Medical Review Officer Manual
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Yerevan State Medical University After M. Heratsi
YEREVAN STATE MEDICAL UNIVERSITY AFTER M. HERATSI DEPARTMENT OF PHARMACY Balasanyan M.G. Zhamharyan A.G. Afrikyan Sh. G. Khachaturyan M.S. Manjikyan A.P. MEDICINAL CHEMISTRY HANDOUT for the 3-rd-year pharmacy students (part 2) YEREVAN 2017 Analgesic Agents Agents that decrease pain are referred to as analgesics or as analgesics. Pain relieving agents are also called antinociceptives. An analgesic may be defined as a drug bringing about insensibility to pain without loss of consciousness. Pain has been classified into the following types: physiological, inflammatory, and neuropathic. Clearly, these all require different approaches to pain management. The three major classes of drugs used to manage pain are opioids, nonsteroidal anti-inflammatory agents, and non opioids with the central analgetic activity. Narcotic analgetics The prototype of opioids is Morphine. Morphine is obtained from opium, which is the partly dried latex from incised unripe capsules of Papaver somniferum. The opium contains a complex mixture of over 20 alkaloids. Two basic types of structures are recognized among the opium alkaloids, the phenanthrene (morphine) type and the benzylisoquinoline (papaverine) type (see structures), of which morphine, codeine, noscapine (narcotine), and papaverine are therapeutically the most important. The principle alkaloid in the mixture, and the one responsible for analgesic activity, is morphine. Morphine is an extremely complex molecule. In view of establish the structure a complicated molecule was to degrade the: compound into simpler molecules that were already known and could be identified. For example, the degradation of morphine with strong base produced methylamine, which established that there was an N-CH3 fragment in the molecule. -

Identification and Quantification of Adulterants in Coffee
foods Communication Identification and Quantification of Adulterants in Coffee (Coffea arabica L.) Using FT-MIR Spectroscopy Coupled with Chemometrics Mauricio Flores-Valdez 1 , Ofelia Gabriela Meza-Márquez 2 , Guillermo Osorio-Revilla 2 and Tzayhri Gallardo-Velázquez 1,* 1 Instituto Politécnico Nacional, Escuela Nacional de Ciencias Biológicas-Santo Tomás, Departamento de Biofísica, Prolongación de Carpio y Plan de Ayala S/N, Col. Santo Tomás, Alcaldía Miguel Hidalgo, Ciudad de México C.P. 11340, Mexico; [email protected] 2 Instituto Politécnico Nacional, Escuela Nacional de Ciencias Biológicas-Zacatenco, Departamento de Ingeniería Bioquímica, Av. Wilfrido Massieu S/N, Esq. Cda, Miguel Stampa, Col. Unidad Profesional Adolfo López Mateos, Zacatenco, Alcaldía Gustavo A. Madero, Ciudad de México C.P. 07738, Mexico; [email protected] (O.G.M.-M.); [email protected] (G.O.-R.) * Correspondence: [email protected]; Tel.: +52-(55)-5729-6000 (ext. 62305) Received: 24 May 2020; Accepted: 28 June 2020; Published: 30 June 2020 Abstract: Food adulteration is an illegal practice performed to elicit economic benefits. In the context of roasted and ground coffee, legumes, cereals, nuts and other vegetables are often used to augment the production volume; however, these adulterants lack the most important coffee compound, caffeine, which has health benefits. In this study, the mid-infrared Fourier transform spectroscopy (FT-MIR) technique coupled with chemometrics was used to identify and quantify adulterants in coffee (Coffea arabica L.). Coffee samples were adulterated with corn, barley, soy, oat, rice and coffee husks, in proportions ranging from 1–30%. A discrimination model was developed using the soft independent modeling of class analogy (SIMCA) framework, and quantitative models were developed using such algorithms as the partial least squares algorithms with one variable (PLS1) and multiple variables (PLS2) and principal component regression (PCR). -

1589361321Unit V Food Adulteration.Pdf
~oodMicrobiology and the PFA Act, a trader is guilty if he sells milk to which water has been added Safety (intentional addition) or the cream of the milk has been replaced by cheap vegetable or animal fat (substitution) or simply the cream has been removed and the milk is sold as such, with a low fat content (abstraction). Unintentional contamination of the milk, due to carelessness on part of the trader is also considered as adulteration under the law. For instance, if the cans in which the trader is transporting or storing the milk, had been earlier treated with the chemicals like washing soda or boric acid or some detergent and not been washed thoroughly with water, residues of the chemicals may get mixed with the milk. Such milk would Ire considered adulterated. In addition, food is also considered to be adulterated, if it does not conform to the basic quality standards. For instance, the maximum amount of moisture allowed in a milk powder sample is 4%. If a sample is found to have greater moisture levels, it is considered to be adulterated. The malpractice of food adulteration is still widely prevalent in our country. There are very few studies on the extent and nature of food adulteration in the country. Whatever sFdies are available, are restricted to a select few cities and hence are not adequate to give a true picture for the country as a whole. The only data that are available are the reports from the food testing laboratories of the Central and State Government. According to these official reports, the extent of food adulteration in India bas been gradually diminishing from 3 1% in 1960s to less than 10% in the 1990s. -

Educational Commentary – Testing for Amphetamines and Related Compounds
EDUCATIONAL COMMENTARY – TESTING FOR AMPHETAMINES AND RELATED COMPOUNDS Learning Outcomes Upon completion of this exercise, participants will be able to: • list amphetamine-like compounds that may be detected by immunoassay screening tests for amphetamines. • describe the 3 types of amphetamine immunoassays based on their antibody specificity. • discuss common causes of false-positive results when testing for amphetamines. Correct interpretation of testing results for amphetamines and related compounds is dependent on many factors including an understanding of the nomenclature, structure, and metabolism of these compounds. The class of phenethylamine compounds having varying degrees of sympathomimetic activity include amphetamine, methamphetamine, and many other compounds known by several names including amphetamines (as a group), designer drugs often grouped together as ecstasy [3,4- methylenedioxymethamphetamine (MDMA); 3,4-methylenedioxyamphetamine (MDA), and 3,4- methylenedioxy-N-ethylamphetamine (MDEA)], and sympathomimetic amines including ephedrine, pseudoephedrine, and phenylpropanolamine found in over-the-counter (OTC) medications. Amphetamine, a primary amine, and methamphetamine, a secondary amine, have a stereogenic center and have enantiomers or optical isomers designated d (or +) for dextrorotatory and l (or -) for levorotatory. In general, the d isomers are the more physiologically active compounds, but pharmaceutical preparations may consist of either isomer or a mixture of both isomers. When the mixture contains equal concentrations of the 2 enantiomers, it is known as a racemic mixture. The existence of enantiomers for amphetamines creates analytical and interpretative problems. Immunoassay Screening The primary screening methods for detecting amphetamines are immunoassays. The structural similarity to amphetamine or methamphetamine of the compounds previously mentioned makes it difficult to produce antibodies specific for amphetamine, methamphetamine, or both. -

Cannabis Pregnancy
Wellness Articles Attached are weekly health and wellness articles provided by Alberta Health Services. As a way to help all Albertans live a healthy life, we welcome and encourage weekly newspapers, community newsletters and other publications to reproduce this information free of charge. Credit to Alberta Health Services or the identified content provider would be appreciated. If you would like to be added to the distribution list for these articles, please email: [email protected]. You will receive a monthly email containing articles for the upcoming four weeks. An archive of past wellness articles is available at http://www.albertahealthservices.ca/9966.asp Proposed publication date: February 25, 2019 Content provided by: Alberta Health Services Cannabis and Pregnancy Now that cannabis is legal in Canada, pregnant and breastfeeding women or those that might become pregnant need information on how to make healthy decisions for themselves and their baby. Throughout pregnancy, a baby’s quickly developing brain is very sensitive to harmful environments. Things that can harm a baby’s brain include certain illnesses, and being exposed to chemicals like alcohol, tobacco, tobacco-like products, cannabis (marijuana, hashish, hash oil) and other drugs. Because of this, pregnant women should not use cannabis in any form (marijuana, hashish, hash oil) because the mother and the baby’s health can be affected. Using cannabis while breastfeeding is also not advised as it is passed into breastmilk and stored there, and could affect a baby’s developing brain. Tetrahydrocannabinol (THC) is the main active chemical in the cannabis plant that gives people who use it a ‘high’. -

(12) Patent Application Publication (10) Pub. No.: US 2006/0110428A1 De Juan Et Al
US 200601 10428A1 (19) United States (12) Patent Application Publication (10) Pub. No.: US 2006/0110428A1 de Juan et al. (43) Pub. Date: May 25, 2006 (54) METHODS AND DEVICES FOR THE Publication Classification TREATMENT OF OCULAR CONDITIONS (51) Int. Cl. (76) Inventors: Eugene de Juan, LaCanada, CA (US); A6F 2/00 (2006.01) Signe E. Varner, Los Angeles, CA (52) U.S. Cl. .............................................................. 424/427 (US); Laurie R. Lawin, New Brighton, MN (US) (57) ABSTRACT Correspondence Address: Featured is a method for instilling one or more bioactive SCOTT PRIBNOW agents into ocular tissue within an eye of a patient for the Kagan Binder, PLLC treatment of an ocular condition, the method comprising Suite 200 concurrently using at least two of the following bioactive 221 Main Street North agent delivery methods (A)-(C): Stillwater, MN 55082 (US) (A) implanting a Sustained release delivery device com (21) Appl. No.: 11/175,850 prising one or more bioactive agents in a posterior region of the eye so that it delivers the one or more (22) Filed: Jul. 5, 2005 bioactive agents into the vitreous humor of the eye; (B) instilling (e.g., injecting or implanting) one or more Related U.S. Application Data bioactive agents Subretinally; and (60) Provisional application No. 60/585,236, filed on Jul. (C) instilling (e.g., injecting or delivering by ocular ion 2, 2004. Provisional application No. 60/669,701, filed tophoresis) one or more bioactive agents into the Vit on Apr. 8, 2005. reous humor of the eye. Patent Application Publication May 25, 2006 Sheet 1 of 22 US 2006/0110428A1 R 2 2 C.6 Fig. -

Levamisole: a Toxic Adulterant Found in Illicit Street Drugs
July 2020 Levamisole: A Toxic Adulterant Found in Illicit Street Drugs. GLOBAL PUBLIC HEALTH ALERT Substance abuse treatment providers, clinicians, outreach workers, public health clinics, etc. need to be aware of the following information. A dangerous drug adulterant, levamisole, is appearing with increasing frequency in illicit cocaine powder and crack cocaine, and to some extent in heroin and fentanyl. Levamisole can cause severe adverse health effects, including a reduction in the patient’s white blood cell count, a condition called agranulocytosis. THIS IS A VERY SERIOUS ILLNESS THAT NEEDS TO BE TREATED IN A HOSPITAL. SEE ATTACHED TREATMENT AND DIAGNOSIS PLAN. Background: Levamisole was initially developed in the mid-1960s as a veterinary and human anti-worming drug. In 1990, it was approved by the United States Food and Drug Administration (FDA) as a therapy for the treatment of colorectal cancer, however, by 2000 it had been withdrawn from the market due to severe adverse effects described below. Since the early 2000’s, levamisole has been in widespread use as an adulterating agent for illicit street drugs, especially cocaine, heroin, and fentanyl. Although its prevalence varies over time and geographically, LEVAMISOLE HAS AT TIMES BEEN DETECTED IN UP TO 79% OF THE COCAINE STREET SUPPLY AT VARYING PERCENTAGES, UP TO 74% BY WEIGHT. Frequent Indicators of Levamisole Recommendations for MEs & Coroners Toxicity • Test for common adulterating agents in • Unexplained fever and agranulocytosis suspected stimulant- or opioid-related • Unexplained vasculitis with purple skin death cases where levamisole related lesions over ear lobes, legs and thighs findings, such as leukopenia or necrosis, Levamisole are identified. -

(19) United States (12) Patent Application Publication (10) Pub
US 20130289061A1 (19) United States (12) Patent Application Publication (10) Pub. No.: US 2013/0289061 A1 Bhide et al. (43) Pub. Date: Oct. 31, 2013 (54) METHODS AND COMPOSITIONS TO Publication Classi?cation PREVENT ADDICTION (51) Int. Cl. (71) Applicant: The General Hospital Corporation, A61K 31/485 (2006-01) Boston’ MA (Us) A61K 31/4458 (2006.01) (52) U.S. Cl. (72) Inventors: Pradeep G. Bhide; Peabody, MA (US); CPC """"" " A61K31/485 (201301); ‘4161223011? Jmm‘“ Zhu’ Ansm’ MA. (Us); USPC ......... .. 514/282; 514/317; 514/654; 514/618; Thomas J. Spencer; Carhsle; MA (US); 514/279 Joseph Biederman; Brookline; MA (Us) (57) ABSTRACT Disclosed herein is a method of reducing or preventing the development of aversion to a CNS stimulant in a subject (21) App1_ NO_; 13/924,815 comprising; administering a therapeutic amount of the neu rological stimulant and administering an antagonist of the kappa opioid receptor; to thereby reduce or prevent the devel - . opment of aversion to the CNS stimulant in the subject. Also (22) Flled' Jun‘ 24’ 2013 disclosed is a method of reducing or preventing the develop ment of addiction to a CNS stimulant in a subj ect; comprising; _ _ administering the CNS stimulant and administering a mu Related U‘s‘ Apphcatlon Data opioid receptor antagonist to thereby reduce or prevent the (63) Continuation of application NO 13/389,959, ?led on development of addiction to the CNS stimulant in the subject. Apt 27’ 2012’ ?led as application NO_ PCT/US2010/ Also disclosed are pharmaceutical compositions comprising 045486 on Aug' 13 2010' a central nervous system stimulant and an opioid receptor ’ antagonist. -
Quantitative Drug Test Menu Section 2
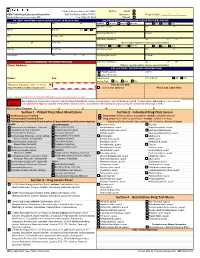
1 Guthrie Square, Sayre, PA 18840 Bill To: Client GMG Toxicology Laboratory Requisition Toll Free Phone (844) 617-4719 Insurance Request Date: _____/______/______ Medical Director: Hani Hojjati, MD Fax (570) 887-4729 Patient PATIENT INFORMATION (PLEASE PRINT IN BLACK INK) INSURANCE BILLING INFORMATION (PLEASE PRINT IN BLACK INK) Pt Last Name First M I PRIMARY Medicare Medicaid Other Ins. Self Spouse Child __ Subscriber Last Name First M Address Birth Date Sex M F Beneficiary/Member # Group # City Pt. SS# or MRN Claims Name and Address City ST ZIP ST ZIP Home Phone (Attach a copy of the patient's insurance card and information) SECONDARY Medicare Medicaid Other Ins. Self Spouse Child Employer Work Phone Subscriber Last Name First M Work Address City ST ZIP Beneficiary/Member # Group # __ CLIENT INFORMATION - REFERRING PHYSICIAN Claims Name and Address City ST ZIP Client Address: (Atttach a copy of the patient's insurance card and information) COLLECTION / REPORTING INFORMATION Copy to: FAX Results to __ CALL Results to Phone: Fax: Date Collected: Time Collected: AM PM Specimen Type: Urine Saliva Other ___________________ Physician Signature (legible - No Stamp) For Lab Use Only (Required for Medicare & Medicaid patient orders) Signed ABN Obtained Place Lab Label Here Contact Laboratory Medical Director (570-887-4719) with questions concerning medical necessity PHYSICIAN When ordering tests, the physician is required to make an independent medical necessity decision with regard to each test thelaboratory will bill. The physician also understands he or she is required NOTICE to (1) submit ICD-10 diagnosis supported in the patient's medical record as documentation of the medical necessity or (2) explain and have the patient sign an ABN. -

Substance Abuse in the Workplace Policy
Substance Abuse in the Workplace Policy Rexnord (herein referred to as “Rexnord” or the “Company”) has a strong commitment to its employees to provide a safe work environment and to promote high standards of employee performance. Consistent with the spirit and intent of this commitment, the Company has established a policy regarding substance abuse in the workplace. Further, the Company is committed to maintaining a drug-free workplace as required by “The Drug-Free Workplace Act of 1988.” Therefore, compliance with this Policy is a condition of continued employment with Rexnord. I. PURPOSE To outline the procedures to be followed by each location in order to ensure that the safety and performance of employees is not impaired by alcohol, illegal drugs or other substances. II. APPLICABILITY This policy shall apply to all employees (full-time, part-time, exempt, and non-exempt employees) as well as to all applicants who have received a conditional offer of employment. Personnel who perform their services on Company property or on a third party’s property at the request of the Company (e.g., a Company customer site), as provided under a contract either directly with the Company or through the services of an outside firm, are required to abide by this policy. It is the responsibility of the contracting firm (at its cost and expense) to ensure that its personnel are tested in conformance with this policy prior to working at / on behalf of Rexnord. III. SUBSTANCE ABUSE It is the Company’s policy that the following is prohibited and will result in discipline up to and including termination: A. -

Pharmacology and Toxicology of Amphetamine and Related Designer Drugs
Pharmacology and Toxicology of Amphetamine and Related Designer Drugs U.S. DEPARTMENT OF HEALTH AND HUMAN SERVICES • Public Health Service • Alcohol Drug Abuse and Mental Health Administration Pharmacology and Toxicology of Amphetamine and Related Designer Drugs Editors: Khursheed Asghar, Ph.D. Division of Preclinical Research National Institute on Drug Abuse Errol De Souza, Ph.D. Addiction Research Center National Institute on Drug Abuse NIDA Research Monograph 94 1989 U.S. DEPARTMENT OF HEALTH AND HUMAN SERVICES Public Health Service Alcohol, Drug Abuse, and Mental Health Administration National Institute on Drug Abuse 5600 Fishers Lane Rockville, MD 20857 For sale by the Superintendent of Documents, U.S. Government Printing Office Washington, DC 20402 Pharmacology and Toxicology of Amphetamine and Related Designer Drugs ACKNOWLEDGMENT This monograph is based upon papers and discussion from a technical review on pharmacology and toxicology of amphetamine and related designer drugs that took place on August 2 through 4, 1988, in Bethesda, MD. The review meeting was sponsored by the Biomedical Branch, Division of Preclinical Research, and the Addiction Research Center, National Institute on Drug Abuse. COPYRIGHT STATUS The National Institute on Drug Abuse has obtained permission from the copyright holders to reproduce certain previously published material as noted in the text. Further reproduction of this copyrighted material is permitted only as part of a reprinting of the entire publication or chapter. For any other use, the copyright holder’s permission is required. All other matieral in this volume except quoted passages from copyrighted sources is in the public domain and may be used or reproduced without permission from the Institute or the authors. -

Methamphetamine (Canadian Drug Summary)
www.ccsa.ca • www.ccdus.ca March 2020 Canadian Drug Summary Methamphetamine Key Points • The prevalence of methamphetamine use in the Canadian population is low (~0.2%). • Several jurisdictions report at least a three-fold increase in the use of methamphetamine over the past five years among individuals accessing treatment or harm reduction services. • Notable increases for rates of criminal violations involving methamphetamine have been observed in the last five years (2013–2018). Introduction Methamphetamine is a synthetic drug classified as a central nervous system (CNS) stimulant or psychostimulant. CNS stimulants cover a wide range of substances that act on the body by increasing the level of activity of the CNS and include caffeine, nicotine, amphetamine (e.g., Adderall®), methylphenidate (e.g., Ritalin®), MDMA (“ecstasy”), cocaine (including crack cocaine) and methamphetamine (including crystal meth).1,2 While both methamphetamine and amphetamine are psychostimulants and often grouped together, they are different drugs. A slight chemical modification of amphetamine produces methamphetamine, which has a different pharmacological profile that results in a larger release of certain neurochemicals in the brain and a stronger and more rapid physiological response. Some amphetamines are prescribed in Canada for attention-deficit hyperactivity disorder (ADHD) and narcolepsy (e.g., Adderall and Vyvanse®), but methamphetamine use is currently illegal. Methamphetamine is often made in illegal, clandestine laboratories with commonly available, inexpensive chemicals, such as ephedrine and pseudoephedrine, found in medications, among other sources. The use of these medications as precursor chemicals for methamphetamine led to stricter regulations introduced in Canada in 2006, limiting access to them by requiring they be kept behind the counter of pharmacies.3 Illegal production can be dangerous due to the toxicity of the chemicals used and the high risk of explosions.