The Effects of Ketamine on Dopaminergic Function: Meta-Analysis and Review of the Implications for Neuropsychiatric Disorders
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Dextromethorphan Attenuates Sensorineural Hearing Loss in an Animal Model and Population-Based Cohort Study
International Journal of Environmental Research and Public Health Article Dextromethorphan Attenuates Sensorineural Hearing Loss in an Animal Model and Population-Based Cohort Study Hsin-Chien Chen 1,* , Chih-Hung Wang 1,2 , Wu-Chien Chien 3,4 , Chi-Hsiang Chung 3,4, Cheng-Ping Shih 1, Yi-Chun Lin 1,2, I-Hsun Li 5,6, Yuan-Yung Lin 1,2 and Chao-Yin Kuo 1 1 Department of Otolaryngology-Head and Neck Surgery, Tri-Service General Hospital, National Defense Medical Center, Taipei 114, Taiwan; [email protected] (C.-H.W.); [email protected] (C.-P.S.); [email protected] (Y.-C.L.); [email protected] (Y.-Y.L.); [email protected] (C.-Y.K.) 2 Graduate Institute of Medical Sciences, National Defense Medical Center, Taipei 114, Taiwan 3 School of Public Health, National Defense Medical Center, Taipei 114, Taiwan; [email protected] (W.-C.C.); [email protected] (C.-H.C.) 4 Department of Medical Research, Tri-Service General Hospital, National Defense Medical Center, Taipei 114, Taiwan 5 Department of Pharmacy Practice, Tri-Service General Hospital, National Defense Medical Center, Taipei 114, Taiwan; [email protected] 6 School of Pharmacy, National Defense Medical Center, Taipei 114, Taiwan * Correspondence: [email protected]; Tel.: +886-2-8792-7192; Fax: +886-2-8792-7193 Received: 31 July 2020; Accepted: 28 August 2020; Published: 31 August 2020 Abstract: The effect of dextromethorphan (DXM) use in sensorineural hearing loss (SNHL) has not been fully examined. We conducted an animal model and nationwide retrospective matched-cohort study to explore the association between DXM use and SNHL. -

Medical Review Officer Manual
Department of Health and Human Services Substance Abuse and Mental Health Services Administration Center for Substance Abuse Prevention Medical Review Officer Manual for Federal Agency Workplace Drug Testing Programs EFFECTIVE OCTOBER 1, 2010 Note: This manual applies to Federal agency drug testing programs that come under Executive Order 12564 dated September 15, 1986, section 503 of Public Law 100-71, 5 U.S.C. section 7301 note dated July 11, 1987, and the Department of Health and Human Services Mandatory Guidelines for Federal Workplace Drug Testing Programs (73 FR 71858) dated November 25, 2008 (effective October 1, 2010). This manual does not apply to specimens submitted for testing under U.S. Department of Transportation (DOT) Procedures for Transportation Workplace Drug and Alcohol Testing Programs (49 CFR Part 40). The current version of this manual and other information including MRO Case Studies are available on the Drug Testing page under Medical Review Officer (MRO) Resources on the SAMHSA website: http://www.workplace.samhsa.gov Previous Versions of this Manual are Obsolete 3 Table of Contents Chapter 1. The Medical Review Officer (MRO)........................................................................... 6 Chapter 2. The Federal Drug Testing Custody and Control Form ................................................ 7 Chapter 3. Urine Drug Testing ...................................................................................................... 9 A. Federal Workplace Drug Testing Overview.................................................................. -
A Case Study on Addressing Abuse of a Safe and Effective Drug David C
Spangler et al. Substance Abuse Treatment, Prevention, and Policy (2016) 11:22 DOI 10.1186/s13011-016-0067-0 DEBATE Open Access Dextromethorphan: a case study on addressing abuse of a safe and effective drug David C. Spangler1, Catherine M. Loyd1* and Emily E. Skor1,2 Abstract Background: Dextromethorphan is a safe, effective cough suppressant, available without a prescription in the United States since 1958. Due to a perceived prevalence of abuse of dextromethorphan by teens, in 2007 the Drug Enforcement Administration requested the Food and Drug Administration evaluate whether dextromethorphan should be recommended for scheduling under the Controlled Substances Act. The Food and Drug Administration held an Advisory Committee meeting in 2010 to provide a scientific and medical evaluation of dextromethorphan and its abuse potential. Discussion: To address reports of abuse, particularly by teens in the United States, the Consumer Healthcare Products Association initiated an abuse mitigation plan in 2010 with specific goals related to awareness of the behavior, perception of risk, social disapproval, and access to the products. In identifying abuse interventions, experts acknowledge that substance abuse among teens is a highly complex behavior and indicate that the best course of action is to address prevention by focusing on the factors that impact teen behavior. Conclusion: It is noteworthy that the annual prevalence of over-the-counter cough medicine abuse has sharply decreased since 2010. While a true cause-and-effect relationship cannot be assured, the Consumer Healthcare Products Association and its member companies believe that the increased awareness of the issue since the 2010 Food and Drug Administration Advisory Committee meeting, and the subsequent implementation of a well-delivered and targeted abuse mitigation plan that addressed the levers influencing teen decisions is contributing to the observed reduction in abuse. -

Forensic Features of a Fatal Datura Poisoning Case During a Robbery
Forensic Science International 261 (2016) e17–e21 Contents lists available at ScienceDirect Forensic Science International jou rnal homepage: www.elsevier.com/locate/forsciint Case report Forensic features of a fatal Datura poisoning case during a robbery a, a a a a,b E. Le Garff *, Y. Delannoy , V. Mesli , V. He´douin , G. Tournel a Univ Lille, CHU Lille, UTML (EA7367), Service de Me´decine Le´gale, F-59000 Lille, France b Univ Lille, CHU Lille, Laboratoire de Toxicologie, F-59000 Lille, France A R T I C L E I N F O A B S T R A C T Article history: Datura poisonings have been previously described but remain rare in forensic practice. Here, we present Received 2 October 2015 a homicide case involving Datura poisoning, which occurred during a robbery. Toxicological results Received in revised form 28 January 2016 were obtained by second autopsy performed after one previous autopsy and full body embalmment. A Accepted 13 February 2016 35-year-old man presented with severe stomach and digestive pain, became unconscious and ultimately Available online 23 February 2016 died during a trip in Asia. A first autopsy conducted in Asia revealed no trauma, intoxication or pathology. The corpse was embalmed with methanol/formalin. A second autopsy was performed in France, and Keywords: toxicology samples were collected. Scopolamine, atropine, and hyoscyamine were found in the vitreous Forensic humor, in addition to methanol. Police investigators questioned the local travel guide, who admitted to Intoxication Datura having added Datura to a drink to stun and rob his victim. The victim’s death was attributed to disordered Homicide heart rhythm due to severe anticholinergic syndrome following fatal Datura intoxication. -

The Cannabinoid Receptor Agonist WIN 55,212-2 Attenuates the Effects Induced by Quinolinic Acid in the Rat Striatum
Neuropharmacology 51 (2006) 1004e1012 www.elsevier.com/locate/neuropharm The cannabinoid receptor agonist WIN 55,212-2 attenuates the effects induced by quinolinic acid in the rat striatum A. Pintor a, M.T. Tebano a, A. Martire a, R. Grieco a, M. Galluzzo a, M.L. Scattoni b,A.Pe`zzola a, R. Coccurello c, F. Felici a, V. Cuomo d, D. Piomelli e, G. Calamandrei b, P. Popoli a,* a Department of Drug Research and Evaluation, Central Nervous System Pharmacology Division, Istituto Superiore di Sanita`, Viale Regina Elena, 299, 00161 Rome, Italy b Department of Cell Biology and Neuroscience, Istituto Superiore di Sanita`, Viale Regina Elena, 299, 00161 Rome, Italy c Institute of Neuroscience, EBRI Foundation, Rome, Italy d Department of Pharmacology and General Physiology, University ‘‘La Sapienza’’, Rome, Italy e Department of Pharmacology and Center for Drug Discovery, University of California, Irvine, CA, USA Received 7 April 2006; received in revised form 15 May 2006; accepted 16 June 2006 Abstract The ability of CB1 receptors to regulate the release of glutamate in the striatum, together with the finding that, in experimental models of Huntington disease (HD), both endocannabinoid levels and CB1 receptor densities are reduced, has prompted the investigation on the neuropro- tective role of the cannabinoids in HD. Quinolinic acid (QA) is an excitotoxin that, when injected in the rat striatum reproduces many features of HD and that acts by stimulating glutamate outflow. The aim of the present study was to test the ability of the cannabinoid receptor agonist WIN 55,212-2 to prevent the effects induced by QA in the rat striatum. -

Carbon-I I-D-Threo-Methylphenidate Binding to Dopamine Transporter in Baboon Brain
Carbon-i i-d-threo-Methylphenidate Binding to Dopamine Transporter in Baboon Brain Yu-Shin Ding, Joanna S. Fowler, Nora D. Volkow, Jean Logan, S. John Gatley and Yuichi Sugano Brookhaven National Laboratory, Upton, New York; and Department of Psychiatry, SUNY Stony Brook@Stony Brook@NY children (1). MP is also used to treat narcolepsy (2). The The more active d-enantiomer of methyiphenidate (dI-threo psychostimulant properties of MP have been linked to its methyl-2-phenyl-2-(2-piperidyl)acetate, Ritalin)was labeled with binding to a site on the dopamine transporter, resulting in lic (t1,@:20.4 mm) to characterize its binding, examine its spec inhibition of dopamine reuptake and enhanced levels of ificftyfor the dopamine transporter and evaluate it as a radio synaptic dopamine. tracer forthe presynapticdopaminergicneuron. Methods PET We have developed a rapid synthesis of [11C]dl-threo studies were canied out inthe baboon. The pharmacokinetics of methylphenidate ([“C]MP)to examine its pharmacokinet r1c]d-th@O-msth@ha@idate @f'1C]d-thmo-MP)weremeasured ics and pharmacological profile in vivo and to evaluate its and compared with r1cY-th@o-MP and with fts racemate ff@1C]fl-thmo-meth@1phenidate,r1c]MP). Nonradioact,ve meth suitability as a radiotracer for the presynaptic dopaminergic ylphenidate was used to assess the reveralbilityand saturability neuron (3,4). These first PET studies of MP in the baboon of the binding. GBR 12909, 3@3-(4-iodophenyI)tropane-2-car and human brain demonstrated the saturable [1‘C]MP boxylic acid methyl ester (fi-Cfl), tomoxetine and citalopram binding to the dopamine transporter in the baboon brain were used to assess the binding specificity. -

The Phytochemistry of Cherokee Aromatic Medicinal Plants
medicines Review The Phytochemistry of Cherokee Aromatic Medicinal Plants William N. Setzer 1,2 1 Department of Chemistry, University of Alabama in Huntsville, Huntsville, AL 35899, USA; [email protected]; Tel.: +1-256-824-6519 2 Aromatic Plant Research Center, 230 N 1200 E, Suite 102, Lehi, UT 84043, USA Received: 25 October 2018; Accepted: 8 November 2018; Published: 12 November 2018 Abstract: Background: Native Americans have had a rich ethnobotanical heritage for treating diseases, ailments, and injuries. Cherokee traditional medicine has provided numerous aromatic and medicinal plants that not only were used by the Cherokee people, but were also adopted for use by European settlers in North America. Methods: The aim of this review was to examine the Cherokee ethnobotanical literature and the published phytochemical investigations on Cherokee medicinal plants and to correlate phytochemical constituents with traditional uses and biological activities. Results: Several Cherokee medicinal plants are still in use today as herbal medicines, including, for example, yarrow (Achillea millefolium), black cohosh (Cimicifuga racemosa), American ginseng (Panax quinquefolius), and blue skullcap (Scutellaria lateriflora). This review presents a summary of the traditional uses, phytochemical constituents, and biological activities of Cherokee aromatic and medicinal plants. Conclusions: The list is not complete, however, as there is still much work needed in phytochemical investigation and pharmacological evaluation of many traditional herbal medicines. Keywords: Cherokee; Native American; traditional herbal medicine; chemical constituents; pharmacology 1. Introduction Natural products have been an important source of medicinal agents throughout history and modern medicine continues to rely on traditional knowledge for treatment of human maladies [1]. Traditional medicines such as Traditional Chinese Medicine [2], Ayurvedic [3], and medicinal plants from Latin America [4] have proven to be rich resources of biologically active compounds and potential new drugs. -

Lithium Stimulates Glutamate "Release" and Inositol 1,4,5
Proc. Nat!. Acad. Sci. USA Vol. 91, pp. 8358-8362, August 1994 Neurobiology Lithium stimulates glutamate "release" and inositol 1,4,5-trisphosphate accumulation via activation of the N-methyl-D-aspartate receptor in monkey and mouse cerebral cortex slices (manic depression/bipolar disorder/primates) JOHN F. DIXON, GEORGYI V. Los, AND LOWELL E. HOKIN* Department of Pharmacology, University of Wisconsin Medical School, 1300 University Avenue, Madison, WI 53706 Communicated by Henry Lardy, May 9, 1994 (received for review February 18, 1994) ABSTRACT Beginning at therapeutic concentrations (1- showed lithium-stimulated increases in Ins(1,4,5)P3 and 1.5 mM), the anti-manic-depressive drug lithium stimulated inositol 1,3,4,5-tetrakisphosphate (2). the release of glutamate, a major excitatory neurotransmitter In the case of rhesus monkey, neither inositol nor an in the brain, in monkey cerebral cortex slices in a time- and agonist was required to demonstrate lithium-stimulated ac- concentration-dependent manner, and this was associated with cumulation of Ins(1,4,5)P3 (3). This suggested that an endog- increased inositol 1,4,5-trisphosphate [Ins(1,4,5)P3] accumu- enous neurotransmitter was involved in the lithium effect. lation. (±)-3-(2-Carboxypiperazin-4-yl)propyl-1-phosphoric We show here that, beginning at therapeutic concentrations, acid (CPP), dizocilpine (MK-801), ketamine, and Mg2+- lithium stimulated the release ofglutamate in rhesus monkey antagonists to the N-methyl-D-aspartate (NMDA) recep- and mouse cerebral cortex slices, and this in turn increased tor/channel complex selectively inhibited lithium-stimulated accumulation of Ins(1,4,5)P3 via activation of the N-methyl- Ins(t,4,5)P3 accumulation. -

Hallucinogens
Hallucinogens What are hallucinogens? Hallucinogens are a diverse group of drugs that alter a person’s awareness of their surroundings as well as their own thoughts and feelings. They are commonly split into two categories: classic hallucinogens (such as LSD) and dissociative drugs (such as PCP). Both types of hallucinogens can cause hallucinations, or sensations and images that seem real though they are not. Additionally, dissociative drugs can cause users to feel out of control or disconnected from their body and environment. Some hallucinogens are extracted from plants or mushrooms, and some are synthetic (human- made). Historically, people have used hallucinogens for religious or healing rituals. More recently, people report using these drugs for social or recreational purposes, including to have fun, deal with stress, have spiritual experiences, or just to feel different. Common classic hallucinogens include the following: • LSD (D-lysergic acid diethylamide) is one of the most powerful mind-altering chemicals. It is a clear or white odorless material made from lysergic acid, which is found in a fungus that grows on rye and other grains. LSD has many other street names, including acid, blotter acid, dots, and mellow yellow. • Psilocybin (4-phosphoryloxy-N,N- dimethyltryptamine) comes from certain types of mushrooms found in tropical and subtropical regions of South America, Mexico, and the United States. Some common names for Blotter sheet of LSD-soaked paper squares that users psilocybin include little smoke, magic put in their mouths. mushrooms, and shrooms. Photo by © DEA • Peyote (mescaline) is a small, spineless cactus with mescaline as its main ingredient. Peyote can also be synthetic. -
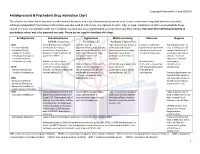
Antidepressant & Psychedelic Drug Interaction Chart
Copyright Psychedelic School 8/2020 Antidepressant & Psychedelic Drug Interaction Chart This chart is not intended to be used to make medical decisions and is for informational purposes only. It was constructed using data whenever possible, although extrapolation from known information was also used to inform risk. Any decision to start, stop, or taper medication and/or use psychedelic drugs should be made in conjunction with your healthcare provider(s). It is recommended to not perform any illicit activity. This chart the intellectual property of psychedelic school and is for personal use only. Please do not copy or distribute this chart. Antidepressant Phenethylamines Tryptamines MAOI-containing Ketamine Ibogaine -MDMA, mescaline -Psilocybin, LSD -Ayahuasca, Syrian Rue SSRIs Taper & discontinue at least 2 Consider taper & Taper & discontinue at least 2 Has been studied and Taper & discontinue at · Paroxetine (Paxil) weeks prior (all except discontinuation at least 2 weeks weeks prior (all except found effective both with least 2 weeks prior (all · Sertraline (Zoloft) fluoxetine) or 6 weeks prior prior (all except fluoxetine) or 6 fluoxetine) or 6 weeks prior and without concurrent except fluoxetine) or 6 · Citalopram (Celexa) (fluoxetine only) due to loss of weeks prior (fluoxetine only) (fluoxetine only) due to use of antidepressants weeks prior (fluoxetine · Escitalopram (Lexapro) psychedelic effect due to potential loss of potential risk of serotonin only) due to risk of · Fluxoetine (Prozac) psychedelic effect syndrome additive QTc interval · Fluvoxamine (Luvox) MDMA is unable to cause Recommended prolongation, release of serotonin when the Chronic antidepressant use may Life threatening toxicities can to be used in conjunction arrhythmias, or SPARI serotonin reuptake pump is result in down-regulation of occur with these with oral antidepressants cardiotoxicity · Vibryyd (Vilazodone) blocked. -

Janssen Research & Development, LLC Advisory Committee Briefing
Janssen Research & Development, LLC Advisory Committee Briefing Document Esketamine Nasal Spray for Patients with Treatment-resistant Depression JNJ-54135419 (esketamine) Status: Approved Date: 16 January 2019 Prepared by: Janssen Research & Development, LLC EDMS number: EDMS-ERI-171521650, 1.0 ADVISORY COMMITTEE BRIEFING MATERIALS: AVAILABLE FOR PUBLIC RELEASE 1 Status: Approved, Date: 16 January 2019 JNJ-54135419 (esketamine) Treatment-resistant Depression Advisory Committee Briefing Document GUIDE FOR REVIEWERS This briefing document provides 3 levels of review with increasing levels of detail: The Executive Overview (Section 1, starting on page 11) provides a narrative summarizing the disease, need for novel treatments, key development program characteristics for esketamine nasal spray, study results, and conclusions. References are made to the respective supporting sections in the core document. The core document (Section 2 to Section 11, starting on page 30) includes detailed summaries and discussion in support of the Executive Overview. The appendices (starting on page 180) provide additional or more detailed information to complement brief descriptions provided in sections of the core document (e.g., demographic and baseline characteristics of the study populations, additional efficacy analyses in the Phase 3 studies, statistical methods). These appendices are referenced in the core document when relevant. This review structure allows review at varying levels of detail; however, reviewers who read at multiple levels will necessarily -

Endocannabinoid Stimulated Release of Nitric Oxide and Its Mitochondrial
A tica nal eu yt c ic a a m A r a c t Stefano et al., Pharm Anal Acta 2015, 6:6 h a P Pharmaceutica Analytica Acta DOI: 10.4172/2153-2435.1000378 ISSN: 2153-2435 Review Article Open Access Endocannabinoid Stimulated Release of Nitric Oxide and its Mitochondrial Influence Triggering Vascular Pathology George B Stefano*, Erin Quinn and Richard M Kream MitoGenetics LLC, 3 Bioscience Park Drive, Suite 307, Farmingdale, NY 11735, USA Abstract Endocannabinoids, and their respective receptors, are involved in a host of cellular regulatory activities. In part, some of these mediated effects occur by way of stimulating constitutive nitric oxide release. This occurs in endothelia, certain white blood cells, microglia, and in similar invertebrate tissues, demonstrating that this is a conserved chemical messenger system. This endocannabinoid chemical messenger system, coupled to constitutive nitric oxide release, also appears to exert regulatory effects on mitochondrial energy associated processes, further substantiating its primordial history. In this regard, it appears to offer some beneficial actions in the occurrence of reperfusion injury and stroke. The mechanism envisioned is one initiated via a hypoxic event, which does not restore normalcy, then progresses to a pro-inflammatory state, and the resultant chronic condition manifests itself in a specific disorder. This fits nicely into a vascular-associated origin for Alzheimer’s Disease, whereby the pro- inflammatory state encompasses vessels that have endothelial gaps, providing for a compromised blood brain barrier, beta amyloid deposition, and enhanced white blood cell trafficking. In time, due to the physical progression of the events, Alzheimer’s Disease occurs.