Resting Membrane Potential (Diffusion Potential, Nernst Potential)
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Oligodendrocytes in Development, Myelin Generation and Beyond
cells Review Oligodendrocytes in Development, Myelin Generation and Beyond Sarah Kuhn y, Laura Gritti y, Daniel Crooks and Yvonne Dombrowski * Wellcome-Wolfson Institute for Experimental Medicine, Queen’s University Belfast, Belfast BT9 7BL, UK; [email protected] (S.K.); [email protected] (L.G.); [email protected] (D.C.) * Correspondence: [email protected]; Tel.: +0044-28-9097-6127 These authors contributed equally. y Received: 15 October 2019; Accepted: 7 November 2019; Published: 12 November 2019 Abstract: Oligodendrocytes are the myelinating cells of the central nervous system (CNS) that are generated from oligodendrocyte progenitor cells (OPC). OPC are distributed throughout the CNS and represent a pool of migratory and proliferative adult progenitor cells that can differentiate into oligodendrocytes. The central function of oligodendrocytes is to generate myelin, which is an extended membrane from the cell that wraps tightly around axons. Due to this energy consuming process and the associated high metabolic turnover oligodendrocytes are vulnerable to cytotoxic and excitotoxic factors. Oligodendrocyte pathology is therefore evident in a range of disorders including multiple sclerosis, schizophrenia and Alzheimer’s disease. Deceased oligodendrocytes can be replenished from the adult OPC pool and lost myelin can be regenerated during remyelination, which can prevent axonal degeneration and can restore function. Cell population studies have recently identified novel immunomodulatory functions of oligodendrocytes, the implications of which, e.g., for diseases with primary oligodendrocyte pathology, are not yet clear. Here, we review the journey of oligodendrocytes from the embryonic stage to their role in homeostasis and their fate in disease. We will also discuss the most common models used to study oligodendrocytes and describe newly discovered functions of oligodendrocytes. -

Clinical Neurophysiology Board Review Q&A
Clinical Neurophysiology Board Review Board Clinical Neurophysiology Clinical Neurophysiology Board Review Q&A Clinical Puneet K. Gupta, MD, MSE • Pradeep N. Modur, MD, MS • Srikanth Muppidi, MD his high-yield, illustrated clinical neurophysiology board review is a comprehen- Neurophysiology sive resource for assessing and refining the knowledge tested on multiple board Texaminations. Written by authors who are collectively board certified in all of the areas covered, the book is a valuable study tool for candidates preparing for certifica- tion or recertification in clinical neurophysiology, neuromuscular medicine, epilepsy, Board Review sleep medicine, and neurology. Using structured question formats typically encountered on boards, this comprehensive review allows users to assess their knowledge in a wide range of topics, provides rationales for correct answers, and explains why the other choices are incorrect. A unique “Pearls” section at the end of the book allows for quick review of the most important concepts prior to exam day. Clinical Neurophysiology Board Review Q&A contains 801 questions with answers and detailed explanations. The book is divided into eight chapters covering anatomy Q and physiology, electronics and instrumentation, nerve conduction studies and EMG, & EEG, evoked potentials and intraoperative monitoring, sleep studies, ethics and safety, and advanced topics including QEEG, MEG, TES, autonomic testing, and more. A Liberal use of image-based questions illustrating the full spectrum of neurophysiologic & tests and findings build interpretive skills. Questions are randomized and include Q A both case-related questions in series and stand-alone items to familiarize candidates Gu with the question types and formats they will find on the exam. -

NF-Jb Signalling Requirement for Brain Myelin Formation Is Shown by Genotype/MRI Phenotype Correlations in Patients with Xq28 Duplications
European Journal of Human Genetics (2013) 21, 195–199 & 2013 Macmillan Publishers Limited All rights reserved 1018-4813/13 www.nature.com/ejhg ARTICLE NF-jB signalling requirement for brain myelin formation is shown by genotype/MRI phenotype correlations in patients with Xq28 duplications Orianne Philippe1, Marle`ne Rio1, Vale´rie Malan1, Hilde Van Esch2, Genevie`ve Baujat1, Nadia Bahi-Buisson3, Vassili Valayannopoulos4, Roseline Gesny1, Jean-Paul Bonnefont1, Arnold Munnich1,GuyFroyen5, Jeanne Amiel1, Nathalie Boddaert1,3 and Laurence Colleaux*,1 One of the key signals regulating peripheral myelin formation by Schwann cell is the activation of the transcription factor NF-jB. Yet, whether NF-jB exerts similar functions in central myelin formation by oligodendrocytes remains largely unknown. We previously reported white matter abnormalities with unusual discordance between T2 and FLAIR sequences in a patient with intellectual disability and defective NF-jB signalling. These observations prompted us to hypothesise that NF-jB signalling may have a role in the axon myelination process of central neurons. We report here on five male patients with Xq28 duplications encompassing MECP2, three of which presented white matter anomalies on brain MRI. Array-CGH and FISH analyses demonstrated that brain abnormalities correlate with additional copies of the IKBKG, a gene encoding a key regulator of NF-jB activation. Quantitative RT-PCR experiments and jB-responsive reporter gene assays provide evidence that IKBKG overexpression causes impaired NF-jB signalling in skin fibroblasts derived from patients with white matter anomalies. These data further support the role of NF-jB signalling in astroglial cells for normal myelin formation of the central nervous system. -

Integrating Brain-Based Psychoeducation Into Clinical Practice Raissa Miller Boise State University
Boise State University ScholarWorks Counselor Education Faculty Publications and Department of Counselor Education Presentations 4-1-2016 Neuroeducation: Integrating Brain-Based Psychoeducation into Clinical Practice Raissa Miller Boise State University This document was originally published in Journal of Mental Health Counseling by the American Mental Health Counselors Association. Copyright restrictions may apply. doi: 10.17744/mehc.38.2.02 Volume 38/Number 2/April 2016/Pages 103-1 IS/doi: 10. l7744/mehc.38.2.02 PRACTICE Neuroeducation: Integrating Brain- Based Psychoeducation into Clinical Practice Raissa M iller Boise State University Understanding and integrating neuroscience research into clinical practice represents a rapidly growing area in mental health. An expanding body of neuroscience literature increasingly informs clinical practice by validating theory, guiding clinical assessment and conceptualiza tion, directing effective interventions, and facilitating cross-disciplinary communication. Little attention, however, has been given to the use of neuroeducation with clients. In this article, the author provides mental health counselors with a definition of neuroeducation and a rationale for incorporating neuroeducation into clinical practice. The author identifies common neuro education topics and offers activity suggestions to illustrate their use in counseling. Finally, the author offers best practices for implementing neuroeducation, including attention to counselor competence, client readiness, and neuroscience of learning -

Supplementation with Complex Milk Lipids During Brain Development Promotes Neuroplasticity Without Altering Myelination Or Vascular Density
food & nutrition æ research ORIGINAL ARTICLE Supplementation with complex milk lipids during brain development promotes neuroplasticity without altering myelination or vascular density Rosamond B. Guillermo1,2, Panzao Yang1,2, Mark H. Vickers1, Paul McJarrow3 and Jian Guan1,2* 1Liggins Institute, The University of Auckland, Auckland, New Zealand; 2Centre for Brain Research, Faculty of Medical and Health Sciences, The University of Auckland, Auckland, New Zealand; 3Fonterra Research and Development Centre, Palmerston North, New Zealand Abstract Background: Supplementation with complex milk lipids (CML) during postnatal brain development has been shown to improve spatial reference learning in rats. Objective: The current study examined histo-biological changes in the brain following CML supplementation and their relationship to the observed improvements in memory. Design: The study used the brain tissues from the rats (male Wistar, 80 days of age) after supplementing with either CML or vehicle during postnatal day 10Á80. Immunohistochemical staining of synaptophysin, glutamate receptor-1, myelin basic protein, isolectin B-4, and glial fibrillary acidic protein was performed. The average area and the density of the staining and the numbers of astrocytes and capillaries were assessed and analysed. Results: Compared with control rats, CML supplementation increased the average area of synaptophysin staining and the number of GFAP astrocytes in the CA3 sub-region of the hippocampus (pB0.01), but not in the CA4 sub-region. The supplementation also led to an increase in dopamine output in the striatum that was related to nigral dopamine expression (pB0.05), but did not alter glutamate receptors, myelination or vascular density. Conclusion: CML supplementation may enhance neuroplasticity in the CA3 sub-regions of the hippocampus. -

Iron Deficiency Alters Auditory Recognition Memory in Newborn
0031-3998/04/5506-1034 PEDIATRIC RESEARCH Vol. 55, No. 6, 2004 Copyright © 2004 International Pediatric Research Foundation, Inc. Printed in U.S.A. Iron Deficiency Alters Auditory Recognition Memory in Newborn Infants of Diabetic Mothers ASHAJYOTHI M. SIDDAPPA, MICHAEL K. GEORGIEFF, SANDI WEWERKA, CATHY WORWA, CHARLES A. NELSON, AND RAYE-ANN DEREGNIER Division of Neonatology, Department of Pediatrics [A.M.S., M.K.G., C.A.N.], Institute of Child Development [M.K.G., S.W., C.A.N.], and Center for Neurobehavioral Development [M.K.G., S.W., C.A.N.], University of Minnesota, Minneapolis, MN 55455, U.S.A.; Division of Neonatology [C.W.], Children’s Hospital-St. Paul, St. Paul, MN 55102, U.S.A.; and Division of Neonatology, Department of Pediatrics [R.-A.d.R.], Northwestern University Feinberg School of Medicine & Children’s Memorial Hospital, Chicago, IL 60611, U.S.A. ABSTRACT Infants of diabetic mothers (IDMs) are at risk for perinatal voices compared with the mothers’ voices, whereas the BID brain iron deficiency that may target the developing hippocam- group did not. Higher cord ferritin concentrations were correlated pus. The objective of this study was to evaluate hippocampally with larger negative slow waves at the right temporal (T4) based recognition memory and infant development in IDMs with electrode site. At1yofage, motor development was slower in suspected brain iron deficiency (BID; cord ferritin Յ34 g/L) the BID group than in the BIS group. IDMs suspected to have compared with IDMs with sufficient brain iron stores (BIS; cord BID demonstrated impaired neonatal auditory recognition mem- ferritin Ͼ34 g/L) using event-related potentials (ERPs). -

The Roles of Lysosomal Exocytosis in Regulated Myelination
Shen YT, Yuan Y, Su WF, Gu Y, Chen G. J Neurol Neuromed (2016) 1(5): 4-8 Neuromedicine www.jneurology.com www.jneurology.com Journal of Neurology & Neuromedicine Mini Review Open Access The Roles of Lysosomal Exocytosis in Regulated Myelination Yun-Tian Shen1, Ying Yuan1,2, Wen-Feng Su1, Yun Gu1, Gang Chen1 1Jiangsu Key Laboratory of Neuroregeneration, Co-innovation Center of Neuroregeneration, Nantong University, Nantong, China 2Affiliated Hospital of Nantong University, Nantong, China ABSTRACT Article Info Article Notes The myelin sheath wraps axons is an intricate process required for Received: June 02, 2016 rapid conduction of nerve impulses, which is formed by two kinds of glial Accepted: July 21, 2016 cells, oligodendrocytes in the central nervous system and Schwann cells in the peripheral nervous system. Myelin biogenesis is a complex and finely *Correspondence: regulated process and accumulating evidence suggests that myelin protein Dr. Gang Chen Jiangsu Key Laboratory of Neuroregeneration Co-innovation synthesis, storage and transportation are key elements of myelination, Center of Neuroregeneration, Nantong University, Nantong, however the mechanisms of regulating myelin protein trafficking are still not China. 226001, Tel: 86-513-85051805, very clear. Recently, the evidences of lysosomal exocytosis in oligodendrocytes Email: [email protected] and Schwann cells are involved in regulated myelination have emerged. In this paper, we briefly summarize how the major myelin-resident protein, as © 2016 Chen G. This article is distributed under the terms of the proteolipid protein in the central nervous system and P0 in the peripheral Creative Commons Attribution 4.0 International License nervous system, transport from lysosome to cell surface to form myelin sheath and focus on the possible mechanisms involved in these processes. -

A Light and Electron Microscope Study of Long
A LIGHT AND ELECTRON MICROSCOPE STUDY OF LONG-TERM ORGANIZED CULTURES OF RAT DORSAL ROOT GANGLIA MARY BARTLETT BUNGE, RICHARD P. BUNGE, EDITH R. PETERSON, and MARGARET R. MURRAY From the Departments of Anatomy and Surgery, Columbia University College of Physicians and Downloaded from http://rupress.org/jcb/article-pdf/32/2/439/1263268/439.pdf by guest on 01 October 2021 Surgeons, New York ABSTRACT Dorsal root ganglia from fetal rats were explanted on collagen-coated coverslips and carried in Maximow double-coverslip assemblies for periods up to 3 months. These cultured ganglia were studied in the living state, in stained whole mounts, and in sections after OsO4 fixation and Epon embedment. From the central cluster of nerve cell bodies, neurites emerge to form a rich network of fascicles which often reach the edge of the carrying coverslip. The neurons resemble their in vivo counterparts in nuclear and cytoplasmic content and organization; e.g., they appear as "light" or "dark" cells, depending on the amount of cytoplasmic neuro- filaments. Satellite cells form a complete investment around the neuronal soma and are themselves everywhere covered by basement membrane. The neuron-satellite cell boundary is complicated by spinelike processes arising from the neuronal soma. Neuron size, myelin- ated fiber diameter, and internode length in the cultures do not reach the larger of the values known for ganglion and peripheral nerve in situ (30). Unmyelinated and myelinated nerve fibers and associated Schwann cells and endoneurial and perineurial components are orga- nized into typical fascicles. The relationship of the Schwann cell and its single myelinated fiber or numerous unmyelinated fibers and the properties of myelin, such as lamellar spacing, mesaxons, Schmidt-Lanterman clefts, nodes of Ranvier, and protuberances, mimic the in vivo pattern. -
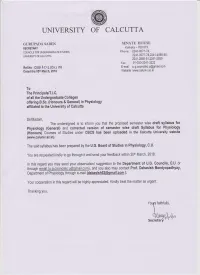
Draft-Physiology-5-2-18.Pdf
University of Calcutta PHYSIOLOGY (GENERAL) SYLLABUS FOR CBCS DRAFT SYLLABUS Core Courses 1. Cellular Basis of Physiology 2. Biophysical Principles, Enzymes and Chemistry of Bio-molecules 3. Blood and Body Fluids 4. Cardiovascular System 5. Respiratory System 6. Digestion and Absorption 7. Metabolism 8. Nutrition and Dietetics 9. Nerve-muscle Physiology 10. Nervous System 11. Special Senses 12. Endocrinology 13. Reproductive Function 14. Excretory Physiology Discipline Specific Electives (DSE)(Any Four) 1. Biostatistics 2. Microbiology 3. Immunology 4. Work Physiology and Ergonomics 5. Exercise and Sports Physiology 6. Human Nutrition and Dietetics 7. Genetics and Molecular Biology 8. Environmental Pollutions and Human Health Hazards 1 Generic Elective (GE)(Any Four) 1. Developmental Biology/ Embryology 2. Instrumentation 3. Environmental Pollution and Human Health 4. Biotechnology 5. Haematology 6. Community and Public Health Ability Enhancement Course (AEC) (Compulsory) 1. Environmental Science 2. English/MIL Communication Skill Enhancement Course (SEC) (Any two) 1. Detection of Food Additives /Adulterants 2. Histopathological Techniques 3. Clinical Biochemistry 4. Hematological Techniques 5. Pathological Microbiology/Bio-Medical Technology 6. Diet Survey and formulation of Diet Chart 2 Outline of Courses and Credits in Each Semester Semester I (A) Core Courses (CC).Theoretical (T) CC1T. Cellular Basis of Physiology Structure and functions of plasma membrane, nucleus and different cell organelles – Endoplasmic reticulum, Golgi bodies,Mitochondria, Lysosome and Peroxisome. Structure, function and classification of Epithelial, Connective, Muscular and Nervous tissues. (4) CC2T. Biophysical Principles, Enzymes and Chemistry of Bio-molecules Physiological importance of the following physical processes: Diffusion , Osmosis and Surface tension. pH and Buffers – Significance in human body and maintenance of pH in the blood. -

Myelin Plasticity and Repair: Neuro-Glial Choir Sets the Tuning Remi Ronzano, Melina Thétiot, Catherine Lubetzki, Anne Desmazières
Myelin Plasticity and Repair: Neuro-Glial Choir Sets the Tuning Remi Ronzano, Melina Thétiot, Catherine Lubetzki, Anne Desmazières To cite this version: Remi Ronzano, Melina Thétiot, Catherine Lubetzki, Anne Desmazières. Myelin Plasticity and Repair: Neuro-Glial Choir Sets the Tuning. Frontiers in Cellular Neuroscience, Frontiers, 2020, 14, pp.42. 10.3389/fncel.2020.00042. hal-02518265 HAL Id: hal-02518265 https://hal.sorbonne-universite.fr/hal-02518265 Submitted on 25 Mar 2020 HAL is a multi-disciplinary open access L’archive ouverte pluridisciplinaire HAL, est archive for the deposit and dissemination of sci- destinée au dépôt et à la diffusion de documents entific research documents, whether they are pub- scientifiques de niveau recherche, publiés ou non, lished or not. The documents may come from émanant des établissements d’enseignement et de teaching and research institutions in France or recherche français ou étrangers, des laboratoires abroad, or from public or private research centers. publics ou privés. MINI REVIEW published: 28 February 2020 doi: 10.3389/fncel.2020.00042 Myelin Plasticity and Repair: Neuro-Glial Choir Sets the Tuning Remi Ronzano 1, Melina Thetiot 1,2, Catherine Lubetzki 1,3 and Anne Desmazieres 1* 1Institut du Cerveau et de la Moelle épinière, Sorbonne Universités UPMC Université Paris 06, CNRS UMR7225-Inserm U1127, Paris, France, 2Unit Zebrafish Neurogenetics, Department of Developmental & Stem Cell Biology, Institut Pasteur, CNRS, Paris, France, 3Assistance Publique-Hôpitaux de Paris, Hôpital Pitié-Salpêtrière, Paris, France The plasticity of the central nervous system (CNS) in response to neuronal activity has been suggested as early as 1894 by Cajal(1894). CNS plasticity has first been studied with a focus on neuronal structures. -

Maturation of the Adolescent Brain
Neuropsychiatric Disease and Treatment Dovepress open access to scientific and medical research Open Access Full Text Article REVIEW Maturation of the adolescent brain Mariam Arain Abstract: Adolescence is the developmental epoch during which children become adults – Maliha Haque intellectually, physically, hormonally, and socially. Adolescence is a tumultuous time, full of Lina Johal changes and transformations. The pubertal transition to adulthood involves both gonadal and Puja Mathur behavioral maturation. Magnetic resonance imaging studies have discovered that myelinogenesis, Wynand Nel required for proper insulation and efficient neurocybernetics, continues from childhood and Afsha Rais the brain’s region-specific neurocircuitry remains structurally and functionally vulnerable to impulsive sex, food, and sleep habits. The maturation of the adolescent brain is also influenced Ranbir Sandhu by heredity, environment, and sex hormones (estrogen, progesterone, and testosterone), which Sushil Sharma play a crucial role in myelination. Furthermore, glutamatergic neurotransmission predominates, For personal use only. Saint James School of Medicine, whereas gamma-aminobutyric acid neurotransmission remains under construction, and this might Kralendijk, Bonaire, The Netherlands be responsible for immature and impulsive behavior and neurobehavioral excitement during adolescent life. The adolescent population is highly vulnerable to driving under the influence of alcohol and social maladjustments due to an immature limbic system and prefrontal -

RECOVERY of MYELINATION in RAT OPTIC NERVE AFTER DEVELOPMENTAL RETARDATION by Cortisoll
0270.6474/82/0209-1292$02.00/O The Journal of Neuroscience Copyright 0 Society for Neuroscience Vol. 2, No. 9, pp. 1292-1298 Printed in U.S.A. September 1982 RECOVERY OF MYELINATION IN RAT OPTIC NERVE AFTER DEVELOPMENTAL RETARDATION BY CORTISOLl MARTHA C. BOHN2 AND VICTOR L. FRIEDRICH, JR. Laboratory of Neuromorphology, Department of Biobehavioral Sciences, University of Connecticut, Storrs, Connecticut 06268 Received October 19,1981; Revised March 15,1982; Accepted April 20, 1982 Abstract Oligodendrocyte formation and myelination in the optic nerve of rats treated with cortisol on postnatal days 7 to 18 were investigated at 21 and 60 days by autoradiographic and morphometric methods. At 21 days, the amount of myelin in the optic nerve of treated rats was reduced by 42%. This reduction was accompanied by a 39% decrease in the number of myelinated axons. In addition, the myelin/axon area ratio was reduced 22% for those axons which were myelinated. At 60 days, the amount of myelin, the number of axons myelinated, the average axonal size, and the average amount of myelin per axon had completely recovered to normal values. Tritiated thymidine-labeling experiments showed that the genesis of oligodendrocytes was enhanced following the cessation of treatment. Since the number of oligodendrocytes in the optic nerve of treated rats was normal at 60 days, it is suggested that the retarding effect of cortisol on myelination in the optic nerve may be mediated, at least in part, by inhibited formation of oligodendrocytes during treatment. Treatment