Australian Public Assessment Report for Esketamine Hydrochloride
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Dextromethorphan Attenuates Sensorineural Hearing Loss in an Animal Model and Population-Based Cohort Study
International Journal of Environmental Research and Public Health Article Dextromethorphan Attenuates Sensorineural Hearing Loss in an Animal Model and Population-Based Cohort Study Hsin-Chien Chen 1,* , Chih-Hung Wang 1,2 , Wu-Chien Chien 3,4 , Chi-Hsiang Chung 3,4, Cheng-Ping Shih 1, Yi-Chun Lin 1,2, I-Hsun Li 5,6, Yuan-Yung Lin 1,2 and Chao-Yin Kuo 1 1 Department of Otolaryngology-Head and Neck Surgery, Tri-Service General Hospital, National Defense Medical Center, Taipei 114, Taiwan; [email protected] (C.-H.W.); [email protected] (C.-P.S.); [email protected] (Y.-C.L.); [email protected] (Y.-Y.L.); [email protected] (C.-Y.K.) 2 Graduate Institute of Medical Sciences, National Defense Medical Center, Taipei 114, Taiwan 3 School of Public Health, National Defense Medical Center, Taipei 114, Taiwan; [email protected] (W.-C.C.); [email protected] (C.-H.C.) 4 Department of Medical Research, Tri-Service General Hospital, National Defense Medical Center, Taipei 114, Taiwan 5 Department of Pharmacy Practice, Tri-Service General Hospital, National Defense Medical Center, Taipei 114, Taiwan; [email protected] 6 School of Pharmacy, National Defense Medical Center, Taipei 114, Taiwan * Correspondence: [email protected]; Tel.: +886-2-8792-7192; Fax: +886-2-8792-7193 Received: 31 July 2020; Accepted: 28 August 2020; Published: 31 August 2020 Abstract: The effect of dextromethorphan (DXM) use in sensorineural hearing loss (SNHL) has not been fully examined. We conducted an animal model and nationwide retrospective matched-cohort study to explore the association between DXM use and SNHL. -
A Case Study on Addressing Abuse of a Safe and Effective Drug David C
Spangler et al. Substance Abuse Treatment, Prevention, and Policy (2016) 11:22 DOI 10.1186/s13011-016-0067-0 DEBATE Open Access Dextromethorphan: a case study on addressing abuse of a safe and effective drug David C. Spangler1, Catherine M. Loyd1* and Emily E. Skor1,2 Abstract Background: Dextromethorphan is a safe, effective cough suppressant, available without a prescription in the United States since 1958. Due to a perceived prevalence of abuse of dextromethorphan by teens, in 2007 the Drug Enforcement Administration requested the Food and Drug Administration evaluate whether dextromethorphan should be recommended for scheduling under the Controlled Substances Act. The Food and Drug Administration held an Advisory Committee meeting in 2010 to provide a scientific and medical evaluation of dextromethorphan and its abuse potential. Discussion: To address reports of abuse, particularly by teens in the United States, the Consumer Healthcare Products Association initiated an abuse mitigation plan in 2010 with specific goals related to awareness of the behavior, perception of risk, social disapproval, and access to the products. In identifying abuse interventions, experts acknowledge that substance abuse among teens is a highly complex behavior and indicate that the best course of action is to address prevention by focusing on the factors that impact teen behavior. Conclusion: It is noteworthy that the annual prevalence of over-the-counter cough medicine abuse has sharply decreased since 2010. While a true cause-and-effect relationship cannot be assured, the Consumer Healthcare Products Association and its member companies believe that the increased awareness of the issue since the 2010 Food and Drug Administration Advisory Committee meeting, and the subsequent implementation of a well-delivered and targeted abuse mitigation plan that addressed the levers influencing teen decisions is contributing to the observed reduction in abuse. -

Lithium Stimulates Glutamate "Release" and Inositol 1,4,5
Proc. Nat!. Acad. Sci. USA Vol. 91, pp. 8358-8362, August 1994 Neurobiology Lithium stimulates glutamate "release" and inositol 1,4,5-trisphosphate accumulation via activation of the N-methyl-D-aspartate receptor in monkey and mouse cerebral cortex slices (manic depression/bipolar disorder/primates) JOHN F. DIXON, GEORGYI V. Los, AND LOWELL E. HOKIN* Department of Pharmacology, University of Wisconsin Medical School, 1300 University Avenue, Madison, WI 53706 Communicated by Henry Lardy, May 9, 1994 (received for review February 18, 1994) ABSTRACT Beginning at therapeutic concentrations (1- showed lithium-stimulated increases in Ins(1,4,5)P3 and 1.5 mM), the anti-manic-depressive drug lithium stimulated inositol 1,3,4,5-tetrakisphosphate (2). the release of glutamate, a major excitatory neurotransmitter In the case of rhesus monkey, neither inositol nor an in the brain, in monkey cerebral cortex slices in a time- and agonist was required to demonstrate lithium-stimulated ac- concentration-dependent manner, and this was associated with cumulation of Ins(1,4,5)P3 (3). This suggested that an endog- increased inositol 1,4,5-trisphosphate [Ins(1,4,5)P3] accumu- enous neurotransmitter was involved in the lithium effect. lation. (±)-3-(2-Carboxypiperazin-4-yl)propyl-1-phosphoric We show here that, beginning at therapeutic concentrations, acid (CPP), dizocilpine (MK-801), ketamine, and Mg2+- lithium stimulated the release ofglutamate in rhesus monkey antagonists to the N-methyl-D-aspartate (NMDA) recep- and mouse cerebral cortex slices, and this in turn increased tor/channel complex selectively inhibited lithium-stimulated accumulation of Ins(1,4,5)P3 via activation of the N-methyl- Ins(t,4,5)P3 accumulation. -

Hallucinogens
Hallucinogens What are hallucinogens? Hallucinogens are a diverse group of drugs that alter a person’s awareness of their surroundings as well as their own thoughts and feelings. They are commonly split into two categories: classic hallucinogens (such as LSD) and dissociative drugs (such as PCP). Both types of hallucinogens can cause hallucinations, or sensations and images that seem real though they are not. Additionally, dissociative drugs can cause users to feel out of control or disconnected from their body and environment. Some hallucinogens are extracted from plants or mushrooms, and some are synthetic (human- made). Historically, people have used hallucinogens for religious or healing rituals. More recently, people report using these drugs for social or recreational purposes, including to have fun, deal with stress, have spiritual experiences, or just to feel different. Common classic hallucinogens include the following: • LSD (D-lysergic acid diethylamide) is one of the most powerful mind-altering chemicals. It is a clear or white odorless material made from lysergic acid, which is found in a fungus that grows on rye and other grains. LSD has many other street names, including acid, blotter acid, dots, and mellow yellow. • Psilocybin (4-phosphoryloxy-N,N- dimethyltryptamine) comes from certain types of mushrooms found in tropical and subtropical regions of South America, Mexico, and the United States. Some common names for Blotter sheet of LSD-soaked paper squares that users psilocybin include little smoke, magic put in their mouths. mushrooms, and shrooms. Photo by © DEA • Peyote (mescaline) is a small, spineless cactus with mescaline as its main ingredient. Peyote can also be synthetic. -
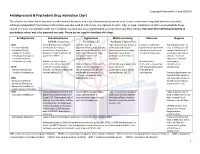
Antidepressant & Psychedelic Drug Interaction Chart
Copyright Psychedelic School 8/2020 Antidepressant & Psychedelic Drug Interaction Chart This chart is not intended to be used to make medical decisions and is for informational purposes only. It was constructed using data whenever possible, although extrapolation from known information was also used to inform risk. Any decision to start, stop, or taper medication and/or use psychedelic drugs should be made in conjunction with your healthcare provider(s). It is recommended to not perform any illicit activity. This chart the intellectual property of psychedelic school and is for personal use only. Please do not copy or distribute this chart. Antidepressant Phenethylamines Tryptamines MAOI-containing Ketamine Ibogaine -MDMA, mescaline -Psilocybin, LSD -Ayahuasca, Syrian Rue SSRIs Taper & discontinue at least 2 Consider taper & Taper & discontinue at least 2 Has been studied and Taper & discontinue at · Paroxetine (Paxil) weeks prior (all except discontinuation at least 2 weeks weeks prior (all except found effective both with least 2 weeks prior (all · Sertraline (Zoloft) fluoxetine) or 6 weeks prior prior (all except fluoxetine) or 6 fluoxetine) or 6 weeks prior and without concurrent except fluoxetine) or 6 · Citalopram (Celexa) (fluoxetine only) due to loss of weeks prior (fluoxetine only) (fluoxetine only) due to use of antidepressants weeks prior (fluoxetine · Escitalopram (Lexapro) psychedelic effect due to potential loss of potential risk of serotonin only) due to risk of · Fluxoetine (Prozac) psychedelic effect syndrome additive QTc interval · Fluvoxamine (Luvox) MDMA is unable to cause Recommended prolongation, release of serotonin when the Chronic antidepressant use may Life threatening toxicities can to be used in conjunction arrhythmias, or SPARI serotonin reuptake pump is result in down-regulation of occur with these with oral antidepressants cardiotoxicity · Vibryyd (Vilazodone) blocked. -

Janssen Research & Development, LLC Advisory Committee Briefing
Janssen Research & Development, LLC Advisory Committee Briefing Document Esketamine Nasal Spray for Patients with Treatment-resistant Depression JNJ-54135419 (esketamine) Status: Approved Date: 16 January 2019 Prepared by: Janssen Research & Development, LLC EDMS number: EDMS-ERI-171521650, 1.0 ADVISORY COMMITTEE BRIEFING MATERIALS: AVAILABLE FOR PUBLIC RELEASE 1 Status: Approved, Date: 16 January 2019 JNJ-54135419 (esketamine) Treatment-resistant Depression Advisory Committee Briefing Document GUIDE FOR REVIEWERS This briefing document provides 3 levels of review with increasing levels of detail: The Executive Overview (Section 1, starting on page 11) provides a narrative summarizing the disease, need for novel treatments, key development program characteristics for esketamine nasal spray, study results, and conclusions. References are made to the respective supporting sections in the core document. The core document (Section 2 to Section 11, starting on page 30) includes detailed summaries and discussion in support of the Executive Overview. The appendices (starting on page 180) provide additional or more detailed information to complement brief descriptions provided in sections of the core document (e.g., demographic and baseline characteristics of the study populations, additional efficacy analyses in the Phase 3 studies, statistical methods). These appendices are referenced in the core document when relevant. This review structure allows review at varying levels of detail; however, reviewers who read at multiple levels will necessarily -

Psychedelics in Psychiatry: Neuroplastic, Immunomodulatory, and Neurotransmitter Mechanismss
Supplemental Material can be found at: /content/suppl/2020/12/18/73.1.202.DC1.html 1521-0081/73/1/202–277$35.00 https://doi.org/10.1124/pharmrev.120.000056 PHARMACOLOGICAL REVIEWS Pharmacol Rev 73:202–277, January 2021 Copyright © 2020 by The Author(s) This is an open access article distributed under the CC BY-NC Attribution 4.0 International license. ASSOCIATE EDITOR: MICHAEL NADER Psychedelics in Psychiatry: Neuroplastic, Immunomodulatory, and Neurotransmitter Mechanismss Antonio Inserra, Danilo De Gregorio, and Gabriella Gobbi Neurobiological Psychiatry Unit, Department of Psychiatry, McGill University, Montreal, Quebec, Canada Abstract ...................................................................................205 Significance Statement. ..................................................................205 I. Introduction . ..............................................................................205 A. Review Outline ........................................................................205 B. Psychiatric Disorders and the Need for Novel Pharmacotherapies .......................206 C. Psychedelic Compounds as Novel Therapeutics in Psychiatry: Overview and Comparison with Current Available Treatments . .....................................206 D. Classical or Serotonergic Psychedelics versus Nonclassical Psychedelics: Definition ......208 Downloaded from E. Dissociative Anesthetics................................................................209 F. Empathogens-Entactogens . ............................................................209 -

Development of Allosteric Modulators of Gpcrs for Treatment of CNS Disorders Hilary Highfield Nickols A, P
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Elsevier - Publisher Connector Neurobiology of Disease 61 (2014) 55–71 Contents lists available at ScienceDirect Neurobiology of Disease journal homepage: www.elsevier.com/locate/ynbdi Review Development of allosteric modulators of GPCRs for treatment of CNS disorders Hilary Highfield Nickols a, P. Jeffrey Conn b,⁎ a Division of Neuropathology, Department of Pathology, Microbiology and Immunology, Vanderbilt University, USA b Department of Pharmacology, Vanderbilt University, Nashville, TN 37232, USA article info abstract Article history: The discovery of allosteric modulators of G protein-coupled receptors (GPCRs) provides a promising new strategy Received 25 July 2013 with potential for developing novel treatments for a variety of central nervous system (CNS) disorders. Tradition- Revised 13 September 2013 al drug discovery efforts targeting GPCRs have focused on developing ligands for orthosteric sites which bind en- Accepted 17 September 2013 dogenous ligands. Allosteric modulators target a site separate from the orthosteric site to modulate receptor Available online 27 September 2013 function. These allosteric agents can either potentiate (positive allosteric modulator, PAM) or inhibit (negative allosteric modulator, NAM) the receptor response and often provide much greater subtype selectivity than Keywords: Allosteric modulator orthosteric ligands for the same receptors. Experimental evidence has revealed more nuanced pharmacological CNS modes of action of allosteric modulators, with some PAMs showing allosteric agonism in combination with pos- Drug discovery itive allosteric modulation in response to endogenous ligand (ago-potentiators) as well as “bitopic” ligands that GPCR interact with both the allosteric and orthosteric sites. Drugs targeting the allosteric site allow for increased drug Metabotropic glutamate receptor selectivity and potentially decreased adverse side effects. -

The Effects of Ketamine on Dopaminergic Function: Meta-Analysis and Review of the Implications for Neuropsychiatric Disorders
OPEN Molecular Psychiatry (2018) 23, 59–69 www.nature.com/mp REVIEW The effects of ketamine on dopaminergic function: meta-analysis and review of the implications for neuropsychiatric disorders M Kokkinou1,2, AH Ashok1,2,3 and OD Howes1,2,3 Ketamine is a non-competitive antagonist at the N-methyl-D-aspartate receptor. It has recently been found to have antidepressant effects and is a drug of abuse, suggesting it may have dopaminergic effects. To examine the effect of ketamine on the dopamine systems, we carried out a systematic review and meta-analysis of dopamine measures in the rodent, human and primate brain following acute and chronic ketamine administration relative to a drug-free baseline or control condition. Systematic search of PubMed and PsychInfo electronic databases yielded 40 original peer-reviewed studies. There were sufficient rodent studies of the acute effects of ketamine at sub-anaesthetic doses for meta-analysis. Acute ketamine administration in rodents is associated with significantly increased dopamine levels in the cortex (Hedge’s g = 1.33, Po0.01), striatum (Hedge’s g = 0.57, Po0.05) and the nucleus accumbens (Hedge’s g = 1.30, Po0.05) compared to control conditions, and 62–180% increases in dopamine neuron population activity. Sub-analysis indicated elevations were more marked in in vivo (g = 1.93) than ex vivo (g = 0.50) studies. There were not enough studies for meta-analysis in other brain regions studied (hippocampus, ventral pallidum and cerebellum), or of the effects of chronic ketamine administration, although consistent increases in cortical dopamine levels (from 88 to 180%) were reported in the latter studies. -

Advisory Council on the Misuse of Drugs Chair: Professor Les Iversen Secretary: Rachel Fowler 3Rd Floor Seacole Building 2
ACMD Advisory Council on the Misuse of Drugs Chair: Professor Les Iversen Secretary: Rachel Fowler 3rd Floor Seacole Building 2. Marsham Street London SW1P 4DF 020 7035 0454 Email: [email protected] Rt Hon. Theresa May MP Home Office 2 Marsham Street London SW1P 4DF 18th October 2012 Dear Home Secretary, In March 2012 the ACMD advised that methoxetamine be subject to a temporary class drug order. Methoxetamine was marketed as a legal alternative to ketamine until a temporary class drug order was implemented in April 2012. As is now required, the ACMD has followed its initial assessment with a consideration of methoxetamine in the context of the Misuse of Drugs Act 1971; I enclose the report with this letter. The chemical structure of methoxetamine bears a close resemblance to that of both ketamine and phencyclidine (PCP, „Angel Dust‟, a class A drug), which both produce well- documented and serious adverse effects following both acute and chronic usage. Users report that the effects of methoxetamine are similar to those of ketamine, however, some users report that the effects are of longer duration.The harmful effects reported include severe dissociation, cardiovascular symptoms, paranoid thoughts and unpleasant hallucinations. The first analytically confirmed series reported by Guy‟s and St Thomas‟ NHS Foundation Trust, London in 2011, was of three individuals who presented having self-reported use of methoxetamine. All three presented with a ketamine-like dissociative state, but also had significant stimulant effects with agitation and cardiovascular effects including tachycardia and hypertension. Toxicological screening of serum samples confirmed methoxetamine use in two of the cases. -

Rxoutlook® 1St Quarter 2019
® RxOutlook 1st Quarter 2020 optum.com/optumrx a RxOutlook 1st Quarter 2020 Orphan drugs continue to feature prominently in the drug development pipeline In 1983 the Orphan Drug Act was signed into law. Thirty seven years later, what was initially envisioned as a minor category of drugs has become a major part of the drug development pipeline. The Orphan Drug Act was passed by the United States Congress in 1983 in order to spur drug development for rare conditions with high unmet need. The legislation provided financial incentives to manufacturers if they could demonstrate that the target population for their drug consisted of fewer than 200,000 persons in the United States, or that there was no reasonable expectation that commercial sales would be sufficient to recoup the developmental costs associated with the drug. These “Orphan Drug” approvals have become increasingly common over the last two decades. In 2000, two of the 27 (7%) new drugs approved by the FDA had Orphan Designation, whereas in 2019, 20 of the 48 new drugs (42%) approved by the FDA had Orphan Designation. Since the passage of the Orphan Drug Act, 37 years ago, additional regulations and FDA designations have been implemented in an attempt to further expedite drug development for certain serious and life threatening conditions. Drugs with a Fast Track designation can use Phase 2 clinical trials to support FDA approval. Drugs with Breakthrough Therapy designation can use alternative clinical trial designs instead of the traditional randomized, double-blind, placebo-controlled trial. Additionally, drugs may be approved via the Accelerated Approval pathway using surrogate endpoints in clinical trials rather than clinical outcomes. -
Effects of Ketamine and Ketamine Metabolites on Evoked Striatal Dopamine Release, Dopamine Receptors, and Monoamine Transporters
1521-0103/359/1/159–170$25.00 http://dx.doi.org/10.1124/jpet.116.235838 THE JOURNAL OF PHARMACOLOGY AND EXPERIMENTAL THERAPEUTICS J Pharmacol Exp Ther 359:159–170, October 2016 U.S. Government work not protected by U.S. copyright Effects of Ketamine and Ketamine Metabolites on Evoked Striatal Dopamine Release, Dopamine Receptors, and Monoamine Transporters Adem Can,1 Panos Zanos,1 Ruin Moaddel, Hye Jin Kang, Katinia S. S. Dossou, Irving W. Wainer, Joseph F. Cheer, Douglas O. Frost, Xi-Ping Huang, and Todd D. Gould Department of Psychiatry (A.C., P.Z., J.F.C., D.O.F., T.D.G.), Department of Pharmacology (D.O.F, T.D.G), and Department of Anatomy and Neurobiology (J.F.C, T.D.G), University of Maryland School of Medicine, Baltimore, Maryland; Department of Psychology, Notre Dame of Maryland University, Baltimore, Maryland (A.C.); Biomedical Research Center, National Institute on Aging, National Institutes of Health, Baltimore, Maryland (R.M., K.S.S.D., I.W.W.); National Institute of Mental Health Psychoactive Drug Screening Program, Department of Pharmacology, University of North Carolina Chapel Hill Medical School, Chapel Hill, North Carolina (H.J.K., X.-P.H.); and Mitchell Woods Pharmaceuticals, Shelton, Connecticut (I.W.W.) Received June 14, 2016; accepted July 27, 2016 ABSTRACT Following administration at subanesthetic doses, (R,S)-ketamine mesolimbic DA release and decay using fast-scan cyclic (ketamine) induces rapid and robust relief from symptoms of voltammetry following acute administration of subanesthetic depression in treatment-refractory depressed patients. Previous doses of ketamine (2, 10, and 50 mg/kg, i.p.).