NIH Public Access Author Manuscript Nat Genet
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Alfred Nobel
www.bibalex.org/bioalex2004conf The BioVisionAlexandria 2004 Conference Newsletter November 2003 Volume 1, Issue 2 BioVisionAlexandria ALFRED NOBEL 2004 aims to celebrate the The inventor, the industrialist outstanding scientists and scholars, in a he Nobel Prize is one of the highest distinctions recognized, granting its winner century dominated by instant fame. However, many do not know the interesting history and background technological and T that led to this award. scientific revolutions, through its It all began with a chemist, known as Alfred Nobel, born in Stockholm, Sweden in 1833. Nobel Day on 3 April Alfred Nobel moved to Russia when he was eight, where his father, Immanuel Nobel, 2004! started a successful mechanical workshop. He provided equipment for the Russian Army and designed naval mines, which effectively prevented the British Royal Navy from moving within firing range of St. Petersburg during the Crimean War. Immanuel Nobel was also a pioneer in the manufacture of arms, and in designing steam engines. INSIDE Scientific awards .........3 Immanuel’s success enabled him to Alfred met Ascanio Sobrero, the Italian Confirmed laureates ....4 Lady laureates ............7 provide his four sons with an excellent chemist who had invented Nitroglycerine education in natural sciences, languages three years earlier. Nitroglycerine, a and literature. Alfred, at an early age, highly explosive liquid, was produced by acquired extensive literary knowledge, mixing glycerine with sulfuric and nitric mastering many foreign languages. His acid. It was an invention that triggered a Nobel Day is interest in science, especially chemistry, fascination in the young scientist for many dedicated to many of was also apparent. -

FORMATO PDF Ranking Instituciones No Acadã©Micas Por Sub Ã
Ranking Instituciones No Académicas por sub área OCDE 2020 3. Ciencias Médicas y de la Salud > 3.02 Medicina Clínica PAÍS INSTITUCIÓN RANKING PUNTAJE USA VA Boston Healthcare System 1 5,000 FRANCE Assistance Publique Hopitaux Paris (APHP) 2 5,000 USA UTMD Anderson Cancer Center 3 5,000 USA Mayo Clinic 4 5,000 USA Memorial Sloan Kettering Cancer Center 5 5,000 USA Dana-Farber Cancer Institute 6 5,000 USA Massachusetts General Hospital 7 5,000 FRANCE Institut National de la Sante et de la Recherche Medicale (Inserm) 8 5,000 USA National Institutes of Health (NIH) - USA 9 5,000 FRANCE UNICANCER 10 5,000 USA Harvard School of Dental Medicine 11 5,000 CANADA University Health Network Toronto 12 5,000 USA Cleveland Clinic Foundation 13 5,000 USA Johns Hopkins Medicine 14 5,000 FRANCE Gustave Roussy 15 5,000 NETHERLANDS Erasmus University Medical Center 16 5,000 GERMANY Helmholtz Association 17 5,000 NETHERLANDS Academic Medical Center Amsterdam 18 5,000 SPAIN CIBER - Centro de Investigacion Biomedica en Red 19 5,000 USA Beth Israel Deaconess Medical Center 20 5,000 SWITZERLAND Roche Holding 21 5,000 CANADA Princess Margaret Cancer Centre 22 5,000 USA H Lee Moffitt Cancer Center & Research Institute 23 5,000 SPAIN Hospital Universitari Vall d'Hebron 24 5,000 BELGIUM University Hospital Leuven 25 5,000 USA NIH National Cancer Institute (NCI) 26 5,000 SPAIN Hospital Clinic de Barcelona 27 5,000 USA Bristol-Myers Squibb 28 5,000 USA Merck & Company 29 5,000 UNITED KINGDOM Royal Marsden NHS Foundation Trust 30 5,000 SOUTH KOREA Seoul National University -

Balcomk41251.Pdf (558.9Kb)
Copyright by Karen Suzanne Balcom 2005 The Dissertation Committee for Karen Suzanne Balcom Certifies that this is the approved version of the following dissertation: Discovery and Information Use Patterns of Nobel Laureates in Physiology or Medicine Committee: E. Glynn Harmon, Supervisor Julie Hallmark Billie Grace Herring James D. Legler Brooke E. Sheldon Discovery and Information Use Patterns of Nobel Laureates in Physiology or Medicine by Karen Suzanne Balcom, B.A., M.L.S. Dissertation Presented to the Faculty of the Graduate School of The University of Texas at Austin in Partial Fulfillment of the Requirements for the Degree of Doctor of Philosophy The University of Texas at Austin August, 2005 Dedication I dedicate this dissertation to my first teachers: my father, George Sheldon Balcom, who passed away before this task was begun, and to my mother, Marian Dyer Balcom, who passed away before it was completed. I also dedicate it to my dissertation committee members: Drs. Billie Grace Herring, Brooke Sheldon, Julie Hallmark and to my supervisor, Dr. Glynn Harmon. They were all teachers, mentors, and friends who lifted me up when I was down. Acknowledgements I would first like to thank my committee: Julie Hallmark, Billie Grace Herring, Jim Legler, M.D., Brooke E. Sheldon, and Glynn Harmon for their encouragement, patience and support during the nine years that this investigation was a work in progress. I could not have had a better committee. They are my enduring friends and I hope I prove worthy of the faith they have always showed in me. I am grateful to Dr. -
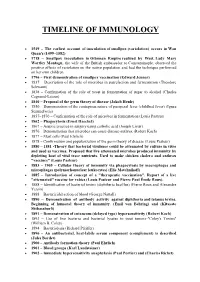
Timeline of Immunology
TIMELINE OF IMMUNOLOGY 1549 – The earliest account of inoculation of smallpox (variolation) occurs in Wan Quan's (1499–1582) 1718 – Smallpox inoculation in Ottoman Empire realized by West. Lady Mary Wortley Montagu, the wife of the British ambassador to Constantinople, observed the positive effects of variolation on the native population and had the technique performed on her own children. 1796 – First demonstration of smallpox vaccination (Edward Jenner) 1837 – Description of the role of microbes in putrefaction and fermentation (Theodore Schwann) 1838 – Confirmation of the role of yeast in fermentation of sugar to alcohol (Charles Cagniard-Latour) 1840 – Proposal of the germ theory of disease (Jakob Henle) 1850 – Demonstration of the contagious nature of puerperal fever (childbed fever) (Ignaz Semmelweis) 1857–1870 – Confirmation of the role of microbes in fermentation (Louis Pasteur) 1862 – Phagocytosis (Ernst Haeckel) 1867 – Aseptic practice in surgery using carbolic acid (Joseph Lister) 1876 – Demonstration that microbes can cause disease-anthrax (Robert Koch) 1877 – Mast cells (Paul Ehrlich) 1878 – Confirmation and popularization of the germ theory of disease (Louis Pasteur) 1880 – 1881 -Theory that bacterial virulence could be attenuated by culture in vitro and used as vaccines. Proposed that live attenuated microbes produced immunity by depleting host of vital trace nutrients. Used to make chicken cholera and anthrax "vaccines" (Louis Pasteur) 1883 – 1905 – Cellular theory of immunity via phagocytosis by macrophages and microphages (polymorhonuclear leukocytes) (Elie Metchnikoff) 1885 – Introduction of concept of a "therapeutic vaccination". Report of a live "attenuated" vaccine for rabies (Louis Pasteur and Pierre Paul Émile Roux). 1888 – Identification of bacterial toxins (diphtheria bacillus) (Pierre Roux and Alexandre Yersin) 1888 – Bactericidal action of blood (George Nuttall) 1890 – Demonstration of antibody activity against diphtheria and tetanus toxins. -

Journal of Immunodeficiency & Disorders
Kobayashi, J Immunodefic Disor 2012, 1:1 http://dx.doi.org/10.4172/2324-853X.1000e102 Journal of Immunodeficiency & Disorders Editorial a SciTechnol journal MHC class II genes [5]. Interestingly, CIITA can activate not only NLRC5/CITA: A Novel the promoters of MHC class II genes but also of MHC class I genes at least in in vitro experiments [6-10]. However, mutations in the CIITA Regulator of Class I Major gene in human BLS patients and deficiency of CIITA in mice did not show any reduction of MHC class I [2,11-14]. This led to the obvious Histocompatibility Complex assumption that a similar unknown transactivator should exist for the Genes regulation of expression of MHC class I genes. Koichi S. Kobayashi1* Seventeen years after the discovery of CIITA, the MHC class I transactivator was identified. Similar to CIITA, it is a member of In 1936, Peter Gorer reported one of the most significant work NLR (nucleotide binding domain-leucine rich repeats containing) in the history of immunology; the first identification of alloantigen family of proteins, called NLRC5 [15,16]. NLRC5 has unusually long using serum from immunized rabbits and his own blood [1]. This led leucine-rich repeats and its N-terminal structure was different from to the discovery of the Major Histocompatibility Complex (MHC) that of CIITA [16,17]. Because of this, these two proteins look very different at first sight. However, upon detailed phylogenetic analysis by his coworker, George Snell at the Jackson Laboratories. After of the nucleotide binding domain, it became clear that NLRC5 is the three quarters of a century, this year, 5 laboratories independently most closely related to CIITA among all NLR proteins [15,18]. -
Nobel Laureates in Physiology Or Medicine
All Nobel Laureates in Physiology or Medicine 1901 Emil A. von Behring Germany ”for his work on serum therapy, especially its application against diphtheria, by which he has opened a new road in the domain of medical science and thereby placed in the hands of the physician a victorious weapon against illness and deaths” 1902 Sir Ronald Ross Great Britain ”for his work on malaria, by which he has shown how it enters the organism and thereby has laid the foundation for successful research on this disease and methods of combating it” 1903 Niels R. Finsen Denmark ”in recognition of his contribution to the treatment of diseases, especially lupus vulgaris, with concentrated light radiation, whereby he has opened a new avenue for medical science” 1904 Ivan P. Pavlov Russia ”in recognition of his work on the physiology of digestion, through which knowledge on vital aspects of the subject has been transformed and enlarged” 1905 Robert Koch Germany ”for his investigations and discoveries in relation to tuberculosis” 1906 Camillo Golgi Italy "in recognition of their work on the structure of the nervous system" Santiago Ramon y Cajal Spain 1907 Charles L. A. Laveran France "in recognition of his work on the role played by protozoa in causing diseases" 1908 Paul Ehrlich Germany "in recognition of their work on immunity" Elie Metchniko France 1909 Emil Theodor Kocher Switzerland "for his work on the physiology, pathology and surgery of the thyroid gland" 1910 Albrecht Kossel Germany "in recognition of the contributions to our knowledge of cell chemistry made through his work on proteins, including the nucleic substances" 1911 Allvar Gullstrand Sweden "for his work on the dioptrics of the eye" 1912 Alexis Carrel France "in recognition of his work on vascular suture and the transplantation of blood vessels and organs" 1913 Charles R. -

History of Clinical Transplantation
World J. Surg. 2.:&.759-782.2000 DOl: 10.1007/s00268001012':& History of Clinical Transplantation Thomas E. Starzl, M.D., Ph.D. Thomas E. Starzl Transplantation Institute. University of Pittsburgh Medical Center. Falk Clinic. 4th Floor, 3601 Fifth Avenue. Pittsburgh. Pennsylvania 15213. USA Abstract. The emergence of transplantation has seen the development of to donor strain tissues was retained as the recipient animals grew increasingly potent immunosuppressive agents, progressively better to adult life, whereas normal reactivity evolved to third party methods of tissue and organ preservation. refinements in histocompati grafts and other kinds of antigens. bility matching. and numerous innovations in surgical techniques. Such efforts in combination ultimately made it possible to successfully engraft This was not the first demonstration that tolerance could be all of the organs and bone marrow cells in humans. At a more fundamen· deliberately produced. Analogous to the neonatal transplant tal level, however, the transplantation enterprise hinged on two seminal model. Traub [6] showed in 1936 that the lymphocytic choriomen turning points. The first was the recognition by Billingham. Brent, and Medawar in 1953 that it was possible to induce chimerism·associated igitis virus (LCMV) persisted after transplacental infection of the neonatal tolerance deliberately. This discovery escalated over the next 15 embryo from the mother or. alternatively. by injection into new years to the first successful bone marrow transplantations in humans in born mice. Howevt!r, when the mice were infected as adults. the 1968. The second turning point was the demonstration during the early virus was eliminated immunologicully. Similar observations had 1960s that canine and human organ allografts could self·induce tolerance been made in experimental tumor models. -
Ssfaoggi 201306
SOCIETA’ DI SCIENZE FARMACOLOGICHE APPLICATE SOCIETY FOR APPLIED PHARMACOLOGICAL SSFAoggi SCIENCES Notiziario di Medicina Farmaceutica Giugno 2013 Bimestrale della Società di Scienze Farmacologiche Applicate Fondata nel 1964 numero 37 Dove sono i nuovi antibiotici? Sommario: La comunità mondiale sta correndo un grosso rischio: questo ci ricordano due editoriali, Editoriale 1 pubblicati su The Lancet e sul British Medical Journal, che riportiamo alle pagine 21 e 22. La resistenza agli antibiotici è un grave problema: The Lancet ci ricorda che fu addirittura Novità in Farmacovigilanza messa in evidenza dallo stesso Alexander Fleming nel 1945, il quale temeva che l’abuso Parte prima 2 della penicillina potesse selezionare ceppi resistenti. Il British Medical Journal evidenzia che molte pratiche mediche e chirurgiche (dall’uso Novità in Farmacovigilanza della chemioterapia agli interventi invasivi in ortopedia e cardiochirurgia) sono possibili Parte seconda 4 grazie alla profilassi con antibiotici. E quindi, la resistenza agli antibiotici non è un solo un problema degli infettivologi, ma sta diventando un problema dei chirurghi, degli oncologi, e Il Decreto Balduzzi 6 di tutto il sistema sanitario. Alcune previsioni sono drammatiche: l’intervento di protesi dell’anca, che è diventato una Farmaci a brevetto scaduto 12 routine per la popolazione anziana, potrebbe essere colpito in modo significativo da com- plicanze infettive, passando dall’1% dei pazienti di oggi fino al 40%-50% dei pazienti nel Affari Istituzionali 12 prossimo futuro, con oltre un terzo di essi in pericolo di vita. Uno scenario davvero preoc- 5a Edizione Master Bicocca 13 cupante. Di fronte a queste previsioni, che ci vengono ormai ripetute ad intervalli regolari, stupisce Master Bicocca 2013: i numeri 13 la mancanza di incentivi per la ricerca di nuovi antibiotici. -

Brief History of Important Immunologic Discoveries and Developments
Brief History of Important Immunologic Discoveries and Developments Year Event Author(s) 1798 Cowpox vaccination Edward Jenner 1866 Wound disinfection Joseph Lister 1876 Discovery of B. antracis, foundation of Robert Koch bacteriology 1880 Discovery of attenuated vaccine by Louis Pasteur invitro passages 1883 Phagocytosis, cellular immunity theory Elie I. I. Metchnikoff 1888 Discovery of bacterial toxins P. P. Emile Roux and Alexandre E. J. Y ersin 1890 Discovery of antitoxins, foundation of Emil A. von Behring and serotherapy Shibasaburo Kitasato 1894 Immunologic bacteriolysis Richard F. J. Pfeiffer and Vasily I. Isaeff 1894 Discovery of antibody and complement Jules J.B. V. Bordet activity as the active factors in bacteriolysis 1896 Discovery of specific agglutination Herbert E. Durham and Max von Gruber 1896 Agglutination test for the diagnosis of Georges F. I. Widal and typhoid (Widal test) Jean-Marie-Athanase Sicard 1900 Formulation of side-chain theory of anti- Paul Ehrlich body formation 1900 Discovery of A, B, 0 blood groups Karl Landsteiner 1900 Development of complement fixation Jules J.B. V. Bordet and reaction Octave Gengou 1902 Discovery of anaphylaxis Charles R. Richet and Paul Portier 1903 Local anaphylaxis due to antibody- Nicholas M. Arthus antigen complex: Arthus reaction 1903 Discovery of opsonization Almroth E. Wright and Steward R. Douglas 440 Brief History of Important Immunologic Discoveries and Developments Year Event Author(s) 1905 Description of serum sickness Clemens von Pirquet and Bela Schick 1910 Introduction of salvarsan, later neo- Paul Ehrlich and Sahachiro Hata salvarsan, foundation of chemotherapy of infections 1910 Development of anaphylaxis test William Schultz (Schultz-Dale) 1914 Formulation of genetic theory of tumor Clarence C. -

List of Nobel Laureates 1
List of Nobel laureates 1 List of Nobel laureates The Nobel Prizes (Swedish: Nobelpriset, Norwegian: Nobelprisen) are awarded annually by the Royal Swedish Academy of Sciences, the Swedish Academy, the Karolinska Institute, and the Norwegian Nobel Committee to individuals and organizations who make outstanding contributions in the fields of chemistry, physics, literature, peace, and physiology or medicine.[1] They were established by the 1895 will of Alfred Nobel, which dictates that the awards should be administered by the Nobel Foundation. Another prize, the Nobel Memorial Prize in Economic Sciences, was established in 1968 by the Sveriges Riksbank, the central bank of Sweden, for contributors to the field of economics.[2] Each prize is awarded by a separate committee; the Royal Swedish Academy of Sciences awards the Prizes in Physics, Chemistry, and Economics, the Karolinska Institute awards the Prize in Physiology or Medicine, and the Norwegian Nobel Committee awards the Prize in Peace.[3] Each recipient receives a medal, a diploma and a monetary award that has varied throughout the years.[2] In 1901, the recipients of the first Nobel Prizes were given 150,782 SEK, which is equal to 7,731,004 SEK in December 2007. In 2008, the winners were awarded a prize amount of 10,000,000 SEK.[4] The awards are presented in Stockholm in an annual ceremony on December 10, the anniversary of Nobel's death.[5] As of 2011, 826 individuals and 20 organizations have been awarded a Nobel Prize, including 69 winners of the Nobel Memorial Prize in Economic Sciences.[6] Four Nobel laureates were not permitted by their governments to accept the Nobel Prize. -

Printwhatyoulike on ノーベル生理学・医学賞
ノーベル生理学・医学賞 出典: フリー百科事典『ウィキペディア(Wikipedia)』 ノーベル賞 > ノーベル生理学・医学賞 ノーベル生理学・医学賞(ノーベルせいりがく・いがくしょう)はノーベル賞6部門のうちの1つ。「(動物)生理学及び医学の分野で 最も重要な発見を行なった」人に与えられる。選考はカロリンスカ研究所のノーベル賞委員会が行う。 歴代受賞者 [編集] 年度 受賞者名 国籍 受賞理由 エミール・アドルフ・フォン・ 血清療法の研究、特にジフテリアに対するものによって、 1901 ベーリング ドイツ帝国 医学の新しい分野を切り開き、生理学者の手に疾病や死 年 Emil Adolf von Behring に勝利しうる手段を提供したこと 1902 ロナルド・ロス マラリアの研究によってその感染経路を示し、疾病やそれ イギリス 年 Ronald Ross に対抗する手段に関する研究の基礎を築いたこと 1903 ニールス・フィンセン 疾病の治療法への寄与、特に尋常性狼瘡への光線治療法 デンマーク 年 Niels Ryberg Finsen によって、医学の新しい領域を開拓したこと 1904 イワン・パブロフ 消化生理の研究により、その性質に関する知見を転換し ロシア連邦 年 Ivan Petrovich Pavlov 拡張したこと 1905 ロベルト・コッホ ドイツ帝国 結核に関する研究と発見 年 Robert Koch カミッロ・ゴルジ イタリア王国 Camillo Golgi 1906 神経系の構造研究 年 サンティアゴ・ラモン・イ・カ ハール スペイン Santiago Ramon y Cajal シャルル・ルイ・アルフォンス・ 1907 ラヴラン フランス 疾病発生における原虫類の役割に関する研究 年 Charles Louis Alphonse Laveran パウル・エールリヒ ドイツ帝国 1908 Paul Ehrlich 免疫の研究 年 イリヤ・メチニコフ ロシア連邦 Ilya Ilyich Mechnikov 1909 エーミール・コッハー スイス 甲状腺の生理学、病理学および外科学的研究 年 Emil Theodor Kocher 1910 アルブレヒト・コッセル 核酸物質を含む、タンパク質に関する研究による細胞化学 ドイツ帝国 年 Albrecht Kossel の知見への寄与 1911 アルヴァル・グルストランド スウェーデン 眼の屈折機能に関する研究 年 Allvar Gullstrand 1912 アレクシス・カレル フランス 血管縫合および臓器の移植に関する研究 年 Alexis Carrel 1913 シャルル・ロベール・リシェ フランス アナフィラキシーの研究 年 Charles Robert Richet 1914 ローベルト・バーラーニ オーストリア=ハンガリー 内耳系の生理学および病理学に関する研究 年 Robert Bárány 帝国 1915 受賞者なし 年 1916 受賞者なし 年 1917 受賞者なし 年 1918 受賞者なし 年 1919 ジュール・ボルデ ベルギー 免疫に関する諸発見 年 Jules Bordet アウグスト・クローグ 1920 Schack August Steenberg デンマーク 毛細血管運動に関する調整機構の発見 年 Krogh 1921 受賞者なし 年 アーチボルド・ヒル イギリス 筋肉中の熱生成に関する発見 1922 Archibald Vivian Hill 年 オットー・マイヤーホフ ドイツ 筋肉における乳酸生成と酸素消費の固定的関連の発見 Otto Fritz Meyerhof -

Image-Brochure-LNLM-2020-LQ.Pdf
NOBEL LAUREATES PARTICIPATING IN LINDAU EVENTS SINCE 1951 Peter Agre | George A. Akerlof | Kurt Alder | Zhores I. Alferov | Hannes Alfvén | Sidney Altman | Hiroshi Amano | Philip W. Anderson | Christian B. Anfinsen | Edward V. Appleton | Werner Arber | Frances H. Arnold | Robert J. Aumann | Julius Axelrod | Abhijit Banerjee | John Bardeen | Barry C. Barish | Françoise Barré-Sinoussi | Derek H. R. Barton | Nicolay G. Basov | George W. Beadle | J. Georg Bednorz | Georg von Békésy |Eric Betzig | Bruce A. Beutler | Gerd Binnig | J. Michael Bishop | James W. Black | Elizabeth H. Blackburn | Patrick M. S. Blackett | Günter Blobel | Konrad Bloch | Felix Bloch | Nicolaas Bloembergen | Baruch S. Blumberg | Niels Bohr | Max Born | Paul Boyer | William Lawrence Bragg | Willy Brandt | Walter H. Brattain | Bertram N. Brockhouse | Herbert C. Brown | James M. Buchanan Jr. | Frank Burnet | Adolf F. Butenandt | Melvin Calvin Thomas R. Cech | Martin Chalfie | Subrahmanyan Chandrasekhar | Pavel A. Cherenkov | Steven Chu | Aaron Ciechanover | Albert Claude | John Cockcroft | Claude Cohen- Tannoudji | Leon N. Cooper | Carl Cori | Allan M. Cormack | John Cornforth André F. Cournand | Francis Crick | James Cronin | Paul J. Crutzen | Robert F. Curl Jr. | Henrik Dam | Jean Dausset | Angus S. Deaton | Gérard Debreu | Petrus Debye | Hans G. Dehmelt | Johann Deisenhofer Peter A. Diamond | Paul A. M. Dirac | Peter C. Doherty | Gerhard Domagk | Esther Duflo | Renato Dulbecco | Christian de Duve John Eccles | Gerald M. Edelman | Manfred Eigen | Gertrude B. Elion | Robert F. Engle III | François Englert | Richard R. Ernst Gerhard Ertl | Leo Esaki | Ulf von Euler | Hans von Euler- Chelpin | Martin J. Evans | John B. Fenn | Bernard L. Feringa Albert Fert | Ernst O. Fischer | Edmond H. Fischer | Val Fitch | Paul J.