Proteomics Analysis of H-RAS-Mediated Oncogenic Transformation in a Genetically Defined Human Ovarian Cancer Model
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Supplemental Information to Mammadova-Bach Et Al., “Laminin Α1 Orchestrates VEGFA Functions in the Ecosystem of Colorectal Carcinogenesis”
Supplemental information to Mammadova-Bach et al., “Laminin α1 orchestrates VEGFA functions in the ecosystem of colorectal carcinogenesis” Supplemental material and methods Cloning of the villin-LMα1 vector The plasmid pBS-villin-promoter containing the 3.5 Kb of the murine villin promoter, the first non coding exon, 5.5 kb of the first intron and 15 nucleotides of the second villin exon, was generated by S. Robine (Institut Curie, Paris, France). The EcoRI site in the multi cloning site was destroyed by fill in ligation with T4 polymerase according to the manufacturer`s instructions (New England Biolabs, Ozyme, Saint Quentin en Yvelines, France). Site directed mutagenesis (GeneEditor in vitro Site-Directed Mutagenesis system, Promega, Charbonnières-les-Bains, France) was then used to introduce a BsiWI site before the start codon of the villin coding sequence using the 5’ phosphorylated primer: 5’CCTTCTCCTCTAGGCTCGCGTACGATGACGTCGGACTTGCGG3’. A double strand annealed oligonucleotide, 5’GGCCGGACGCGTGAATTCGTCGACGC3’ and 5’GGCCGCGTCGACGAATTCACGC GTCC3’ containing restriction site for MluI, EcoRI and SalI were inserted in the NotI site (present in the multi cloning site), generating the plasmid pBS-villin-promoter-MES. The SV40 polyA region of the pEGFP plasmid (Clontech, Ozyme, Saint Quentin Yvelines, France) was amplified by PCR using primers 5’GGCGCCTCTAGATCATAATCAGCCATA3’ and 5’GGCGCCCTTAAGATACATTGATGAGTT3’ before subcloning into the pGEMTeasy vector (Promega, Charbonnières-les-Bains, France). After EcoRI digestion, the SV40 polyA fragment was purified with the NucleoSpin Extract II kit (Machery-Nagel, Hoerdt, France) and then subcloned into the EcoRI site of the plasmid pBS-villin-promoter-MES. Site directed mutagenesis was used to introduce a BsiWI site (5’ phosphorylated AGCGCAGGGAGCGGCGGCCGTACGATGCGCGGCAGCGGCACG3’) before the initiation codon and a MluI site (5’ phosphorylated 1 CCCGGGCCTGAGCCCTAAACGCGTGCCAGCCTCTGCCCTTGG3’) after the stop codon in the full length cDNA coding for the mouse LMα1 in the pCIS vector (kindly provided by P. -

Discovery of Endoplasmic Reticulum Calcium Stabilizers to Rescue ER-Stressed Podocytes in Nephrotic Syndrome
Discovery of endoplasmic reticulum calcium stabilizers to rescue ER-stressed podocytes in nephrotic syndrome Sun-Ji Parka, Yeawon Kima, Shyh-Ming Yangb, Mark J. Hendersonb, Wei Yangc, Maria Lindahld, Fumihiko Uranoe, and Ying Maggie Chena,1 aDivision of Nephrology, Department of Medicine, Washington University School of Medicine, St. Louis, MO 63110; bNational Center for Advancing Translational Sciences, National Institutes of Health, Rockville, MD 20850; cDepartment of Genetics, Washington University School of Medicine, St. Louis, MO 63110; dInstitute of Biotechnology, University of Helsinki, Helsinki, Finland 00014; and eDivision of Endocrinology, Metabolism, and Lipid Research, Department of Medicine, Washington University School of Medicine, St. Louis, MO 63110 Edited by Martin R. Pollak, Beth Israel Deaconess Medical Center, Brookline, MA, and approved May 28, 2019 (received for review August 16, 2018) Emerging evidence has established primary nephrotic syndrome activating transcription factor 6 (ATF6), which act as proximal (NS), including focal segmental glomerulosclerosis (FSGS), as a sensors of ER stress. ER stress activates these sensors by inducing primary podocytopathy. Despite the underlying importance of phosphorylation and homodimerization of IRE1α and PERK/ podocyte endoplasmic reticulum (ER) stress in the pathogenesis of eukaryotic initiation factor 2α (eIF2α), as well as relocalization of NS, no treatment currently targets the podocyte ER. In our mono- ATF6 to the Golgi, where it is cleaved by S1P/S2P proteases from genic podocyte ER stress-induced NS/FSGS mouse model, the 90 kDa to the active 50-kDa ATF6 (8), leading to activation of podocyte type 2 ryanodine receptor (RyR2)/calcium release channel their respective downstream transcription factors, spliced XBP1 on the ER was phosphorylated, resulting in ER calcium leak and (XBP1s), ATF4, and p50ATF6 (8–10). -

Altered Calcium Handling in Cerebellar Purkinje Neurons with the Malignant Hyperthermia Mutation, Ryr1-Y522S/+
University of Denver Digital Commons @ DU Electronic Theses and Dissertations Graduate Studies 1-1-2011 Altered Calcium Handling in Cerebellar Purkinje Neurons with the Malignant Hyperthermia Mutation, RyR1-Y522S/+ George C. Talbott University of Denver Follow this and additional works at: https://digitalcommons.du.edu/etd Part of the Biochemistry, Biophysics, and Structural Biology Commons, and the Biology Commons Recommended Citation Talbott, George C., "Altered Calcium Handling in Cerebellar Purkinje Neurons with the Malignant Hyperthermia Mutation, RyR1-Y522S/+" (2011). Electronic Theses and Dissertations. 638. https://digitalcommons.du.edu/etd/638 This Thesis is brought to you for free and open access by the Graduate Studies at Digital Commons @ DU. It has been accepted for inclusion in Electronic Theses and Dissertations by an authorized administrator of Digital Commons @ DU. For more information, please contact [email protected],[email protected]. ALTERED CALCIUM HANDLING IN CEREBELLAR PURKINJE NEURONS WITH THE MALIGNANT HYPERTHERMIA MUTATION, RYR1 Y522S/+ __________ A Thesis Presented to The Faculty of Natural Sciences and Mathematics University of Denver __________ In Partial Fulfillment of the Requirements for the Degree Master of Science __________ by George C. Talbott June 2011 Advisor: Nancy M. Lorenzon, PhD ©Copyright by George C. Talbott 2011 All Rights Reserved Author: George C. Talbott Title: ALTERED CALCIUM HANDLING IN CEREBELLAR PURKINJE NEURONS WITH THE MALIGNANT HYPERTHERMIA MUTATION, RYR1 Y522S/+ Advisor: Nancy M. Lorenzon, PhD Degree Date: June 2011 Abstract To investigate the etiology of malignant hyperthermia and central core disease, mouse models have recently been generated and characterized (Chelu et al., 2006). These RyR Y522S/+ knock-in mutant mice provide an excellent tool to investigate calcium dysregulation, its pathological consequences, and potential therapeutic approaches. -

CCN3 and Calcium Signaling Alain Lombet1, Nathalie Planque2, Anne-Marie Bleau2, Chang Long Li2 and Bernard Perbal*2
Cell Communication and Signaling BioMed Central Review Open Access CCN3 and calcium signaling Alain Lombet1, Nathalie Planque2, Anne-Marie Bleau2, Chang Long Li2 and Bernard Perbal*2 Address: 1CNRS UMR 8078, Hôpital Marie Lannelongue, 133, Avenue de la Résistance 92350 Le PLESSIS-ROBINSON, France and 2Laboratoire d'Oncologie Virale et Moléculaire, Tour 54, Case 7048, Université Paris 7-D.Diderot, 2 Place Jussieu 75005 PARIS, France Email: Alain Lombet - [email protected]; Nathalie Planque - [email protected]; Anne-Marie Bleau - [email protected]; Chang Long Li - [email protected]; Bernard Perbal* - [email protected] * Corresponding author Published: 15 August 2003 Received: 26 June 2003 Accepted: 15 August 2003 Cell Communication and Signaling 2003, 1:1 This article is available from: http://www.biosignaling.com/content/1/1/1 © 2003 Lombet et al; licensee BioMed Central Ltd. This is an Open Access article: verbatim copying and redistribution of this article are permitted in all media for any purpose, provided this notice is preserved along with the article's original URL. Abstract The CCN family of genes consists presently of six members in human (CCN1-6) also known as Cyr61 (Cystein rich 61), CTGF (Connective Tissue Growth Factor), NOV (Nephroblastoma Overexpressed gene), WISP-1, 2 and 3 (Wnt-1 Induced Secreted Proteins). Results obtained over the past decade have indicated that CCN proteins are matricellular proteins, which are involved in the regulation of various cellular functions, such as proliferation, differentiation, survival, adhesion and migration. The CCN proteins have recently emerged as regulatory factors involved in both internal and external cell signaling. -

Myoplasmic Resting Ca2+ Regulation by Ryanodine Receptors Is
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Georgia State University Georgia State University ScholarWorks @ Georgia State University Chemistry Faculty Publications Department of Chemistry 2014 Myoplasmic resting Ca2+ regulation by ryanodine receptors is under the control of a novel Ca2+- binding region of the receptor Yanyi Chen Georgia State University, [email protected] Shenghui Xue Georgia State University, [email protected] Juan Zou Georgia State University, [email protected] Jose Lopez University of California, Davis Jenny J. Yang Georgia State University, [email protected] See next page for additional authors Follow this and additional works at: http://scholarworks.gsu.edu/chemistry_facpub Part of the Chemistry Commons Recommended Citation Chen, Yanyi; Xue, Shenghui; Zou, Juan; Lopez, Jose; Yang, Jenny J.; and Perez, Claudio, "Myoplasmic resting Ca2+ regulation by ryanodine receptors is under the control of a novel Ca2+-binding region of the receptor" (2014). Chemistry Faculty Publications. Paper 10. http://scholarworks.gsu.edu/chemistry_facpub/10 This Article is brought to you for free and open access by the Department of Chemistry at ScholarWorks @ Georgia State University. It has been accepted for inclusion in Chemistry Faculty Publications by an authorized administrator of ScholarWorks @ Georgia State University. For more information, please contact [email protected]. Authors Yanyi Chen, Shenghui Xue, Juan Zou, Jose Lopez, Jenny J. Yang, and Claudio Perez This article is available at ScholarWorks @ Georgia State University: http://scholarworks.gsu.edu/chemistry_facpub/10 Biochem. J. (2014) 460, 261–271 (Printed in Great Britain) doi:10.1042/BJ20131553 261 Myoplasmic resting Ca2 + regulation by ryanodine receptors is under the control of a novel Ca2 + -binding region of the receptor Yanyi CHEN*1, Shenghui XUE*1, Juan ZOU*, Jose R. -
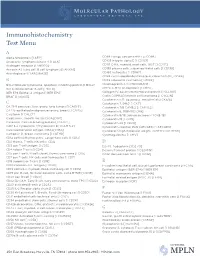
IHC Test Menu
Immunohistochemistry Test Menu A Alpha fetoprotein [I AFP] CD99 Ewings sarcoma PNET [I CD99] Anaplastic lymphoma kinase -1 [I ALK] CD103 Integrin alpha E [I CD103] Androgen receptor [I ANDRO]* CD117 C-Kit, myeloid, mast cells, GIST [I CD117] Annexin A1, hairy cell, B cell lymphoma [I ANXA1] CD138 plasma cells, subset epithelial cells [I CD138] Anti-Arginase-1 [I ARGINASE] CD163 histiocytes [I CD163] CDK4 cyclin-depdendent kinase-4, clone DCS-31 [I CDK4] B CDX2 colorectal carcinoma [I CDX2] BCL2 follicular lymphoma, apoptosis inhibiting protein [I BCL2] Chromogranin A [I CHROGRAN] BCL6 follicle center B-cell [I BCL6] CMYC C-MYC oncoprotein [I CMYC] BER EP4 Epithelial antigen [I BER EP4] Collagen IV, basement membrane protein [I CLLGIV] BRAF [I V600E] Cyclin D1/PRAD1 mantle cell lymphoma [I CYCLIN] Cytokeratin 5/6, squamous, mesothelial [I CK5/6] C Cytokeratin 7, 54kD [I CK7] CA 19-9 pancreas, liver, ovary, lung tumors [I CA19 9] Cytokeratin 7/8 CAM5.2 [I CAM 5.2] CA 125 epitheliod malignancies ovary, breast [I CA125] Cytokeratin 8, 35BH11 [I CK8] Calcitonin [I CALCT] Cytokeratin 8/18, adenocarcinoma [I CK8/18] Caldesmon, smooth muscle [I CALDSM] Cytokeratin 19 [I CK19] Calretinin; Calcium binding protein [I CALRT] Cytokeratin 20 [I CK20] CAM 5.2 Cytokeratin 7/Cytokeratin 8 [I CAM 5.2] Cytokeratin cocktail, PAN (AE1/AE3) [I AE1/AE3] Carcinoembryonic antigen (CEA) [I CEA] Cytokeratin high molecular weight; 34BE12 [I CK HMW] Cathepsin D, breast carcinoma [I CATHD] Cytomegalovirus [I CMV] CD1a cortical thymocyctes, Langerhans cells [I CD1a] -

Proteomics of Serum Extracellular Vesicles Identifies a Novel COPD Biomarker, Fibulin-3 from Elastic Fibres
ORIGINAL ARTICLE COPD Proteomics of serum extracellular vesicles identifies a novel COPD biomarker, fibulin-3 from elastic fibres Taro Koba 1, Yoshito Takeda1, Ryohei Narumi2, Takashi Shiromizu2, Yosui Nojima 3, Mari Ito3, Muneyoshi Kuroyama1, Yu Futami1, Takayuki Takimoto4, Takanori Matsuki1, Ryuya Edahiro1, Satoshi Nojima5, Yoshitomo Hayama1, Kiyoharu Fukushima1, Haruhiko Hirata1, Shohei Koyama1, Kota Iwahori1, Izumi Nagatomo1, Mayumi Suzuki1, Yuya Shirai1, Teruaki Murakami1, Kaori Nakanishi 1, Takeshi Nakatani1, Yasuhiko Suga1, Kotaro Miyake1, Takayuki Shiroyama1, Hiroshi Kida 1, Takako Sasaki6, Koji Ueda7, Kenji Mizuguchi3, Jun Adachi2, Takeshi Tomonaga2 and Atsushi Kumanogoh1 ABSTRACT There is an unmet need for novel biomarkers in the diagnosis of multifactorial COPD. We applied next-generation proteomics to serum extracellular vesicles (EVs) to discover novel COPD biomarkers. EVs from 10 patients with COPD and six healthy controls were analysed by tandem mass tag-based non-targeted proteomics, and those from elastase-treated mouse models of emphysema were also analysed by non-targeted proteomics. For validation, EVs from 23 patients with COPD and 20 healthy controls were validated by targeted proteomics. Using non-targeted proteomics, we identified 406 proteins, 34 of which were significantly upregulated in patients with COPD. Of note, the EV protein signature from patients with COPD reflected inflammation and remodelling. We also identified 63 upregulated candidates from 1956 proteins by analysing EVs isolated from mouse models. Combining human and mouse biomarker candidates, we validated 45 proteins by targeted proteomics, selected reaction monitoring. Notably, levels of fibulin-3, tripeptidyl- peptidase 2, fibulin-1, and soluble scavenger receptor cysteine-rich domain-containing protein were significantly higher in patients with COPD. -

This Electronic Thesis Or Dissertation Has Been Downloaded from Explore Bristol Research
This electronic thesis or dissertation has been downloaded from Explore Bristol Research, http://research-information.bristol.ac.uk Author: Al Ahdal, Hadil Title: Investigating the role of miR-21 in adult neurogenesis General rights Access to the thesis is subject to the Creative Commons Attribution - NonCommercial-No Derivatives 4.0 International Public License. A copy of this may be found at https://creativecommons.org/licenses/by-nc-nd/4.0/legalcode This license sets out your rights and the restrictions that apply to your access to the thesis so it is important you read this before proceeding. Take down policy Some pages of this thesis may have been removed for copyright restrictions prior to having it been deposited in Explore Bristol Research. However, if you have discovered material within the thesis that you consider to be unlawful e.g. breaches of copyright (either yours or that of a third party) or any other law, including but not limited to those relating to patent, trademark, confidentiality, data protection, obscenity, defamation, libel, then please contact [email protected] and include the following information in your message: •Your contact details •Bibliographic details for the item, including a URL •An outline nature of the complaint Your claim will be investigated and, where appropriate, the item in question will be removed from public view as soon as possible. Investigating the role of miR-21 in adult neurogenesis Hadil Mohammad Al Ahdal Faculty of Health Sciences Bristol Medical School A dissertation submitted to the University of Bristol in accordance with the requirements for award of the degree of Doctor of Philosophy in the Faculty of Health Sciences, Bristol Medical School 64,598 words Abstract MicroRNAs (miRNAs) are a class of small non-coding RNAs that act as post- transcriptional regulators and play important roles in neurodegenerative diseases and brain disorders (Nelson et al. -

Immunohistochemistry Stain Offerings
immunohistochemistry stain offerings TRUSTED PATHOLOGISTS. INVALUABLE ANSWERS.™ MARCHMAY 20172021 www.aruplab.com/ap-ihcaruplab.com/ap-ihc InformationInformation in this brochurein this brochure is current is current as of as May of March 2021. 2017. All content All content is subject is subject to tochange. change. Please contactPlease ARUPcontact ClientARUP Services Client Services at 800-522-2787 at (800) 522-2787 with any with questions any questions or concerns.or concerns. ARUP LABORATORIES As a nonprofit, academic institution of the University of Utah and its Department We believe in of Pathology, ARUP believes in collaborating, sharing and contributing to laboratory science in ways that benefit our clients and their patients. collaborating, Our test menu is one of the broadest in the industry, encompassing more sharing and than 3,000 tests, including highly specialized and esoteric assays. We offer comprehensive testing in the areas of genetics, molecular oncology, pediatrics, contributing pain management, and more. to laboratory ARUP’s clients include many of the nation’s university teaching hospitals and children’s hospitals, as well as multihospital groups, major commercial science in ways laboratories, and group purchasing organizations. We believe that healthcare should be delivered as close to the patient as possible, which is why we support that provide our clients’ efforts to be the principal healthcare provider in the communities they serve by offering highly complex assays and accompanying consultative support. the best value Offering analytics, consulting, and decision support services, ARUP provides for the patient. clients with the utilization management tools necessary to prosper in this time of value-based care. -

Calbindin-D28k and Its Role in Apoptosis: Inhibition of Caspase-3 Activity and Interaction with Pro-Caspase-3 Investigated by In-Situ FRET Microscopy
Dissertation Aus dem Physiologischen Institut Lehrstuhl: Physiologie – Zelluläre Physiologie (Biomedizinisches Zentrum München) der Ludwig-Maximilians-Universität München Vorstand: Prof. Dr. Claudia Veigel Calbindin-D28k and its role in apoptosis: Inhibition of Caspase-3 activity and interaction with Pro-Caspase-3 investigated by in-situ FRET microscopy. Dissertation zum Erwerb des Doktorgrades der Medizin an der Medizinischen Fakultät der Ludwig-Maximilians-Universität zu München vorgelegt von Johannes Lohmeier aus Bong Town, Liberia 2018 Mit Genehmigung der Medizinischen Fakultät der Universität München Berichterstatter: Prof. Dr. Michael Meyer Prof. Dr. Alexander Faussner Mitberichterstatter: Prof. Dr. Nikolaus Plesnila Prof. Dr. Dr. Bernd Sutor Dekan: Prof. Dr. med. dent. Reinhard Hickel Tag der mündlichen Prüfung: 14.06.2018 Eidesstattliche Versicherung Lohmeier, Johannes Name, Vorname Ich erkläre hiermit an Eides statt, dass ich die vorliegende Dissertation mit dem Thema Calbindin-D28k and its role in apoptosis: Inhibition of Caspase-3 activity and interaction with Pro-Caspase-3 investigated by in-situ FRET microscopy. selbständig verfasst, mich außer der angegebenen keiner weiteren Hilfsmittel bedient und alle Erkenntnisse, die aus dem Schrifttum ganz oder annähernd übernommen sind, als solche kenntlich gemacht und nach ihrer Herkunft unter Bezeichnung der Fundstelle einzeln nachgewiesen habe. Ich erkläre des Weiteren, dass die hier vorgelegte Dissertation nicht in gleicher oder in ähnlicher Form bei einer anderen Stelle zur Erlangung -

Calpain Inhibitor and Ibudilast Rescue Β Cell Functions in a Cellular Model of Wolfram Syndrome
Calpain inhibitor and ibudilast rescue β cell functions in a cellular model of Wolfram syndrome Lien D. Nguyena,b,1, Tom T. Fischera,c,1, Damien Abreud,e, Alfredo Arroyoa, Fumihiko Uranod,f, and Barbara E. Ehrlicha,b,2 aDepartment of Pharmacology, Yale University, New Haven, CT 06520; bInterdepartmental Neuroscience Program, Yale University, New Haven, CT 06520; cInstitute of Pharmacology, University of Heidelberg, 69117 Heidelberg, Germany; dDepartment of Medicine, Division of Endocrinology, Metabolism, and Lipid Research, Washington University School of Medicine, St. Louis, MO 63110; eMedical Scientist Training Program, Washington University School of Medicine, St. Louis, MO 63110; and fDepartment of Pathology and Immunology, Washington University School of Medicine, St. Louis, MO 63110 Edited by Melanie H. Cobb, University of Texas Southwestern Medical Center, Dallas, TX, and approved June 1, 2020 (received for review April 18, 2020) Wolfram syndrome is a rare multisystem disease characterized by diseases, such as Alzheimer’s disease (22), cancer progression childhood-onset diabetes mellitus and progressive neurodegener- (23), and diabetes mellitus (24, 25). ation. Most cases are attributed to pathogenic variants in a single Here we show that KO of WFS1 in rat insulinoma (INS1) cells gene, Wolfram syndrome 1 (WFS1). There currently is no disease- led to elevated resting cytosolic calcium, reduced stimulus- modifying treatment for Wolfram syndrome, as the molecular con- evoked calcium signaling, and, consequently, hypersusceptibility sequences of the loss of WFS1 remain elusive. Because diabetes to hyperglycemia and decreased glucose-stimulated insulin se- mellitus is the first diagnosed symptom of Wolfram syndrome, we cretion. Overexpression of WFS1 or WFS1’s interacting partner aimed to further examine the functions of WFS1 in pancreatic β neuronal calcium sensor-1 (NCS1) reversed the deficits observed cells in the context of hyperglycemia. -

Chemical Agent and Antibodies B-Raf Inhibitor RAF265
Supplemental Materials and Methods: Chemical agent and antibodies B-Raf inhibitor RAF265 [5-(2-(5-(trifluromethyl)-1H-imidazol-2-yl)pyridin-4-yloxy)-N-(4-trifluoromethyl)phenyl-1-methyl-1H-benzp{D, }imidazol-2- amine] was kindly provided by Novartis Pharma AG and dissolved in solvent ethanol:propylene glycol:2.5% tween-80 (percentage 6:23:71) for oral delivery to mice by gavage. Antibodies to phospho-ERK1/2 Thr202/Tyr204(4370), phosphoMEK1/2(2338 and 9121)), phospho-cyclin D1(3300), cyclin D1 (2978), PLK1 (4513) BIM (2933), BAX (2772), BCL2 (2876) were from Cell Signaling Technology. Additional antibodies for phospho-ERK1,2 detection for western blot were from Promega (V803A), and Santa Cruz (E-Y, SC7383). Total ERK antibody for western blot analysis was K-23 from Santa Cruz (SC-94). Ki67 antibody (ab833) was from ABCAM, Mcl1 antibody (559027) was from BD Biosciences, Factor VIII antibody was from Dako (A082), CD31 antibody was from Dianova, (DIA310), and Cot antibody was from Santa Cruz Biotechnology (sc-373677). For the cyclin D1 second antibody staining was with an Alexa Fluor 568 donkey anti-rabbit IgG (Invitrogen, A10042) (1:200 dilution). The pMEK1 fluorescence was developed using the Alexa Fluor 488 chicken anti-rabbit IgG second antibody (1:200 dilution).TUNEL staining kits were from Promega (G2350). Mouse Implant Studies: Biopsy tissues were delivered to research laboratory in ice-cold Dulbecco's Modified Eagle Medium (DMEM) buffer solution. As the tissue mass available from each biopsy was limited, we first passaged the biopsy tissue in Balb/c nu/Foxn1 athymic nude mice (6-8 weeks of age and weighing 22-25g, purchased from Harlan Sprague Dawley, USA) to increase the volume of tumor for further implantation.