The Effect of Morphine-Lidocaine-Ketamine
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Ketamine Homogeneous Enzyme Immunoassay (HEIA™)
Ketamine Homogeneous Enzyme Immunoassay (HEIA™) Exclusively from Immunalysis Formula: C13H16CINO Semi-Quantitative or Qualitative Testing Systematic Name: (RS)- 2- (2- chlorophenyl)- 2- (methylamino)cyclohexanone Accurate and reliable Brand Names: Ketanest®, Ketaset®, Ketalar® Ready to use About Ketamine: Ketamine is an anesthetic agent used in the United States since 1972 for veterinary and pediatric medicine. It is also used in the treatment of depression and postoperative pain management. However, in recent years it has gained popularity as a street drug used at clubs and raves due to its hallucinogenic effects. Administration: Oral; intravenous; intramuscular; insufflation Elimination: Ketamine metabolizes by N-demethylation to Norketamine and further dehydrogenates to Dehydronorketamine. After 72 hours of a single dose, 2.3% of Ketamine is unchanged, 1.6% is Norketamine, 16.2% is Dehydronorketamine, and 80% is hydroxylated derivatives of Ketamine.1,2 Abuse Potential: An overdose can cause unconsciousness and dangerously slowed breathing. 1) R. Baselt, Disposition of Toxic Drugs and Chemicals in Man, Fourth Edition, p. 412-414. 2) K. Moore, J.Skerov, B.Levine, and A.Jacobs, Urine Concentrations of Ketamine and Norketamine Following Illegal Consumption, J.Anal, Toxicol. 25: 583-588 (2001). Ketanest® is a registered trademark of Pfizer, Inc., Ketaset® is a trademark of ZOETIS W LLC., Ketalar® is a trademark of PAR STERILE PRODUCTS, LLC. Tel 909.482.0840 | Toll Free 888.664.8378 | Fax 909.482.0850 ISO13485:2003 www.immunalysis.com CERTIFIED -

ARK™ Ketamine Assay Package Insert
The ARK Ketamine Assay provides only a preliminary analytical test result. A more specific alternative chemical method must be used in order to obtain a confirmed positive analytical result. Gas Chromatography/Mass Spectrometry (GC/MS) or Liquid Chromatography/tandem Mass Spectrometry (LC-MS/MS) is the preferred confirmatory method. Clinical consideration and professional judgment should be exercised with any drug test result, particularly when the For Criminal Justice and Forensic Use Only preliminary test result is positive. 3 SUMMARY AND EXPLANATION OF THE TEST Ketamine ((+/-)-2-(2-chlorophenyl)-2-(methylamino)cyclohexanone) is a synthetic, non- RK™ Ketamine Assay barbiturate and rapid-acting general anesthetic that is indicated for use in both human and A veterinary surgical procedures.1,2 This ARK Diagnostics, Inc. package insert for the ARK Ketamine Assay must be read prior to use. Package insert instructions must be followed accordingly. The assay provides a simple Ketamine is a Schedule III substance under the United States Controlled Substances Act for and rapid analytical screening procedure for detecting ketamine in urine. Reliability of the its potential for abuse and risk of dependence. Ketamine is structurally and pharmacologically assay results cannot be guaranteed if there are any deviations from the instructions in this similar to phencyclidine (PCP), but is less potent, has a faster onset and shorter duration of package insert. action relative to PCP. Ketamine produces a variety of symptoms including, but not limited to anxiety, dysphoria, disorientation, insomnia, flashbacks, hallucinations, and psychotic episodes.1,3 CUSTOMER SERVICE Following administration in humans, ketamine is N-demethylated by liver microsomal ARK Diagnostics, Inc. -

Dextromethorphan and Memantine After Ketamine Analgesia: a Randomized Control Trial
Drug Design, Development and Therapy Dovepress open access to scientific and medical research Open Access Full Text Article ORIGINAL RESEARCH Dextromethorphan and memantine after ketamine analgesia: a randomized control trial This article was published in the following Dove Press journal: Drug Design, Development and Therapy Elodie Martin,1 Marc Sorel,2 Purpose: Intravenous ketamine is often prescribed in severe neuropathic pain. Oral N- 3 Véronique Morel, Fabienne methyl-D-aspartate receptor (NMDAR) antagonists might prolong pain relief, reducing the 4 4 Marcaillou, Pascale Picard, frequency of ketamine infusions and hospital admissions. This clinical trial aimed at asses- Noémie Delage,4 Florence sing whether oral dextromethorphan or memantine might prolong pain relief after intrave- Tiberghien,5 Marie-Christine 6 6 nous ketamine. Crosmary, Mitra Najjar, Renato Colamarino,6 Christelle Créach,7,8 Patients and methods: A multicenter randomized controlled clinical trial included 60 Béatrice Lietar,7 Géraldine Brumauld patients after ketamine infusion for refractory neuropathic pain. Dextromethorphan (90 mg/ de Montgazon,9 Anne Margot- day), memantine (20 mg/day) or placebo was given for 12 weeks (n=20 each) after ketamine 10 11,12 Duclot, Marie-Anne Loriot, infusion. The primary endpoint was pain intensity at one month. Secondary endpoints 11,12 13 Céline Narjoz, Céline Lambert, included pain, sleep, anxiety, depression, cognitive function and quality of life evaluations 13 1,3 Bruno Pereira, Gisèle Pickering up to 12 weeks. 1Université Clermont Auvergne, Pharmacologie Results: At 1 month, dextromethorphan maintained ketamine pain relief (Numeric Pain Fondamentale Et Clinique de la Douleur, Neuro- Dol, Inserm 1107, F-63000 Clermont-Ferrand, Scale: 4.01±1.87 to 4.05±2.61, p=0.53) and diminished pain paroxysms (p=0.03) while pain France; 2Centre D’evaluation et de Traitement de intensity increased significantly with memantine and placebo (p=0.04). -

FSU ETD Template
Florida State University Libraries Electronic Theses, Treatises and Dissertations The Graduate School 2018 Sex Differences in the Effects of Low- Dose Ketamine in Rats: A Behavioral, Pharmacokinetic and Pharmacodynamic Analysis Samantha K. Saland Follow this and additional works at the DigiNole: FSU's Digital Repository. For more information, please contact [email protected] FLORIDA STATE UNIVERSITY COLLEGE OF MEDICINE SEX DIFFERENCES IN THE EFFECTS OF LOW-DOSE KETAMINE IN RATS: A BEHAVIORAL, PHARMACOKINETIC AND PHARMACODYNAMIC ANALYSIS By SAMANTHA K. SALAND A Dissertation submitted to the Department of Biomedical Sciences in partial fulfillment of the requirements for the degree of Doctor of Philosophy 2018 Samantha Saland defended this dissertation on April 18, 2018. The members of the supervisory committee were: Mohamed Kabbaj Professor Directing Dissertation Thomas Keller University Representative James Olcese Committee Member Branko Stefanovic Committee Member Zuoxin Wang Committee Member The Graduate School has verified and approved the above-named committee members, and certifies that the dissertation has been approved in accordance with university requirements. ii I dedicate this work to my loving husband and to my parents—without their endless encouragement and unconditional support throughout the years, this would not have been possible. iii ACKNOWLEDGEMENTS I would like to acknowledge all those in the Department of Biomedical Sciences here at Florida State University who have made it possible for me to succeed, not only through financial and research support, but by providing an environment of opportunity, understanding and encouragement time and again during my time in the graduate program. I would also like to express my gratitude to my committee members for their continued guidance and support throughout all these years—thank you for challenging me and expanding my continuous search for knowledge. -

Role and Advantageousness of Ketamine
a & hesi C st lin e ic n a A l Journal of Anesthesia and Clinical f R o e l s e a a n Weinbroum, J Anesth Clin Res 2018, 9:5 r r c u h o J Research DOI: 10.4172/2155-6148.1000827 ISSN: 2155-6148 Review Article Open Access Role and Advantageousness of Ketamine in Obese and Non-Obese Patients: Peri-Interventional Considerations Avi A Weinbroum* Department of Research and Development, Tel Aviv Sourasky Medical Center affiliated to the Sackler Faculty of Medicine, Tel Aviv University, Tel Aviv, Israel *Corresponding author: Avi A Weinbroum, Department of Research and Development, Tel Aviv Sourasky Medical Center affiliated to the Sackler Faculty of Medicine, Tel Aviv University, Tel Aviv, Israel, Tel: +972-3-5440904; E-mail: [email protected] Received date: May 16, 2018; Accepted date: May 25, 2018; Published date: May 29, 2018 Copyright: ©2018 Weinbroum AA, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Abstract Obese and morbidly obese patients are a growing group of individuals that generates medical, social and economic problems worldwide. They undergo various interventions that require anesthesia and/or analgesia. Despite their healthy look, these individuals are graded at high ASA physical status, mainly because of their impaired respiratory and cardiovascular conditions, and the metabolic changes their body undergoes. Opioids are the default drugs for perioperative analgesia. Nevertheless, their use has reached a frightening epidemic-like condition worldwide. -

An Experimental Approach to Detect the Presence of the Date Rape Drug Ketamine in Non-Biological Samples”
IOSR Journal of Environmental Science, Toxicology and Food Technology (IOSR-JESTFT) e-ISSN: 2319-2402,p- ISSN: 2319-2399.Volume 9, Issue 6 Ver. II (Jun. 2015), PP 31-35 www.iosrjournals.org “An Experimental Approach to Detect the Presence of the Date Rape Drug Ketamine in Non-Biological Samples” Ruchi Pandey I. Introduction 1.1 What Is Ketamine Ketamine is a drug used in human and veterinary medicine, primarily for the induction and maintenance of general anesthesia, usually in combination with a sedative. Other uses include sedation in intensive care, analgesia (particularly in emergency medicine), and treatment of bronchospasm. Ketamine has a wide range of effects in humans, including analgesia, anesthesia,hallucinations, elevated blood pressure, and bronchodilation (Peck, 2008). Like other drugs of its class, such as tiletamine and phencyclidine (PCP), ketamine induces a state referred to as "dissociative anesthesia (Bergman, 1999) and is used as a recreational drug( Table 1). Table 1: Ketamine KETAMINE Systematic IUPAC Name (RS)-2-(2-Chlorophenyl)-2-(methylamino)cyclohexanone Chemical formula C13H16ClNO Molecular mass 237.725 g/mol 1.2 Stucture Of Ketamine Ketamine is a chiral compound. Most pharmaceutical preparations of ketamine are racemic; however, some brands reportedly have (mostly undocumented) differences in their enantiomeric proportions. The more active enantiomer, (S)-ketamine, is also available for medical use under the brand name Ketanest S(Krüger, 1998) (Figure 1). Figure 1: Ketamine structure Ketamine is a "core" medicine in the World Health Organization's "Essential Drugs List", a list of minimum medical needs for a basic healthcare system. Its hydrochloridesalt is sold as KETANEST, KETASET and KETALAR. -

SDTL News January 2010 Volume 1 Issue 1
SDTL News January 2010 Volume 1 Issue 1 Clients receive custom solu- Phosphatidylethanol test more sensitive than CDT marker tions with USDTL by Douglas Lewis by Heather Sliwinski President and Scientific Director Lund University method vs. USDTL method PEth Sales and Marketing Associate Recent studies have A drug treatment program participant claims indicated that the direct they are sober. The program supervisor suspects alcohol biomarker phos- a relapse. The participant is using an unusual phatidylethanol (PEth) is drug of abuse. After hours of grueling research, superior to indirect mark- the supervisor still cannot find a laboratory that ers like carbohydrate de- tests for the drug, leaving them without options ficient transferrin (CDT). to monitor their participant. PEth is a pathological Clients of USDTL run into the same ob- phospholipid formed in tis- stacles, but experience different outcomes. We sues only by the action of assist our clients by tailoring a monitoring pro- phospholipase D on phos- gram to meet their specific needs, even if the phatidylcholine and etha- solution does not yet exist. nol. PEth in blood remains Recently, a valu- in the red cell membrane able client contacted until it spontaneously hy- USDTL concern- drolyses or is oxidized by ing a sevoflurane lipid peroxidation. abuser in their treat- USDTL took part in Dr. ment program. The Marques’ DUI and biomar- rhosis, among others, are present. Also, im- program suspected kers research by re-analyzing 281 blood proved test methods in PEth appear to have a relapse, while the specimens that had been previously analyzed reduced the other issues related to gender and participant denied it. -

Efficacy and Safety of Intranasal Esketamine When Tapered from Twice-Weekly Dosing to Once Per Week Dosing and Then Dosing Once Every Other Week
Janssen Research & Development * Clinical Protocol A Double-Blind, Doubly-Randomized, Placebo-Controlled Study of Intranasal Esketamine in an Adaptive Treatment Protocol to Assess Safety and Efficacy in Treatment-Resistant Depression (SYNAPSE) Protocol ESKETINTRD2003; Phase 2a AMENDMENT INT-3 JNJ-54135419 (esketamine) *Janssen Research & Development is a global organization that operates through different legal entities in various countries. Therefore, the legal entity acting as the sponsor for Janssen Research & Development studies may vary, such as, but not limited to Janssen Biotech, Inc.; Janssen Products, LP; Janssen Biologics, BV; Janssen-Cilag International NV; Janssen, Inc; Janssen Infectious Diseases BVBA; Janssen R&D Ireland; or Janssen Research & Development, LLC. The term “sponsor” is used throughout the protocol to represent these various legal entities; the sponsor is identified on the Contact Information page that accompanies the protocol. This study will be conducted under US Food & Drug Administration IND regulations (21 CFR Part 312). EudraCT NUMBER: 2013-004005-11 Status: Approved Date: 28 April 2014 Prepared by: Janssen Research & Development, LLC EDMS No & Version: EDMS-ERI-71950055:5.0 GCP Compliance: This study will be conducted in compliance with Good Clinical Practice, and applicable regulatory requirements. Confidentiality Statement The information in this document contains trade secrets and commercial information that are privileged or confidential and may not be disclosed unless such disclosure is required by applicable law or regulations. In any event, persons to whom the information is disclosed must be informed that the information is privileged or confidential and may not be further disclosed by them. These restrictions on disclosure will apply equally to all future information supplied to you that is indicated as privileged or confidential. -
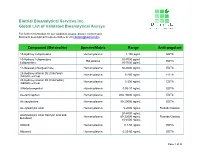
Biotrial Bioanalytical Services Inc. Global List of Validated Bioanalytical Assays
Biotrial Bioanalytical Services Inc. Global List of Validated Bioanalytical Assays For further information on our validated assays, please contact your Business development representative or via [email protected] Compound (Metabolite) Species/Matrix Range Anticoagulant 15-Hydroxy Lubiprostone Human plasma 1-150 pgmL EDTA 15-Hydroxy Lubiprostone 35-7000 pg/mL Rat plasma EDTA Lubiprostone 35-7000 pg/mL 17-Desacetyl-Norgestimate Human plasma 50-5000 pg/mL EDTA 25-Hydroxy-vitamin D2 (Calciferol) Human plasma 5-250 ng/mL EDTA (DEQAS certified) 25-Hydroxy-vitamin D3 (Calcifediol) Human plasma 5-250 ng/mL EDTA (DEQAS certified) 3-Ketodesogestrel Human plasma 0.05-10 ng/mL EDTA Acetaminophen Human plasma 200-10000 ng/mL EDTA Acetazolamine Human plasma 50-20000 ng/mL EDTA Acetylsalicylic Acid Human plasma 5-2000 ng/mL Fluoride/Oxalate 20-8000 ng/mL Acetylsalicylic Acid, Salicylic acid and Human plasma 80-32000 ng/mL Fluoride/Oxalate Butalbital 10-4000 ng/mL Afatinib Human plasma 0.1-50 ng/mL EDTA Albuterol Human plasma 0.25-50 ng/mL EDTA Page 1 of 28 Biotrial Bioanalytical Services Inc. Global List of Validated Bioanalytical Assays For further information on our validated assays, please contact your Business development representative or via [email protected] Compound (Metabolite) Species/Matrix Range Anticoagulant Alendronate Human urine 1-200 ng/mL N/A Alfuzosin Human plasma 0.15-30 ng/mL EDTA Aliskiren Human plasma 1-500 ng/mL EDTA Alprazolam Human plasma 0.25-25 ng/mL EDTA Amlodipine Human plasma 0.1-15 ng/mL EDTA Anagrelide Human plasma 0.05-11 ng/mL EDTA 0.5-150 ng/mL D,L-Amphetamine Human plasma EDTA 0.25-30 ng/mL Anastrazole Human plasma 0.1-20 ng/mL EDTA Aripiprazole Human plasma 0.5-100 ng/mL EDTA Asenapine Human plasma 0.05-20 ng/mL EDTA Asoxime Human plasma 0.1-30 µg/mL EDTA Asoxime Human urine 1-300 µg/mL N/A Page 2 of 28 Biotrial Bioanalytical Services Inc. -

Consensus Guidelines on the Use of Intravenous Ketamine Infusions for Chronic Pain from the American Society of Regional Anesthe
CHRONIC AND INTERVENTIONAL PAIN SPECIAL ARTICLE Consensus Guidelines on the Use of Intravenous Ketamine Infusions for Chronic Pain From the American Society of Regional Anesthesia and Pain Medicine, the American Academy of Pain Medicine, and the American Society 08/03/2018 on BhDMf5ePHKav1zEoum1tQfN4a+kJLhEZgbsIHo4XMi0hCywCX1AWnYQp/IlQrHD3ctdU4DsFBzQV47uVtFPOpvD2z5+FZglkepm2O2Xm059tZalIP6ZFyg== by https://journals.lww.com/rapm from Downloaded of Anesthesiologists Downloaded Steven P.Cohen, MD,*† Anuj Bhatia, MBBS, MD,‡ Asokumar Buvanendran, MD,§ Eric S. Schwenk, MD,|| Ajay D. Wasan, MD, MSc,** Robert W. Hurley, MD, PhD,†† Eugene R. Viscusi, MD,|| from https://journals.lww.com/rapm Samer Narouze, MD, PhD,‡‡ Fred N. Davis, MD,§§|||| Elspeth C. Ritchie, MD, MPH,***††† Timothy R. Lubenow, MD,§ and William M. Hooten, MD‡‡‡ relationship, or a minimum or therapeutic dose range; whether oral keta- by Background: Over the past 2 decades, the use of intravenous ketamine BhDMf5ePHKav1zEoum1tQfN4a+kJLhEZgbsIHo4XMi0hCywCX1AWnYQp/IlQrHD3ctdU4DsFBzQV47uVtFPOpvD2z5+FZglkepm2O2Xm059tZalIP6ZFyg== mine or another N-methyl-D-aspartate receptor antagonist was a reasonable infusions as a treatment for chronic pain has increased dramatically, with treatment option as a follow-up to infusions; preinfusion testing require- wide variation in patient selection, dosing, and monitoring. This has ments; settings and personnel necessary to administer and monitor treat- led to a chorus of calls from various sources for the development of ment; the use of preemptive and rescue medications to address adverse consensus guidelines. effects; and what constitutes a positive treatment response. The group Methods: In November 2016, the charge for developing consensus was able to reach consensus on all questions. guidelines was approved by the boards of directors of the American So- Conclusions: Evidence supports the use of ketamine for chronic pain, ciety of Regional Anesthesia and Pain Medicine and, shortly thereafter, but the level of evidence varies by condition and dose range. -

Role of Cytochrome P4502B6 Polymorphisms in Ketamine Metabolism and Clearance
Role of Cytochrome P4502B6 Polymorphisms in Ketamine Metabolism and Clearance Lesley K. Rao, M.D., Alicia M. Flaker, A.S., Christina C. Friedel, B.S., Evan D. Kharasch, M.D., Ph.D. ABSTRACT Background: At therapeutic concentrations, cytochrome P4502B6 (CYP2B6) is the major P450 isoform catalyzing hepatic ketamine N-demethylation to norketamine in vitro. The CYP2B6 gene is highly polymorphic. The most common variant allele, CYP2B6*6, is associated with diminished hepatic CYP2B6 expression and catalytic activity compared with wild-type CYP2B6*1/*1. CYP2B6.6, the protein encoded by the CYP2B6*6 allele, and liver microsomes from CYP2B6*6 carriers had diminished ketamine metabolism in vitro. This investigation tested whether humans with the CYP2B6*6 allele would have Downloaded from http://pubs.asahq.org/anesthesiology/article-pdf/125/6/1103/487909/20161200_0-00014.pdf by guest on 27 September 2021 decreased clinical ketamine metabolism and clearance. Methods: Thirty volunteers with CYP2B6*1/*1, *1/*6, or *6/*6 genotypes (n = 10 each) received a subsedating dose of oral ketamine. Plasma and urine concentrations of ketamine and the major CYP2B6-dependent metabolites were determined by mass spectrometry. Subjects’ self-assessment of ketamine effects were also recorded. The primary outcome was ketamine N-demethylation, measured as the plasma norketamine/ketamine area under the curve ratio. Secondary outcomes included plasma ketamine enantiomer and metabolite area under the plasma concentration–time curve, maximum concentrations, apparent oral clearance, and metabolite formation clearances. Results: There was no significant difference between CYP2B6 genotypes in ketamine metabolism or any of the secondary outcome measures. Subjective self-assessment did reveal some differences in energy and level of awareness among subjects. -

Formulary Advisory Council Meeting Agenda for October 29, 2020
OKLAHOMA BOARD OF NURSING 2915 North Classen Boulevard, Suite 524 Oklahoma City, OK 73106 (405) 962-1800 Formulary Advisory Council AGENDA Thursday, October 29, 2020 2:30 p.m. This virtual Board meeting is being held consistent with the amendments to the Open Meeting Act, 25 O.S. 2011, § 301 et seq, signed into law by Governor Stitt on Wednesday, March 18, 2020. See SB661, 2020 O.S.L. 3, § 3 Website: www.nursing.ok.gov Link to access meeting: https://obn.webex.com/obn/onstage/g.php?MTID=e97fa9d972fec5d402697141d3cab15f1 Event Number: 146 789 6240 Password: W3Lcome2U! Dial US: +1-415-655-0001 to join by audio Access code: 146 789 6240 Link to access meeting materials: http://nursing.ok.gov/facag2020.pdf. The Notice of this meeting was filed with the Secretary of State’s Office on November 27, 2019, and was amended on July 22, 2020, and October 13, 2020. Notice/final agenda was posted on October 15, 2020, at 3:30 PM, on the Cameron Building front entrance at 2915 N. Classen Blvd., Oklahoma City, at the Board office Suite 524, and on the Oklahoma Board of Nursing web site. The Formulary Advisory Council members may discuss, vote to approve, vote to disapprove, vote to table, change the sequence of any agenda item, or vote to strike or not discuss any agenda item. The following council members are participating remotely via the Cisco Webex Events electronic platform: Leanna Harkess, APRN-CNP, CNM Tracy Langley, APRN-CNP Kathy O’Dell, DNP, RN Robin Kimball-Potter, APRN-CNS Jay Kinnard, DPh Denton Chancey, DPh JJ Peek, DPh Kacee Blackwell, DPh Dr.