the world todayp'-"Unending understudies hream of-he went on during Kenny breath-control" - "Crystal-clear voice" - "Rich Bake-'s extended illness to play opposite Mary timbre, extrordinary agility, limpid high tones" Martin. The result of this was a new part in -"A true diva." In being thus acclaimed the Jackie Gleason show, FOLLOW THE Miss Wilson established a precedent, because GIRLS and a short excursion with HOLLY- she was considered a top coloratura in Europe WOOD PINAFORE which starred Shirley before ever singing in her native Arne-ica. -
Korea Revisit
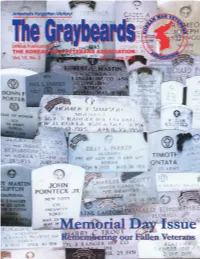
Staff Officers The Graybeards Presidential Envoy to UN Forces: Kathleen Wyosnick The Magazine for Members and Veterans of the Korean War. P.O. Box 3716, Saratoga, CA 95070 The Graybeards is the official publication of the Korean War Veterans Association, PH: 408-253-3068 FAX: 408-973-8449 PO Box, 10806, Arlington, VA 22210, (www.kwva.org) and is published six times per year for members of the Association. Judge Advocate and Legal Advisor: Sherman Pratt 1512 S. 20th St., Arlington, VA 22202 EDITOR Vincent A. Krepps PH: 703-521-7706 24 Goucher Woods Ct. Towson, MD 21286-5655 PH: 410-828-8978 FAX: 410-828-7953 Washington, DC Affairs: Blair Cross E-MAIL: [email protected] 904B Martel Ct., Bel Air, MD 21014 MEMBERSHIP Nancy Monson PH: 410-893-8145 PO Box 10806, Arlington, VA 22210 National Chaplain: Irvin L. Sharp, PH: 703-522-9629 16317 Ramond, Maple Hights, OH 44137 PUBLISHER Finisterre Publishing Incorporated PH: 216-475-3121 PO Box 70346, Beaufort, SC 29902 E-MAIL: [email protected] Korean Ex-POW Associatiion: Elliott Sortillo, President 2533 Diane Street, Portage, IN 46368-2609 National KWVA Headquarters National VA/VS Representative: Michael Mahoney PRESIDENT Harley J. Coon 582 Wiltshire Rd., Columbus, OH 43204 4120 Industrial Lane, Beavercreek, OH 45430 PH: 614-279-1901 FAX: 614-276-1628 PH: 937-426-5105 or FAX: 937-426-8415 E-MAIL: [email protected] E-MAIL: [email protected] Office Hours: 9am to 5 pm (EST) Mon.–Fri. Liaison for Canada: Bill Coe 59 Lenox Ave., Cohoes, N.Y.12047 National Officers PH: 518-235-0194 1st VICE PRESIDENT Edward L. -

BULLETIN 61 Divisions on Your Front Could Fully Satisfy of an Armistice to Comrade GAO GANG in the Korean Army and Chinese Volunteer Troops the Needs of the Front
30 COLD WAR INTERNATIONAL HISTORY PROJECT BULLETIN NEW EVIDENCE ON NEW RUSSIAN DOCUMENTS ON THE KOREAN WAR Introduction and Translations significant first months of the conflict. (Un- Vasilevsky on February 23 (document #4) fortunately, some key materials from this supports accounts given by former DPRK by Kathryn Weathersby period, particularly the months immediately military officers that Stalin began taking preceding the war, have not yet become steps to strengthen the North Korean mili- In the previous issue of the Cold War available; for key documents from mid-Sep- tary forces even before Kim Il Sung’s secret International History Project Bulletin (Issue tember to mid-October 1950, covering events trip to Moscow in April, by appointing Ma- 5, Spring 1995 pp. 1, 2-9), I described the from the Inchon landing to China’s decision jor-General Vasiliev, a Hero of the Soviet collection of high-level documents on the to intervene in the war, see the article by Union and section chief for War Experience Korean War that Russian President Boris Alexandre Y. Mansourov elsewhere in this Analysis in the Soviet General Staff, to re- Yeltsin presented to President Kim Young issue of the CWIHP Bulletin.) It then offers place Shtykov as principal military adviser Sam of South Korea in June 1994. I also a more selective sample of documents from to the Korean People’s Army (KPA).3 presented translations of six key documents spring 1951 through the end of the war, From Shtykov’s telegram to Foreign from that collection that illuminate the deci- focusing primarily on Stalin’s approach to Minister Andrei Vyshinsky on February 7 sion-making behind the outbreak of full- the armistice negotiations.