Efficacy and Safety of Intranasal Esketamine When Tapered from Twice-Weekly Dosing to Once Per Week Dosing and Then Dosing Once Every Other Week
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Dextromethorphan Attenuates Sensorineural Hearing Loss in an Animal Model and Population-Based Cohort Study
International Journal of Environmental Research and Public Health Article Dextromethorphan Attenuates Sensorineural Hearing Loss in an Animal Model and Population-Based Cohort Study Hsin-Chien Chen 1,* , Chih-Hung Wang 1,2 , Wu-Chien Chien 3,4 , Chi-Hsiang Chung 3,4, Cheng-Ping Shih 1, Yi-Chun Lin 1,2, I-Hsun Li 5,6, Yuan-Yung Lin 1,2 and Chao-Yin Kuo 1 1 Department of Otolaryngology-Head and Neck Surgery, Tri-Service General Hospital, National Defense Medical Center, Taipei 114, Taiwan; [email protected] (C.-H.W.); [email protected] (C.-P.S.); [email protected] (Y.-C.L.); [email protected] (Y.-Y.L.); [email protected] (C.-Y.K.) 2 Graduate Institute of Medical Sciences, National Defense Medical Center, Taipei 114, Taiwan 3 School of Public Health, National Defense Medical Center, Taipei 114, Taiwan; [email protected] (W.-C.C.); [email protected] (C.-H.C.) 4 Department of Medical Research, Tri-Service General Hospital, National Defense Medical Center, Taipei 114, Taiwan 5 Department of Pharmacy Practice, Tri-Service General Hospital, National Defense Medical Center, Taipei 114, Taiwan; [email protected] 6 School of Pharmacy, National Defense Medical Center, Taipei 114, Taiwan * Correspondence: [email protected]; Tel.: +886-2-8792-7192; Fax: +886-2-8792-7193 Received: 31 July 2020; Accepted: 28 August 2020; Published: 31 August 2020 Abstract: The effect of dextromethorphan (DXM) use in sensorineural hearing loss (SNHL) has not been fully examined. We conducted an animal model and nationwide retrospective matched-cohort study to explore the association between DXM use and SNHL. -

The Effect of Morphine-Lidocaine-Ketamine
THE EFFECT OF MORPHINE-LIDOCAINE-KETAMINE- DEXMEDETOMIDINE CO-INFUSION ON MINIMUM ALVEOLAR CONCENTRATION OF ISOFLURANE IN DOGS Thesis Presented in Partial Fulfillment of the Requirements for the Degree of Master of Science in the Graduate School of The Ohio State University By Lisa Michelle Sams, D.V.M. Graduate Program in Comparative and Veterinary Medicine The Ohio State University 2011 Thesis Committee: Dr. Phillip Lerche, Advisor Dr. Richard M. Bednarski Dr. John A.E. Hubbell Copyright by Lisa Michelle Sams 2011 ABSTRACT The purpose of this study was to determine the effects of an infusion of dexmedetomidine, a co-infusion of morphine-lidocaine-ketamine (MLK), and a co- infusion of dexmedetomidine-morphine-lidocaine-ketamine (alpha-MLK) on minimum alveolar concentration (MAC) of isoflurane in dogs. The MAC of an inhalant anesthetic required to prohibit purposeful movement is a measure of anesthetic potency (Eger et al 1965). Isoflurane is the most commonly used inhalant anesthetic in veterinary practice (Lozano et al 2009), but has potent vasodilatory effects and causes a dose-dependent decrease in mean arterial pressure in anesthetized dogs (Steffey and Howland 1977). Additional drugs are used during anesthesia to decrease the inhalant anesthetic requirement, a concept referred to as balanced anesthesia. Each of the drugs we infused has a different central nervous system receptor mechanism of action. Co-infusion of MLK, as well as the infusion of each drug separately, has been shown to reduce MAC in isoflurane-anesthetized dogs (Muir et al 2003). Dexmedetomidine, an alpha-2 agonist, has been shown to reduce isoflurane MAC in dogs (Pascoe et al 2006). -

The In¯Uence of Medication on Erectile Function
International Journal of Impotence Research (1997) 9, 17±26 ß 1997 Stockton Press All rights reserved 0955-9930/97 $12.00 The in¯uence of medication on erectile function W Meinhardt1, RF Kropman2, P Vermeij3, AAB Lycklama aÁ Nijeholt4 and J Zwartendijk4 1Department of Urology, Netherlands Cancer Institute/Antoni van Leeuwenhoek Hospital, Plesmanlaan 121, 1066 CX Amsterdam, The Netherlands; 2Department of Urology, Leyenburg Hospital, Leyweg 275, 2545 CH The Hague, The Netherlands; 3Pharmacy; and 4Department of Urology, Leiden University Hospital, P.O. Box 9600, 2300 RC Leiden, The Netherlands Keywords: impotence; side-effect; antipsychotic; antihypertensive; physiology; erectile function Introduction stopped their antihypertensive treatment over a ®ve year period, because of side-effects on sexual function.5 In the drug registration procedures sexual Several physiological mechanisms are involved in function is not a major issue. This means that erectile function. A negative in¯uence of prescrip- knowledge of the problem is mainly dependent on tion-drugs on these mechanisms will not always case reports and the lists from side effect registries.6±8 come to the attention of the clinician, whereas a Another way of looking at the problem is drug causing priapism will rarely escape the atten- combining available data on mechanisms of action tion. of drugs with the knowledge of the physiological When erectile function is in¯uenced in a negative mechanisms involved in erectile function. The way compensation may occur. For example, age- advantage of this approach is that remedies may related penile sensory disorders may be compen- evolve from it. sated for by extra stimulation.1 Diminished in¯ux of In this paper we will discuss the subject in the blood will lead to a slower onset of the erection, but following order: may be accepted. -

)&F1y3x PHARMACEUTICAL APPENDIX to THE
)&f1y3X PHARMACEUTICAL APPENDIX TO THE HARMONIZED TARIFF SCHEDULE )&f1y3X PHARMACEUTICAL APPENDIX TO THE TARIFF SCHEDULE 3 Table 1. This table enumerates products described by International Non-proprietary Names (INN) which shall be entered free of duty under general note 13 to the tariff schedule. The Chemical Abstracts Service (CAS) registry numbers also set forth in this table are included to assist in the identification of the products concerned. For purposes of the tariff schedule, any references to a product enumerated in this table includes such product by whatever name known. Product CAS No. Product CAS No. ABAMECTIN 65195-55-3 ACTODIGIN 36983-69-4 ABANOQUIL 90402-40-7 ADAFENOXATE 82168-26-1 ABCIXIMAB 143653-53-6 ADAMEXINE 54785-02-3 ABECARNIL 111841-85-1 ADAPALENE 106685-40-9 ABITESARTAN 137882-98-5 ADAPROLOL 101479-70-3 ABLUKAST 96566-25-5 ADATANSERIN 127266-56-2 ABUNIDAZOLE 91017-58-2 ADEFOVIR 106941-25-7 ACADESINE 2627-69-2 ADELMIDROL 1675-66-7 ACAMPROSATE 77337-76-9 ADEMETIONINE 17176-17-9 ACAPRAZINE 55485-20-6 ADENOSINE PHOSPHATE 61-19-8 ACARBOSE 56180-94-0 ADIBENDAN 100510-33-6 ACEBROCHOL 514-50-1 ADICILLIN 525-94-0 ACEBURIC ACID 26976-72-7 ADIMOLOL 78459-19-5 ACEBUTOLOL 37517-30-9 ADINAZOLAM 37115-32-5 ACECAINIDE 32795-44-1 ADIPHENINE 64-95-9 ACECARBROMAL 77-66-7 ADIPIODONE 606-17-7 ACECLIDINE 827-61-2 ADITEREN 56066-19-4 ACECLOFENAC 89796-99-6 ADITOPRIM 56066-63-8 ACEDAPSONE 77-46-3 ADOSOPINE 88124-26-9 ACEDIASULFONE SODIUM 127-60-6 ADOZELESIN 110314-48-2 ACEDOBEN 556-08-1 ADRAFINIL 63547-13-7 ACEFLURANOL 80595-73-9 ADRENALONE -

WO 2013/169741 Al 14 November 2013 (14.11.2013) P O P C T
(12) INTERNATIONAL APPLICATION PUBLISHED UNDER THE PATENT COOPERATION TREATY (PCT) (19) World Intellectual Property Organization International Bureau (10) International Publication Number (43) International Publication Date WO 2013/169741 Al 14 November 2013 (14.11.2013) P O P C T (51) International Patent Classification: (81) Designated States (unless otherwise indicated, for every A61K 31/401 (2006.01) A61P 9/12 (2006.01) kind of national protection available): AE, AG, AL, AM, A61K 31/405 (2006.01) A61P 25/00 (2006.01) AO, AT, AU, AZ, BA, BB, BG, BH, BN, BR, BW, BY, A61K 31/7048 (2006.01) BZ, CA, CH, CL, CN, CO, CR, CU, CZ, DE, DK, DM, DO, DZ, EC, EE, EG, ES, FI, GB, GD, GE, GH, GM, GT, (21) International Application Number: HN, HR, HU, ID, IL, IN, IS, JP, KE, KG, KM, KN, KP, PCT/US20 13/039904 KR, KZ, LA, LC, LK, LR, LS, LT, LU, LY, MA, MD, (22) International Filing Date: ME, MG, MK, MN, MW, MX, MY, MZ, NA, NG, NI, 7 May 2013 (07.05.2013) NO, NZ, OM, PA, PE, PG, PH, PL, PT, QA, RO, RS, RU, RW, SC, SD, SE, SG, SK, SL, SM, ST, SV, SY, TH, TJ, (25) Filing Language: English TM, TN, TR, TT, TZ, UA, UG, US, UZ, VC, VN, ZA, (26) Publication Language: English ZM, ZW. (30) Priority Data: (84) Designated States (unless otherwise indicated, for every 61/644,134 8 May 2012 (08.05.2012) US kind of regional protection available): ARIPO (BW, GH, GM, KE, LR, LS, MW, MZ, NA, RW, SD, SL, SZ, TZ, (72) Inventors; and UG, ZM, ZW), Eurasian (AM, AZ, BY, KG, KZ, RU, TJ, (71) Applicants : STEIN, Emily A. -

(12) Patent Application Publication (10) Pub. No.: US 2012/0115729 A1 Qin Et Al
US 201201.15729A1 (19) United States (12) Patent Application Publication (10) Pub. No.: US 2012/0115729 A1 Qin et al. (43) Pub. Date: May 10, 2012 (54) PROCESS FOR FORMING FILMS, FIBERS, Publication Classification AND BEADS FROM CHITNOUS BOMASS (51) Int. Cl (75) Inventors: Ying Qin, Tuscaloosa, AL (US); AOIN 25/00 (2006.01) Robin D. Rogers, Tuscaloosa, AL A6II 47/36 (2006.01) AL(US); (US) Daniel T. Daly, Tuscaloosa, tish 9.8 (2006.01)C (52) U.S. Cl. ............ 504/358:536/20: 514/777; 426/658 (73) Assignee: THE BOARD OF TRUSTEES OF THE UNIVERSITY OF 57 ABSTRACT ALABAMA, Tuscaloosa, AL (US) (57) Disclosed is a process for forming films, fibers, and beads (21) Appl. No.: 13/375,245 comprising a chitinous mass, for example, chitin, chitosan obtained from one or more biomasses. The disclosed process (22) PCT Filed: Jun. 1, 2010 can be used to prepare films, fibers, and beads comprising only polymers, i.e., chitin, obtained from a suitable biomass, (86). PCT No.: PCT/US 10/36904 or the films, fibers, and beads can comprise a mixture of polymers obtained from a suitable biomass and a naturally S3712). (4) (c)(1), Date: Jan. 26, 2012 occurring and/or synthetic polymer. Disclosed herein are the (2), (4) Date: an. AO. films, fibers, and beads obtained from the disclosed process. O O This Abstract is presented solely to aid in searching the sub Related U.S. Application Data ject matter disclosed herein and is not intended to define, (60)60) Provisional applicationpp No. 61/182,833,sy- - - s filed on Jun. -

Pharmacogenetics of Ketamine Metabolism And
Pharmacogenetics of Ketamine Metabolism and Immunopharmacology of Ketamine Yibai Li B.HSc. (Hons) Discipline of Pharmacology, School of Medical Sciences, Faculty of Health Sciences, The University of Adelaide September 2014 A thesis submitted for the Degree of PhD (Medicine) Table of contents TABLE OF CONTENTS .............................................................................................. I LIST OF FIGURES ....................................................................................................IV LIST OF TABLES ......................................................................................................IV ABSTRACT ............................................................................................................... V DECLARATION .......................................................................................................VIII ACKNOWLEDGEMENTS ..........................................................................................IX ABBREVIATIONS .....................................................................................................XI CHAPTER 1. INTRODUCTION .................................................................................. 1 1.1 A historical overview of ketamine ........................................................................................ 1 1.2 Structure and Chemistry ....................................................................................................... 3 1.3 Classical analgesic mechanisms of ketamine ................................................................... -

Opioid Withdrawal ��������������������������������������������������������������������������������������������������� 15 Mark S
Magdalena Anitescu Honorio T. Benzon Mark S. Wallace Editors Challenging Cases and Complication Management in Pain Medicine 123 Challenging Cases and Complication Management in Pain Medicine Magdalena Anitescu Honorio T. Benzon • Mark S. Wallace Editors Challenging Cases and Complication Management in Pain Medicine Editors Magdalena Anitescu Honorio T. Benzon Department of Anesthesia and Critical Care Department of Anesthesiology University of Chicago Medicine Northwestern University Chicago, IL Feinberg School of Medicine USA Chicago, IL USA Mark S. Wallace Division of Pain Medicine Department of Anesthesiology University of California San Diego School of Medicine La Jolla, CL USA ISBN 978-3-319-60070-3 ISBN 978-3-319-60072-7 (eBook) https://doi.org/10.1007/978-3-319-60072-7 Library of Congress Control Number: 2017960332 © Springer International Publishing AG 2018 This work is subject to copyright. All rights are reserved by the Publisher, whether the whole or part of the material is concerned, specifically the rights of translation, reprinting, reuse of illustrations, recitation, broadcasting, reproduction on microfilms or in any other physical way, and transmission or information storage and retrieval, electronic adaptation, computer software, or by similar or dissimilar methodology now known or hereafter developed. The use of general descriptive names, registered names, trademarks, service marks, etc. in this publication does not imply, even in the absence of a specific statement, that such names are exempt from the relevant protective laws and regulations and therefore free for general use. The publisher, the authors and the editors are safe to assume that the advice and information in this book are believed to be true and accurate at the date of publication. -

Hallucinogens
Hallucinogens What are hallucinogens? Hallucinogens are a diverse group of drugs that alter a person’s awareness of their surroundings as well as their own thoughts and feelings. They are commonly split into two categories: classic hallucinogens (such as LSD) and dissociative drugs (such as PCP). Both types of hallucinogens can cause hallucinations, or sensations and images that seem real though they are not. Additionally, dissociative drugs can cause users to feel out of control or disconnected from their body and environment. Some hallucinogens are extracted from plants or mushrooms, and some are synthetic (human- made). Historically, people have used hallucinogens for religious or healing rituals. More recently, people report using these drugs for social or recreational purposes, including to have fun, deal with stress, have spiritual experiences, or just to feel different. Common classic hallucinogens include the following: • LSD (D-lysergic acid diethylamide) is one of the most powerful mind-altering chemicals. It is a clear or white odorless material made from lysergic acid, which is found in a fungus that grows on rye and other grains. LSD has many other street names, including acid, blotter acid, dots, and mellow yellow. • Psilocybin (4-phosphoryloxy-N,N- dimethyltryptamine) comes from certain types of mushrooms found in tropical and subtropical regions of South America, Mexico, and the United States. Some common names for Blotter sheet of LSD-soaked paper squares that users psilocybin include little smoke, magic put in their mouths. mushrooms, and shrooms. Photo by © DEA • Peyote (mescaline) is a small, spineless cactus with mescaline as its main ingredient. Peyote can also be synthetic. -
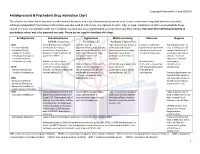
Antidepressant & Psychedelic Drug Interaction Chart
Copyright Psychedelic School 8/2020 Antidepressant & Psychedelic Drug Interaction Chart This chart is not intended to be used to make medical decisions and is for informational purposes only. It was constructed using data whenever possible, although extrapolation from known information was also used to inform risk. Any decision to start, stop, or taper medication and/or use psychedelic drugs should be made in conjunction with your healthcare provider(s). It is recommended to not perform any illicit activity. This chart the intellectual property of psychedelic school and is for personal use only. Please do not copy or distribute this chart. Antidepressant Phenethylamines Tryptamines MAOI-containing Ketamine Ibogaine -MDMA, mescaline -Psilocybin, LSD -Ayahuasca, Syrian Rue SSRIs Taper & discontinue at least 2 Consider taper & Taper & discontinue at least 2 Has been studied and Taper & discontinue at · Paroxetine (Paxil) weeks prior (all except discontinuation at least 2 weeks weeks prior (all except found effective both with least 2 weeks prior (all · Sertraline (Zoloft) fluoxetine) or 6 weeks prior prior (all except fluoxetine) or 6 fluoxetine) or 6 weeks prior and without concurrent except fluoxetine) or 6 · Citalopram (Celexa) (fluoxetine only) due to loss of weeks prior (fluoxetine only) (fluoxetine only) due to use of antidepressants weeks prior (fluoxetine · Escitalopram (Lexapro) psychedelic effect due to potential loss of potential risk of serotonin only) due to risk of · Fluxoetine (Prozac) psychedelic effect syndrome additive QTc interval · Fluvoxamine (Luvox) MDMA is unable to cause Recommended prolongation, release of serotonin when the Chronic antidepressant use may Life threatening toxicities can to be used in conjunction arrhythmias, or SPARI serotonin reuptake pump is result in down-regulation of occur with these with oral antidepressants cardiotoxicity · Vibryyd (Vilazodone) blocked. -

Janssen Research & Development, LLC Advisory Committee Briefing
Janssen Research & Development, LLC Advisory Committee Briefing Document Esketamine Nasal Spray for Patients with Treatment-resistant Depression JNJ-54135419 (esketamine) Status: Approved Date: 16 January 2019 Prepared by: Janssen Research & Development, LLC EDMS number: EDMS-ERI-171521650, 1.0 ADVISORY COMMITTEE BRIEFING MATERIALS: AVAILABLE FOR PUBLIC RELEASE 1 Status: Approved, Date: 16 January 2019 JNJ-54135419 (esketamine) Treatment-resistant Depression Advisory Committee Briefing Document GUIDE FOR REVIEWERS This briefing document provides 3 levels of review with increasing levels of detail: The Executive Overview (Section 1, starting on page 11) provides a narrative summarizing the disease, need for novel treatments, key development program characteristics for esketamine nasal spray, study results, and conclusions. References are made to the respective supporting sections in the core document. The core document (Section 2 to Section 11, starting on page 30) includes detailed summaries and discussion in support of the Executive Overview. The appendices (starting on page 180) provide additional or more detailed information to complement brief descriptions provided in sections of the core document (e.g., demographic and baseline characteristics of the study populations, additional efficacy analyses in the Phase 3 studies, statistical methods). These appendices are referenced in the core document when relevant. This review structure allows review at varying levels of detail; however, reviewers who read at multiple levels will necessarily -

Psychedelics in Psychiatry: Neuroplastic, Immunomodulatory, and Neurotransmitter Mechanismss
Supplemental Material can be found at: /content/suppl/2020/12/18/73.1.202.DC1.html 1521-0081/73/1/202–277$35.00 https://doi.org/10.1124/pharmrev.120.000056 PHARMACOLOGICAL REVIEWS Pharmacol Rev 73:202–277, January 2021 Copyright © 2020 by The Author(s) This is an open access article distributed under the CC BY-NC Attribution 4.0 International license. ASSOCIATE EDITOR: MICHAEL NADER Psychedelics in Psychiatry: Neuroplastic, Immunomodulatory, and Neurotransmitter Mechanismss Antonio Inserra, Danilo De Gregorio, and Gabriella Gobbi Neurobiological Psychiatry Unit, Department of Psychiatry, McGill University, Montreal, Quebec, Canada Abstract ...................................................................................205 Significance Statement. ..................................................................205 I. Introduction . ..............................................................................205 A. Review Outline ........................................................................205 B. Psychiatric Disorders and the Need for Novel Pharmacotherapies .......................206 C. Psychedelic Compounds as Novel Therapeutics in Psychiatry: Overview and Comparison with Current Available Treatments . .....................................206 D. Classical or Serotonergic Psychedelics versus Nonclassical Psychedelics: Definition ......208 Downloaded from E. Dissociative Anesthetics................................................................209 F. Empathogens-Entactogens . ............................................................209