Today's Topic
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Dextromethorphan Attenuates Sensorineural Hearing Loss in an Animal Model and Population-Based Cohort Study
International Journal of Environmental Research and Public Health Article Dextromethorphan Attenuates Sensorineural Hearing Loss in an Animal Model and Population-Based Cohort Study Hsin-Chien Chen 1,* , Chih-Hung Wang 1,2 , Wu-Chien Chien 3,4 , Chi-Hsiang Chung 3,4, Cheng-Ping Shih 1, Yi-Chun Lin 1,2, I-Hsun Li 5,6, Yuan-Yung Lin 1,2 and Chao-Yin Kuo 1 1 Department of Otolaryngology-Head and Neck Surgery, Tri-Service General Hospital, National Defense Medical Center, Taipei 114, Taiwan; [email protected] (C.-H.W.); [email protected] (C.-P.S.); [email protected] (Y.-C.L.); [email protected] (Y.-Y.L.); [email protected] (C.-Y.K.) 2 Graduate Institute of Medical Sciences, National Defense Medical Center, Taipei 114, Taiwan 3 School of Public Health, National Defense Medical Center, Taipei 114, Taiwan; [email protected] (W.-C.C.); [email protected] (C.-H.C.) 4 Department of Medical Research, Tri-Service General Hospital, National Defense Medical Center, Taipei 114, Taiwan 5 Department of Pharmacy Practice, Tri-Service General Hospital, National Defense Medical Center, Taipei 114, Taiwan; [email protected] 6 School of Pharmacy, National Defense Medical Center, Taipei 114, Taiwan * Correspondence: [email protected]; Tel.: +886-2-8792-7192; Fax: +886-2-8792-7193 Received: 31 July 2020; Accepted: 28 August 2020; Published: 31 August 2020 Abstract: The effect of dextromethorphan (DXM) use in sensorineural hearing loss (SNHL) has not been fully examined. We conducted an animal model and nationwide retrospective matched-cohort study to explore the association between DXM use and SNHL. -

Hallucinogens
Hallucinogens What are hallucinogens? Hallucinogens are a diverse group of drugs that alter a person’s awareness of their surroundings as well as their own thoughts and feelings. They are commonly split into two categories: classic hallucinogens (such as LSD) and dissociative drugs (such as PCP). Both types of hallucinogens can cause hallucinations, or sensations and images that seem real though they are not. Additionally, dissociative drugs can cause users to feel out of control or disconnected from their body and environment. Some hallucinogens are extracted from plants or mushrooms, and some are synthetic (human- made). Historically, people have used hallucinogens for religious or healing rituals. More recently, people report using these drugs for social or recreational purposes, including to have fun, deal with stress, have spiritual experiences, or just to feel different. Common classic hallucinogens include the following: • LSD (D-lysergic acid diethylamide) is one of the most powerful mind-altering chemicals. It is a clear or white odorless material made from lysergic acid, which is found in a fungus that grows on rye and other grains. LSD has many other street names, including acid, blotter acid, dots, and mellow yellow. • Psilocybin (4-phosphoryloxy-N,N- dimethyltryptamine) comes from certain types of mushrooms found in tropical and subtropical regions of South America, Mexico, and the United States. Some common names for Blotter sheet of LSD-soaked paper squares that users psilocybin include little smoke, magic put in their mouths. mushrooms, and shrooms. Photo by © DEA • Peyote (mescaline) is a small, spineless cactus with mescaline as its main ingredient. Peyote can also be synthetic. -
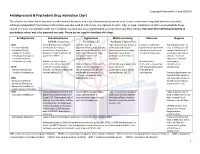
Antidepressant & Psychedelic Drug Interaction Chart
Copyright Psychedelic School 8/2020 Antidepressant & Psychedelic Drug Interaction Chart This chart is not intended to be used to make medical decisions and is for informational purposes only. It was constructed using data whenever possible, although extrapolation from known information was also used to inform risk. Any decision to start, stop, or taper medication and/or use psychedelic drugs should be made in conjunction with your healthcare provider(s). It is recommended to not perform any illicit activity. This chart the intellectual property of psychedelic school and is for personal use only. Please do not copy or distribute this chart. Antidepressant Phenethylamines Tryptamines MAOI-containing Ketamine Ibogaine -MDMA, mescaline -Psilocybin, LSD -Ayahuasca, Syrian Rue SSRIs Taper & discontinue at least 2 Consider taper & Taper & discontinue at least 2 Has been studied and Taper & discontinue at · Paroxetine (Paxil) weeks prior (all except discontinuation at least 2 weeks weeks prior (all except found effective both with least 2 weeks prior (all · Sertraline (Zoloft) fluoxetine) or 6 weeks prior prior (all except fluoxetine) or 6 fluoxetine) or 6 weeks prior and without concurrent except fluoxetine) or 6 · Citalopram (Celexa) (fluoxetine only) due to loss of weeks prior (fluoxetine only) (fluoxetine only) due to use of antidepressants weeks prior (fluoxetine · Escitalopram (Lexapro) psychedelic effect due to potential loss of potential risk of serotonin only) due to risk of · Fluxoetine (Prozac) psychedelic effect syndrome additive QTc interval · Fluvoxamine (Luvox) MDMA is unable to cause Recommended prolongation, release of serotonin when the Chronic antidepressant use may Life threatening toxicities can to be used in conjunction arrhythmias, or SPARI serotonin reuptake pump is result in down-regulation of occur with these with oral antidepressants cardiotoxicity · Vibryyd (Vilazodone) blocked. -

Janssen Research & Development, LLC Advisory Committee Briefing
Janssen Research & Development, LLC Advisory Committee Briefing Document Esketamine Nasal Spray for Patients with Treatment-resistant Depression JNJ-54135419 (esketamine) Status: Approved Date: 16 January 2019 Prepared by: Janssen Research & Development, LLC EDMS number: EDMS-ERI-171521650, 1.0 ADVISORY COMMITTEE BRIEFING MATERIALS: AVAILABLE FOR PUBLIC RELEASE 1 Status: Approved, Date: 16 January 2019 JNJ-54135419 (esketamine) Treatment-resistant Depression Advisory Committee Briefing Document GUIDE FOR REVIEWERS This briefing document provides 3 levels of review with increasing levels of detail: The Executive Overview (Section 1, starting on page 11) provides a narrative summarizing the disease, need for novel treatments, key development program characteristics for esketamine nasal spray, study results, and conclusions. References are made to the respective supporting sections in the core document. The core document (Section 2 to Section 11, starting on page 30) includes detailed summaries and discussion in support of the Executive Overview. The appendices (starting on page 180) provide additional or more detailed information to complement brief descriptions provided in sections of the core document (e.g., demographic and baseline characteristics of the study populations, additional efficacy analyses in the Phase 3 studies, statistical methods). These appendices are referenced in the core document when relevant. This review structure allows review at varying levels of detail; however, reviewers who read at multiple levels will necessarily -

Psychedelics in Psychiatry: Neuroplastic, Immunomodulatory, and Neurotransmitter Mechanismss
Supplemental Material can be found at: /content/suppl/2020/12/18/73.1.202.DC1.html 1521-0081/73/1/202–277$35.00 https://doi.org/10.1124/pharmrev.120.000056 PHARMACOLOGICAL REVIEWS Pharmacol Rev 73:202–277, January 2021 Copyright © 2020 by The Author(s) This is an open access article distributed under the CC BY-NC Attribution 4.0 International license. ASSOCIATE EDITOR: MICHAEL NADER Psychedelics in Psychiatry: Neuroplastic, Immunomodulatory, and Neurotransmitter Mechanismss Antonio Inserra, Danilo De Gregorio, and Gabriella Gobbi Neurobiological Psychiatry Unit, Department of Psychiatry, McGill University, Montreal, Quebec, Canada Abstract ...................................................................................205 Significance Statement. ..................................................................205 I. Introduction . ..............................................................................205 A. Review Outline ........................................................................205 B. Psychiatric Disorders and the Need for Novel Pharmacotherapies .......................206 C. Psychedelic Compounds as Novel Therapeutics in Psychiatry: Overview and Comparison with Current Available Treatments . .....................................206 D. Classical or Serotonergic Psychedelics versus Nonclassical Psychedelics: Definition ......208 Downloaded from E. Dissociative Anesthetics................................................................209 F. Empathogens-Entactogens . ............................................................209 -

The Effects of Ketamine on Dopaminergic Function: Meta-Analysis and Review of the Implications for Neuropsychiatric Disorders
OPEN Molecular Psychiatry (2018) 23, 59–69 www.nature.com/mp REVIEW The effects of ketamine on dopaminergic function: meta-analysis and review of the implications for neuropsychiatric disorders M Kokkinou1,2, AH Ashok1,2,3 and OD Howes1,2,3 Ketamine is a non-competitive antagonist at the N-methyl-D-aspartate receptor. It has recently been found to have antidepressant effects and is a drug of abuse, suggesting it may have dopaminergic effects. To examine the effect of ketamine on the dopamine systems, we carried out a systematic review and meta-analysis of dopamine measures in the rodent, human and primate brain following acute and chronic ketamine administration relative to a drug-free baseline or control condition. Systematic search of PubMed and PsychInfo electronic databases yielded 40 original peer-reviewed studies. There were sufficient rodent studies of the acute effects of ketamine at sub-anaesthetic doses for meta-analysis. Acute ketamine administration in rodents is associated with significantly increased dopamine levels in the cortex (Hedge’s g = 1.33, Po0.01), striatum (Hedge’s g = 0.57, Po0.05) and the nucleus accumbens (Hedge’s g = 1.30, Po0.05) compared to control conditions, and 62–180% increases in dopamine neuron population activity. Sub-analysis indicated elevations were more marked in in vivo (g = 1.93) than ex vivo (g = 0.50) studies. There were not enough studies for meta-analysis in other brain regions studied (hippocampus, ventral pallidum and cerebellum), or of the effects of chronic ketamine administration, although consistent increases in cortical dopamine levels (from 88 to 180%) were reported in the latter studies. -

Rxoutlook® 1St Quarter 2019
® RxOutlook 1st Quarter 2020 optum.com/optumrx a RxOutlook 1st Quarter 2020 Orphan drugs continue to feature prominently in the drug development pipeline In 1983 the Orphan Drug Act was signed into law. Thirty seven years later, what was initially envisioned as a minor category of drugs has become a major part of the drug development pipeline. The Orphan Drug Act was passed by the United States Congress in 1983 in order to spur drug development for rare conditions with high unmet need. The legislation provided financial incentives to manufacturers if they could demonstrate that the target population for their drug consisted of fewer than 200,000 persons in the United States, or that there was no reasonable expectation that commercial sales would be sufficient to recoup the developmental costs associated with the drug. These “Orphan Drug” approvals have become increasingly common over the last two decades. In 2000, two of the 27 (7%) new drugs approved by the FDA had Orphan Designation, whereas in 2019, 20 of the 48 new drugs (42%) approved by the FDA had Orphan Designation. Since the passage of the Orphan Drug Act, 37 years ago, additional regulations and FDA designations have been implemented in an attempt to further expedite drug development for certain serious and life threatening conditions. Drugs with a Fast Track designation can use Phase 2 clinical trials to support FDA approval. Drugs with Breakthrough Therapy designation can use alternative clinical trial designs instead of the traditional randomized, double-blind, placebo-controlled trial. Additionally, drugs may be approved via the Accelerated Approval pathway using surrogate endpoints in clinical trials rather than clinical outcomes. -

WE WANT to HEAR from YOU Abarca Created the Drug Intelligence Newsletter to Keep Our Clients and Partners Apprised of Critical and Impending Changes to Patient Care
April 2019 WE WANT TO HEAR FROM YOU Abarca created the Drug Intelligence Newsletter to keep our clients and partners apprised of critical and impending changes to patient care. If there are any topics that you would like to learn more about, or feedback for our Clinical Team, please contact David Capó, Clinical Epidemiologist, at [email protected]. CLINICAL UPDATES, OUTCOMES, & REAL-WORLD EVIDENCE New Pulmonary Arterial Hypertension (PAH) Guidelines Rollout | ACCP In March, the American College of Chest Physicians (ACCP) published an update of the CHEST Guideline and Expert Panel Report on Therapy for Pulmonary Arterial Hypertension (PAH) in Adults[1]. Highlights from the updates include: 1. ACCP now suggests prescribing an initial Letairis™ (ambrisentan; Gilead) and Adcirca™ (tadalafil, currently available as a generic) combination to improve 6-min walk distance (6MWD) in treatment- naive World Health Organization (WHO) functional class (FC) II and III PAH; and to add Adcirca™ to improve 6MWD among stable or symptomatic PAH patients on background Letairis™ 2. Incorporating palliative care services in the management of PAH patients 3. A revamped, evidence-based, and consensus-driven, treatment algorithm to guide the clinician through an organized approach to PAH management (below) PAH Combination Therapy Algorithm Combination therapy with ambrisentan and tadalfil (Recommendation 10; weak Yes recommendation, moderate quality evidence) Treatment Naïve PAH Is the patient willing or able to patients with WHO FC II tolerate combination -

Lääkealan Turvallisuus- Ja Kehittämiskeskuksen Päätös
Lääkealan turvallisuus- ja kehittämiskeskuksen päätös N:o xxxx lääkeluettelosta Annettu Helsingissä xx päivänä maaliskuuta 2016 ————— Lääkealan turvallisuus- ja kehittämiskeskus on 10 päivänä huhtikuuta 1987 annetun lääke- lain (395/1987) 83 §:n nojalla päättänyt vahvistaa seuraavan lääkeluettelon: 1 § Lääkeaineet ovat valmisteessa suolamuodossa Luettelon tarkoitus teknisen käsiteltävyyden vuoksi. Lääkeaine ja sen suolamuoto ovat biologisesti samanarvoisia. Tämä päätös sisältää luettelon Suomessa lääk- Liitteen 1 A aineet ovat lääkeaineanalogeja ja keellisessä käytössä olevista aineista ja rohdoksis- prohormoneja. Kaikki liitteen 1 A aineet rinnaste- ta. Lääkeluettelo laaditaan ottaen huomioon lää- taan aina vaikutuksen perusteella ainoastaan lää- kelain 3 ja 5 §:n säännökset. kemääräyksellä toimitettaviin lääkkeisiin. Lääkkeellä tarkoitetaan valmistetta tai ainetta, jonka tarkoituksena on sisäisesti tai ulkoisesti 2 § käytettynä parantaa, lievittää tai ehkäistä sairautta Lääkkeitä ovat tai sen oireita ihmisessä tai eläimessä. Lääkkeeksi 1) tämän päätöksen liitteessä 1 luetellut aineet, katsotaan myös sisäisesti tai ulkoisesti käytettävä niiden suolat ja esterit; aine tai aineiden yhdistelmä, jota voidaan käyttää 2) rikoslain 44 luvun 16 §:n 1 momentissa tar- ihmisen tai eläimen elintoimintojen palauttami- koitetuista dopingaineista annetussa valtioneuvos- seksi, korjaamiseksi tai muuttamiseksi farmako- ton asetuksessa kulloinkin luetellut dopingaineet; logisen, immunologisen tai metabolisen vaikutuk- ja sen avulla taikka terveydentilan -

094 Esketamine Nasal Spray
Esketamine Nasal Spray (SpravatoTM) and Intravenous Ketamine for Mental Health Conditions Prior Authorization Request Form Medical Policy #087 Esketamine Nasal Spray (SpravatoTM) and Intravenous Ketamine for Mental Health Conditions Please use this form to assist in identifying members who meet Blue Cross Blue Shield of Massachusetts’ (BCBSMA’s) medical necessity criteria for Esketamine Nasal Spray (SpravatoTM) and Intravenous Ketamine for Treatment-Resistant Depression. For members who do not meet all the criteria listed below, submit a letter of medical necessity with a request for Clinical Exception (Individual Consideration) and include copied of clinical documentation supporting the clinical exception request . Once completed, please fax to: 1-888-641-5199 Patient Information Patient Name: Today’s Date: BCBSMA ID#: Treatment Start Date: Date of Birth: Place of Service: Outpatient Inpatient Physician Information Facility Information Name: Name: Address: Address: Phone #: Phone #: Fax#: Fax#: This is a secure fax line This is a secure fax line NPI / TIN#: NPI / TIN#: For Esketamine and IV Ketamine requests for TREATMENT RESISTANT DEPRESSION: Initial requests are authorized for up to 28 days - Number of treatment session requested: __________________________ Esketamine (Spravato) Nasal Spray: Initial Therapy Intravenous Ketamine: Initial Therapy Individual is 18 or over, Individual meets the (DSM-5) criteria for a major depressive episode (See Table 1 in medical policy #087) by a structured clinical interview for DSM-5 disorders, Current depressive episode is severe depression based on either of the following: a. Montgomery-Asberg Depression Rating Scale (MADRS) ≥ 28 OR b. Hamilton Rating Scale for Depression (HAM-D) score ≥ 17 AND, Individual has had an inadequate response to four antidepressant agents from at least: • Four antidepressant agents from at least: o 2 or more different antidepressant classes (i.e. -

Esketamine (Spravato®) Nasal Spray Restricted Product(S)
Corporate Medical Policy: Esketamine (Spravato®) Nasal Spray Restricted Product(s): • esketamine (Spravato®) intranasal spray for administration under supervision of healthcare professional FDA Approved Use: • For the treatment of treatment-resistant depression in adults • For the treatment of depressive symptoms in adults with major depressive disorder with acute suicidal ideation or behavior • Limitations of use: o Effectiveness in preventing suicide or in reducing suicidal ideation or behavior has not been demonstrated; use of Spravato does not preclude need for hospitalization if clinically warranted, even if improvement is observed following initial dosing o Not approved as an anesthetic agent, as safety and effectiveness for this use have not been established Criteria for Medical Necessity: The restricted product(s) may be considered medically necessary when the following criteria are met: Initial Criteria for Approval: 1. The patient is 18 years of age or older; AND 2. The patient has been diagnosed with treatment-resistant depression (TRD); AND a. The patient has a confirmed diagnosis of major depressive disorder (MDD) to include one of the following: i. If single-episode MDD, the duration has been ≥ 2 years; OR ii. Recurrent MDD without psychotic features; AND b. In the current depressive episode, the patient has had an inadequate response (≤ 25% improvement) to at least two different oral antidepressants of adequate dose and duration (typically 6 weeks); OR 3. The patient has been diagnosed with major depressive disorder (MDD) with suicidal ideation or behavior; AND a. The suicidal ideation and intent are imminent and warrant potential hospitalization; AND 4. At initiation of treatment with esketamine nasal spray, the patient has a depression symptom severity of ≥ 28 on the Montgomery-Asberg Depression Rating Scale (MADRS), or as scored by a comparable standardized rating scale that reliably measures depressive symptoms; AND 5. -

Swissmedic Journal 01 2019
Schweizerisches Heilmittelinstitut Institut suisse des produits thérapeutiques Istituto svizzero per gli agenti terapeutici Swiss Agency for Therapeutic Products Swissmedic Journal 01/2019 18. Jahrgang 18° année ISSN 2234-9456 Amtliches Publikationsorgan der Swissmedic, Schweizerisches Heilmittelinstitut, Bern Publication officielle de Swissmedic, Institut suisse des produits thérapeutiques, Berne Erscheint monatlich/Publication mensuelle www.swissmedic.ch/journal Redaktion und Administration: Swissmedic, Abteilung Kommunikation, Hallerstrasse 7, 3012 Bern Tel. +41 58 462 02 11 Grafische Aufbereitung: Rickli+Wyss AG, Eymattstrasse 5, Postfach 316, 3027 Bern Inhalt / Table des matières Seite Seite Arzneimittel Nachrichten Arzneimittel Statistik Zulassung eines Arzneimittels mit Neuzulassung 6 neuem Wirkstoff: Radicava®, Revision und Änderung der Zulassung 11 Infusionslösung (Edaravonum) 4 Änderung der Zulassungsinhaberin 63 Widerruf der Zulassung 65 Erlöschen der Zulassung 67 Eingang eines vollständigen Gesuchs um Zulassung, um Erweiterung der Indikation oder um Erweiterung der Zulassung eines Arzneimittels 70 Swissmedic Kontaktliste Auf unserer Website www.swissmedic.ch finden Sie unter dem Navigationspunkt «Über uns» in der Rubrik «Kontakt» die Kontaktmaske für Anfragen und Reklamationen. Adressen für Meldungen sowie weitere Adressen finden Sie auf den entsprechenden Themenseiten. Zeichenerklärung Abgabekategorien A Einmalige Abgabe auf ärztliche oder C Abgabe nach Fachberatung durch tierärztliche Verschreibung Medizinalpersonen B Abgabe