Management of Infraoccluded Second Primary Molars Without Successors
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
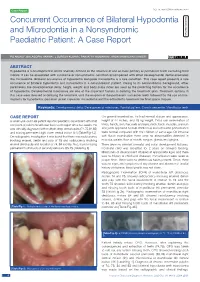
Concurrent Occurrence of Bilateral Hypodontia and Microdontia in a Nonsyndromic Paediatric Patient: a Case Report
Case Report DOI: 10.7860/JCDR/2020/43540.14083 Concurrent Occurrence of Bilateral Hypodontia Dentistry Section and Microdontia in a Nonsyndromic Paediatric Patient: A Case Report PG ANJALI1, BALAGOpaL VARMA2, J SURESH KUMAR3, paRVATHY KUMARAN4, ARUN MAMACHAN XAVIER5 ABSTRACT Hypodontia is a developmental dental anomaly defined as the absence of one or more primary or permanent teeth excluding third molars. It can be associated with syndrome or nonsyndromic condition accompanied with other developmental dental anomalies like microdontia. Bilateral occurrence of hypodontia alongside microdontia is a rare condition. This case report presents a rare occurrence of bilateral hypodontia and microdontia in a nonsyndromic patient. Owing to its nonsyndromic background, other parameters like developmental delay, height, weight and body mass index are used as the predicting factors for the occurrence of hypodontia. Developmental milestones are one of the important factors in deriving the treatment plan. Treatment options in this case were directed at delaying the treatment until the eruption of the permanent successor teeth followed by the use of mini- implants for hypodontia, porcelain jacket crown for microdontia and the orthodontic treatment for final space closure. Keywords: Developmental delay, Developmental milestones, Familial pattern, Growth percentile, Mandibular teeth CASE REPORT On general examination, he had normal stature and appearance, A seven-year-old male patient reported paediatric department with chief height of 44 inches, and 18 kg weight. Extra oral examination of complaint of pain in the left lower back tooth region since two weeks. He limbs, hands, skin, hair, nails and eyes, neck, back, muscles, cranium was clinically diagnosed with multiple deep dental caries (74,75,84,85) and joints appeared normal. -

Section I the Patient BLUK133-Jacobsen December 7, 2007 16:38
BLUK133-Jacobsen December 7, 2007 16:38 Section I The Patient BLUK133-Jacobsen December 7, 2007 16:38 “I’m ready when you are.” 2 BLUK133-Jacobsen December 7, 2007 16:38 Chapter 1 The Patient – His Limitations and Expectations Section I The provision of high-quality restorative dentistry depends upon the dentist: Making an accurate diagnosis Devising a comprehensive and realistic treatment plan Executing the treatment plan to a high technical standard Providing subsequent continuing care There is a very strong tendency, particularly in the and here re-education is often necessary to bring him field of fixed prosthodontics, for the dentist to become down to the practical and feasible. over-interested in the technical execution of treat- It might be that the dentist has the skills and tech- ment. There is a vast range of materials and equip- nical facilities to perform advanced procedures, but ment to stimulate this interest and compete for his before he puts bur to tooth, he must stop and ask attention. It is perhaps inevitable that dentists can be- whether this is really what this patient needs and come obsessive about types of bur or root canal file, wants. If the answer is no, then to proceed is an act the pros and cons of various materials and the precise of pure selfishness that might also be regarded as techniques of restoration. negligent! This is not to decry such interest because a high Certainly the dentist may have certain treatment standard of technical execution is essential for the goals for all his patients – no pain or caries, healthy longevity of restorations. -
Gracis S. a Simplified Method to Develop An
CLINICAL RESEARCH A simplified method to develop an interdisciplinary treatment plan: an esthetically and functionally driven approach in three steps Stefano Gracis, DMD, MSD Private Practice, Milan, Italy Correspondence to: Dr Stefano Gracis Via Brera 28/a, 20121 Milan, Italy; Tel: +39 02 72094471; Email: [email protected] 76 | The International Journal of Esthetic Dentistry | Volume 16 | Number 1 | Spring 2021 GRACIS Abstract typically required. This article provides a practical step- by-step approach to planning comprehensive interdis- Many clinicians are unsure of how to develop a com- ciplinary treatment focused primarily on the teeth as prehensive plan of treatment for patients who present they relate to each other and to the structures that with multiple problems and pathologies. In order to surround them. The approach is based on the answers efficiently plan appropriate treatment for such com- to six questions that are grouped into three steps: 1) plex patient cases, the clinician needs to either have or evaluation of the teeth relative to the face and lips; develop the necessary knowledge of evidence-based 2) assessment of anterior tooth dimensions; and 3) information on the predictability of available clinical analysis of the anteroposterior and maxillomandibular procedures. The clinician also needs to understand relationships. The information obtained must then be the correct sequence in which such treatment is ap- related to the patient’s skeletal framework, periodontal plied, and perfect the skills required for carrying out status, caries susceptibility, and biomechanical risk as- that treatment. Since most clinicians have not ac- sessment in order to formulate a clear and complete quired all the knowledge and skills necessary for this plan of treatment. -

Discuss Before Fabricating: Communicating the Realities of Par Tial Den T U R E Th E R a P Y
C L I N I C A L P R A C T I C E Discuss Before Fabricating: Communicating the Realities of Par tial Den t u r e Th e r a p y . Par t II: Clinical Out c o m e s • Nita M. Mazurat, DDS • • Randall D. Mazurat, BSc, DDS, MDEd • A b s t r a c t The premise of this review is that patients’ satisfaction (and hence compliance) with partial denture therapy may be better if they are more fully informed about the limitations of the prosthesis they are to receive. Neither the dentist nor the patient should assume that all of their respective expectations will be mutually understood and inherently met. By discussing patient-centred issues and predictable clinical outcomes, both dentist and patient will be better prepared to determine whether a removable prosthesis is appropriate. Searches of the Cochrane Collaboration and MEDLINE databases were conducted to identify issues pertaining to patient compliance in wearing cast removable partial dentures. In addition to the 2 most frequent patient concerns, esthetics and mastication, discussed in the first article of this series, additional aspects of concern to the dentist and the patient when considering a removable partial denture include overeruption, post-insertion care, comfort, longevity of the prosthesis, effect on speech and biologic consequences are discussed here. MeSH Key Words: denture, partial, removable; prosthodontics; treatment outcomes © J Can Dent Assoc 2003; 69(2):96–100 This article has been peer reviewed. o re than a quarter of all re m ovable part i a l Materials and Methods dentures (RPDs) fabricated are deemed unsuc- Searches of the Cochrane Collaboration and MEDLINE M cessful,1 where failure is defined as refusal or databases were conducted between January and April 2002 inability to wear the denture. -
Creating Brighter Futures Aesthetics & Teamwork
University of Sydney Aesthetics & Teamwork Creating Brighter Futures Aesthetics & Teamwork Utilizing an Interdisciplinary Approach to Enhance Anterior • The gingival margins of the central incisors should be Dental Aesthetics positioned 0.5-1mm apical to the lateral incisors and should be at the same level as the canines. The general goals of orthodontic treatment are to establish • The contour of the labial gingival margins should follow a good occlusion, enhance periodontal health, and improve the CEJ of the teeth. dental and facial aesthetics. In the past, greater emphasis has been placed on achieving ideal alignment and a good • There should be a papilla between each tooth, which occlusal result, with less emphasis being placed on occupies the apical half of the interproximal contact. periodontal health and the aesthetic appearance of individual teeth. In some patients, well-aligned teeth may still The following situations can detract from an aesthetically look unaesthetic. A “gummy smile”, uneven gingival margins pleasing smile. and crown heights, worn teeth, missing papillae and abnormal tooth morphology can jeopardize the aesthetic 1. The “Gummy Smile” appearance of teeth. In many cases, these unaesthetic situations can be improved through a coordinated The “gummy smile” has three potential causes. It may be teamwork approach of orthodontics, periodontics and the result of excessive vertical maxillary growth, which is restorative dentistry. most often managed with a combined orthodontic and orthognathic surgery treatment approach. Secondly, a “gummy smile” may be caused by delayed apical migration What Contributes to an of the gingival margin, or thirdly, overeruption of the Aesthetically Pleasing Smile? maxillary anterior teeth.The management of the latter two causes is determined by probing the sulcular depth of the Having well-aligned teeth is not the only factor that maxillary anterior teeth. -

Ankylosis of Permanent First Molar: Diagnosis by Cone Beam
Int. J. Odontostomat., 11(3):319-325, 2017. Ankylosis of Permanent First Molar: Diagnosis by Cone Beam Computed Tomography Anquilosis del Primer Molar Permanente: Diagnóstico por Tomografía Computarizada con Haz Cónico Eliana Dantas da Costa1; Priscila Dias Peyneau1; Francielle Silvestre Verner2; Rafael Binato Junqueira3; Solange Maria de Almeida1 & Glaucia Maria Bovi Ambrosano4 DA COSTA, E. D.; PEYNEAU, P. D.; VERNER, F. S.; JUNQUEIRA, R. B.; DE ALMEIDA, S. M. & AMBROSANO, G. M. B. Ankylosis of permanent first molar: Diagnosis by cone beam computed tomography. Int. J. Odontostomat., 11(3):319-325, 2017. ABSTRACT: Ankylosis is an anomaly of tooth eruption characterized by the fusion of cementum and alveolar bone, and may affect from small regions to the entire root surface. Clinical assessment combined with imaging exams can aid diagnosis. Radiographic testing enables assessing only proximal regions of possibly affected roots. Whereas cone beam computed tomography (CBCT) allows a three-dimensional assessment of axial, coronal, and sagittal planes of all dental extension, eliminating thus overlapping images and helping to confirm the correct diagnosis. The present study contains a case report of a male patient with ankylosis in tooth 16 diagnosed by CBCT, aiming at providing information for dentists about this anomaly, its characteristics and situations in which CBCT should be indicated. KEY WORDS: dental ankylosis, diagnosis, cone beam computed tomography. INTRODUCTION Dentoalveolar ankylosis is an anomaly of den- mandibular deciduous first molars (Loriato et al.; Alves tal eruption, caused by mechanical failure of eruption et al.; Bertl et al.; Parisay et al., 2013), followed by (Frazier-Bowers et al., 2007), characterized by the second mandibular and maxillary deciduous molars fusion of cementum and alveolar bone (Loriato et al., (Parisay et al.). -

Does Fixed Retention Prevent Overeruption of Unopposed
University of Groningen Does fixed retention prevent overeruption of unopposed mandibular second molars in maxillary first molar extraction cases? Livas, Christos; Halazonetis, Demetrios J; Booij, Johan W; Katsaros, Christos; Ren, Yijin Published in: Progress in Orthodontics DOI: 10.1186/s40510-016-0119-z IMPORTANT NOTE: You are advised to consult the publisher's version (publisher's PDF) if you wish to cite from it. Please check the document version below. Document Version Publisher's PDF, also known as Version of record Publication date: 2016 Link to publication in University of Groningen/UMCG research database Citation for published version (APA): Livas, C., Halazonetis, D. J., Booij, J. W., Katsaros, C., & Ren, Y. (2016). Does fixed retention prevent overeruption of unopposed mandibular second molars in maxillary first molar extraction cases? Progress in Orthodontics, 17(6). https://doi.org/10.1186/s40510-016-0119-z Copyright Other than for strictly personal use, it is not permitted to download or to forward/distribute the text or part of it without the consent of the author(s) and/or copyright holder(s), unless the work is under an open content license (like Creative Commons). Take-down policy If you believe that this document breaches copyright please contact us providing details, and we will remove access to the work immediately and investigate your claim. Downloaded from the University of Groningen/UMCG research database (Pure): http://www.rug.nl/research/portal. For technical reasons the number of authors shown on this cover page is limited to 10 maximum. Download date: 26-09-2021 Livas et al. Progress in Orthodontics (2016) 17:6 DOI 10.1186/s40510-016-0119-z RESEARCH Open Access Does fixed retention prevent overeruption of unopposed mandibular second molars in maxillary first molar extraction cases? Christos Livas1*, Demetrios J. -

Glossary of Periodontal Terms.Pdf
THE AMERICAN ACADEMY OF PERIODONTOLOGY Glossary of Periodontal Te rms 4th Edition Copyright 200 I by The American Academy of Periodontology Suite 800 737 North Michigan Avenue Chicago, Illinois 60611-2690 All rights reserved. No part of this publication may be reproduced, stored in a retrieval system, or transmitted in any form or by any means, electronic, mechanical, photocopying, or otherwise without the express written permission of the publisher. ISBN 0-9264699-3-9 The first two editions of this publication were published under the title Glossary of Periodontic Terms as supplements to the Journal of Periodontology. First edition, January 1977 (Volume 48); second edition, November 1986 (Volume 57). The third edition was published under the title Glossary vf Periodontal Terms in 1992. ACKNOWLEDGMENTS The fourth edition of the Glossary of Periodontal Terms represents four years of intensive work by many members of the Academy who generously contributed their time and knowledge to its development. This edition incorporates revised definitions of periodontal terms that were introduced at the 1996 World Workshop in Periodontics, as well as at the 1999 International Workshop for a Classification of Periodontal Diseases and Conditions. A review of the classification system from the 1999 Workshop has been included as an Appendix to the Glossary. Particular recognition is given to the members of the Subcommittee to Revise the Glossary of Periodontic Terms (Drs. Robert E. Cohen, Chair; Angelo Mariotti; Michael Rethman; and S. Jerome Zackin) who developed the revised material. Under the direction of Dr. Robert E. Cohen, the Committee on Research, Science and Therapy (Drs. David L. -

GPT-9 the Academy of Prosthodontics the Academy of Prosthodontics Foundation
THE GLOSSARY OF PROSTHODONTIC TERMS Ninth Edition GPT-9 The Academy of Prosthodontics The Academy of Prosthodontics Foundation Editorial Staff Glossary of Prosthodontic Terms Committee of the Academy of Prosthodontics Keith J. Ferro, Editor and Chairman, Glossary of Prosthodontic Terms Committee Steven M. Morgano, Copy Editor Carl F. Driscoll, Martin A. Freilich, Albert D. Guckes, Kent L. Knoernschild and Thomas J. McGarry, Members, Glossary of Prosthodontic Terms Committee PREFACE TO THE NINTH EDITION prosthodontic organizations regardless of geographic location or political affiliations. Acknowledgments are recognized by many of “The difference between the right word and the almost right the Academy fellowship, too many to name individually, with word is the difference between lightning and a lightning bug.” whom we have consulted for expert opinion. Also recognized are dMark Twain Gary Goldstein, Charles Goodacre, Albert Guckes, Steven Mor- I live down the street from Samuel Clemens’ (aka Mark Twain) gano, Stephen Rosenstiel, Clifford VanBlarcom, and Jonathan home in Hartford, Connecticut. I refer to his quotation because he Wiens for their contributions to the Glossary, which have spanned is a notable author who wrote with familiarity about our spoken many decades. We thank them for guiding us in this monumental language. Sometimes these spoken words are objectionable and project and teaching us the objectiveness and the standards for more appropriate words have evolved over time. The editors of the evidence-based dentistry to be passed on to the next generation of ninth edition of the Glossary of Prosthodontic Terms ensured that the dentists. spoken vernacular is represented, although it may be nonstandard in formal circumstances. -

Repositioning of Overerupted Upper Molar for Facilitating Lower Implant Placement with Miniscrews
CASE REPORT Repositioning of Overerupted Upper Molar for Facilitating Lower Implant Placement with Miniscrews Shafira Kurnia, Samuel Rehuel Santoso, Widyawati Sutedjo and Chiquita Prahasanti Department of Periodontology, Faculty of Dental Medicine, Universitas Airlangga, Surabaya, Indonesia ABSTRACT Loss of the mandibular first molar often leads to the overeruption of the opposing maxillary first molar, resulting in inadequate interocclusal space. In this report, two miniscrews were placed into the buccal and palatal region of the upper first molar to correct the overerupted teeth using power chains. Progress of treatment was evaluated every two weeks for five months. The clinical results showed significant intrusion while maintaining periodontal health, tooth vitality, and root length. Key Words: overerupted molar, intrusion, miniscrew INTRODUCTION The loss of mandibular first molar can lead to serious problems with remarkable clinical changes in the position of adjacent and antagonist teeth; this may require orthodontic and rehabilitation treatment due to the complexity of the resulting malocclusion. Overeruption was statistically greater in maxillary unopposed teeth than in mandibular unopposed teeth.1,2 The maxillary molar overeruption often causes difficulties upon treating antagonist tooth prostheses. The use of orthodontic miniscrew for molar intrusion to re-establish a functional posterior occlusion is an option compared to enameloplasty, intentional root canal treatment, and surgical impaction.3 This case report describes a method for regaining of vertical space by an intrusion of upper left first maxillary molar using orthodontic miniscrews and power chains for antagonist implant crown restoration. CASE REport The patient was a 42-year-old woman who came to University of Airlangga Oral and Dental Hospital with the complaint of missing lower left molars since a year ago. -

SNODENT (Systemized Nomenclature of Dentistry)
ANSI/ADA Standard No. 2000.2 Approved by ANSI: December 3, 2018 American National Standard/ American Dental Association Standard No. 2000.2 (2018 Revision) SNODENT (Systemized Nomenclature of Dentistry) 2018 Copyright © 2018 American Dental Association. All rights reserved. Any form of reproduction is strictly prohibited without prior written permission. ADA Standard No. 2000.2 - 2018 AMERICAN NATIONAL STANDARD/AMERICAN DENTAL ASSOCIATION STANDARD NO. 2000.2 FOR SNODENT (SYSTEMIZED NOMENCLATURE OF DENTISTRY) FOREWORD (This Foreword does not form a part of ANSI/ADA Standard No. 2000.2 for SNODENT (Systemized Nomenclature of Dentistry). The ADA SNODENT Canvass Committee has approved ANSI/ADA Standard No. 2000.2 for SNODENT (Systemized Nomenclature of Dentistry). The Committee has representation from all interests in the United States in the development of a standardized clinical terminology for dentistry. The Committee has adopted the standard, showing professional recognition of its usefulness in dentistry, and has forwarded it to the American National Standards Institute with a recommendation that it be approved as an American National Standard. The American National Standards Institute granted approval of ADA Standard No. 2000.2 as an American National Standard on December 3, 2018. A standard electronic health record (EHR) and interoperable national health information infrastructure require the use of uniform health information standards, including a common clinical language. Data must be collected and maintained in a standardized format, using uniform definitions, in order to link data within an EHR system or share health information among systems. The lack of standards has been a key barrier to electronic connectivity in healthcare. Together, standard clinical terminologies and classifications represent a common medical language, allowing clinical data to be effectively utilized and shared among EHR systems. -
Periodontal Care in General Practice
FEATURE CPD: ONE HOUR Periodontal care in general practice: CPD 20 important FAQs – Part two Images Plus ©Santiago Iñiguez/EyeEm/Getty questions This article has four CPD 1 2 questions attached to it which Reena Wadia and Iain L. C. Chapple summarise answers will earn you one hour of to common periodontal care questions facing dental verifiable CPD. To access the free BDA CPD hub, go to professionals in general practice. The first part of this series https://cpd.bda.org/ login/index.php contains the first set of ten FAQs and is available at: https:// go.nature.com/2Opu20F. 1: How do I manage patients with drug-infuenced Te clinical appearance varies according to the causative drug, gingival enlargement? phenytoin giving rise to a largely fbrotic and pink enlargement, Drug-infuenced gingival enlargement is now classifed as whereas calcium channel blockers are associated with a more a form of plaque-induced gingivitis according to the 2017 vascular overgrowth. Te interdental papillae become swollen with World Workshop Classifcation of periodontal diseases and a granular, pebbly surface which may enlarge further to become conditions, recognising that certain drugs may modify the nodular and lobulated as the tissues coalesce to afect the marginal infammatory-immune response to plaque accumulation and attached gingiva.5 Enlarged tissues usually have two components: and that improved plaque control reduces the enlargement.1 a fbrosis component involving excess collagen deposition, and an Gingival enlargement, or ‘overgrowth’ as it has been referred infammatory one that is initiated by bacterial plaque accumulation. to, is an overarching clinical description that does not While the two components present in the enlarged gingivae are necessitate a diagnosis based upon the histologic composition likely to be a result of distinct pathogenic processes, they are almost of the afected gingival tissues.