A12 March PCCC Papers 21 07 2020
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
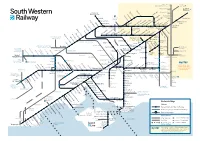
Download Network
Milton Keynes, London Birmingham and the North Victoria Watford Junction London Brentford Waterloo Syon Lane Windsor & Shepherd’s Bush Eton Riverside Isleworth Hounslow Kew Bridge Kensington (Olympia) Datchet Heathrow Chiswick Vauxhall Airport Virginia Water Sunnymeads Egham Barnes Bridge Queenstown Wraysbury Road Longcross Sunningdale Whitton TwickenhamSt. MargaretsRichmondNorth Sheen BarnesPutneyWandsworthTown Clapham Junction Staines Ashford Feltham Mortlake Wimbledon Martins Heron Strawberry Earlsfield Ascot Hill Croydon Tramlink Raynes Park Bracknell Winnersh Triangle Wokingham SheppertonUpper HallifordSunbury Kempton HamptonPark Fulwell Teddington Hampton KingstonWick Norbiton New Oxford, Birmingham Winnersh and the North Hampton Court Malden Thames Ditton Berrylands Chertsey Surbiton Malden Motspur Reading to Gatwick Airport Chessington Earley Bagshot Esher TolworthManor Park Hersham Crowthorne Addlestone Walton-on- Bath, Bristol, South Wales Reading Thames North and the West Country Camberley Hinchley Worcester Beckenham Oldfield Park Wood Park Junction South Wales, Keynsham Trowbridge Byfleet & Bradford- Westbury Brookwood Birmingham Bath Spaon-Avon Newbury Sandhurst New Haw Weybridge Stoneleigh and the North Reading West Frimley Elmers End Claygate Farnborough Chessington Ewell West Byfleet South New Bristol Mortimer Blackwater West Woking West East Addington Temple Meads Bramley (Main) Oxshott Croydon Croydon Frome Epsom Taunton, Farnborough North Exeter and the Warminster Worplesdon West Country Bristol Airport Bruton Templecombe -

Street Name Tree Species/Job Instructions Location Ward ALBURY AVENUE Carpinius Betulus Fastigiata Plant in Grass Verge Outside
Street Name Tree Species/Job Instructions Location Ward Carpinius betulus fastigiata plant Isleworth and ALBURY AVENUE in grass verge Outside 3-5 Brentford Area Carpinus bet.Fastigiata(clear stem) plant in excisting tree pit, Isleworth and ALBURY AVENUE grub out dead sampling. Os 12-14 Brentford Area Plant Sorbus thur. Fastigiata opposite 10 and install new tree ALKERDEN ROAD pit Os 04/06 Chiswick Area Plant Sorbus thur. Fastigiata and ALKERDEN ROAD install new tree pit Os 4-6 Chiswick Area Plant a Sorbus thur. Fastigiata opposite 10 and install new tree ALKERDEN ROAD pit Os 10 Chiswick Area Please plant new Prunus maackii on excisting grass O/S 16 on the O/S 16 on the green plant new Heston and ALMORAH ROAD green Prunus maackii Cranford Area Please plant new Prunus maackii O/S 17 plant new Prunus Heston and ALMORAH ROAD tree on excisting grass O/S 17 maackii tree on excisting grass Cranford Area O/S 21 please plant new O/S 21 Please plant new Prunus Prunus maackii tree on the Heston and ALMORAH ROAD maackii tree on the green grass on the green Cranford Area Please plant new Prunus maackii tree O/S 20-21 on the green on O/S 20-21Please plant new Heston and ALMORAH ROAD excisting grass Prunus maackii tree on grass Cranford Area Please plant new Prunus maackii on excisting grass O/S 16 on the O/S 16 on the green plant new Heston and ALMORAH ROAD green Prunus maackii Cranford Area Transplant Prunus maackii centrally in excisting grass verge O/S 17-21. -

THE CHARACTER of the LANDSCAPE 2.39 the Thames
THE CHARACTER OF THE LANDSCAPE 2.39 The Thames enters the Greater London Area at Hampton. From Hampton to Erith, the river fl ows through the metropolis; an urban area even though much of the riverside is verdant open space, particularly in the fi rst stretch between Hampton and Kew. 2.40 The character of the river is wonderfully varied and this chapter concentrates on understanding how that variety works. We have deliberately avoided detailed uniform design guidelines, such as standard building setbacks from the water’s edge. At this level, such guidelines would tend to stifl e rather than encourage the variety in character. Instead we have tried to highlight the main factors which determine the landscape character and propose recommendations to conserve and enhance it. 2.41 Landscape Character Guidance LC 1: New development and new initiatives within the Strategy area should be judged against the paramount aim of conserving and enhancing the unique character of the Thames Landscape as defi ned in the Strategy. The River 2.42 Although, being a physical boundary, the river is often on the periphery of county and local authority jurisdictions, it is essentially the centre of the landscape. The Thames has carved the terraces and banks that line its course, the valley sides drain down to its edges and the water acts as the main visual and physical focus. It is a dynamic force, constantly changing with the tide and refl ecting the wind and the weather on its surface. 2.43 Downstream of the great expanse of water at the confl uence with the Wey, the Thames fl ows from west to east – the Desborough Cut by-passing the large meander near Shepperton. -

1.0 Site 1.1 Liddle Keen & Co
References – L/676/5/436 & P/2003/3749 Isleworth and Brentford Area Committee 04 March 2004 Case Officer – [email protected] - (020 8583 4943) 1.0 SITE 1.1 LIDDLE KEEN & CO, RAILSHEAD ROAD, ISLEWORTH (London Borough of Richmond, affecting Isleworth Ward) 2.0 PROPOSAL 2.1 Demolition of existing buildings, new development comprising of 18 residential units (9 private dwellings and 9 affordable flats) 2.2 The application has been called into area committee by Councillor Hibbs. The reason given is that this is an environmentally sensitive Thames Riverside area, which should be protected. 3.0 SITE DESCRIPTION: 3.1 The site is located within the London Borough of Richmond upon Thames, and is on the south side of the River Crane at its confluence with the Thames. The Richmond Road traffic bridge passes over the Crane on the western boundary of the site. Land on the northern side of the river is within the London Borough of Hounslow, and comprises the Nazareth House convent and care home complex, and also has the Isleworth Sea Scouts base. This site is within the Isleworth Riverside Conservation Area. A boat shed and dock area is directly opposite the application site. 3.2 The application site is currently used as the headquarters of a building company, and contains offices and storage areas. 4.0 HISTORY: 4.1 L/676/5/429 – Demolition of existing buildings and erection of a new building comprising 18 residential units (9 private dwellings and 9 affordable flats). The Council raised no objection to this application. -

Appointment of Election Agents
Greater London Authority Election of the Assembly Member for the SOUTH WEST Constituency APPOINTMENT OF ELECTION AGENTS NOTICE IS HEREBY GIVEN that the following candidates have appointed or are deemed to have appointed the person named as election agents for the election of the London Assembly Member for the SOUTH WEST Constituency on Thursday, 5 May 2016. NAME AND ADDRESS OF NAME AND ADDRESS OF AGENT ADDRESS OF OFFICE TO WHICH CANDIDATE CLAIMS AND OTHER DOCUMENTS MAY BE SENT IF DIFFERENT FROM ADDRESS OF AGENT Tony Arbour David Richard Jones 372 Upper Richmond Road West, 3 Holmesdale Road, Teddington, 16 Eaton Drive, Kingston Hill, East Sheen, London, SW14 7JU Middlesex, TW11 9LJ Kingston upon Thames, KT2 7QT Adam John Lewis Buick Oliver Rupert Bond 23 Ham Street, Richmond, TW10 Flat 9, 84 London Road, Kingston, 7HR KT2 6PX Alexander Alan Craig Peter Staveley Flat 1, 156 Pentonville Road, 36 Studley Road, London, E7 9LX 247 Davidson Road, Croydon, CR0 London, N1 9JL 6DQ Andree Michelle Frieze Thomas Dunning Beaton 139 Latchmere Lane, Kingston upon 42 Church Street, Isleworth, TW7 Thames, KT2 5NX 6BG Rosina Jane Robson Roisin Miller 21 Berrylands Road, Surbiton, KT5 26 Adelaide Road, Richmond, TW9 6b Arcade Parade, Elm Road, 8QX 1XW Chessington, KT9 1AB Martin James Whelton Alastair Michael Craft Brentford & Isleworth Labour Party, 4 Crossways Road, Mitcham, CR4 1 Arta House, Devonport Street, 367 Chiswick High Road, London, 1DQ London, E1 0EF W4 4AG Dated this Friday, 01 April 2016 Mary Harpley, Constituency Returning Officer London Borough of Hounslow Civic Centre Lampton Road Hounslow TW3 4DN Published and printed by Mary Harpley, Constituency Returning Officer, London Borough of Hounslow, Civic Centre, Lampton Road, Hounslow, TW3 4DN . -
Proposed Additions to the Local List
Proposed Additions to the Local List January 2019 Table of Contents Page number Area Chiswick 3 Brentford 26 Isleworth 36 Hounslow 52 Heston & Cranford 65 Feltham and Bedfont 73 2 Chiswick 3 Image Asset Details Description Address: Homefield Lodge, Lodge which acted as the keeper’s cottage for Chiswick Lane South the Homefield Recreation Ground. It likely dates from the late 19th – early 20th century. Significance: Architectural, The house is made of brick with bargeboards Historical and roof ridge detailing. Reference Number: CH28 Address: Chiswick Baptist Chiswick Baptist Church is a good example of Church, Annandale Road Nonconformist architecture of the late 19th century. The church is ‘a tightly planned, Significance: Architectural, irregular composition’ (Pevsner). It is a red Historical, Social brick three-storey building in gothic style with a pitched slate roof. Chiswick Baptist Church Reference Number: CH29 was designed by John Wills of Derby (1846 - 1906), the foremost architect of non- conformist church buildings of his era. Address: Hogarth Statue, The statue is a one-and-a-quarter-times-life- Chiswick High Road size bronze statue. It shows Hogarth wearing his painting smock and cap and holding his Significance: Architectural, palette and brushes. His pug sits by his side, Historical, Social reminiscent of Hogarth’s self portrait now in the Tate, sculpted by Jim Mathieson. Reference Number: CH30 Hogarth’s main home was in Leicester Square but in 1749 he bought the house in Chiswick that is now known as Hogarth's House and he spent time there for the rest of his life. Hogarth is buried in the family tomb in St Nicholas’ Churchyard, Chiswick. -

Residential Development Opportunity on Behalf of London Borough of Hounslow
Residential Development Opportunity On behalf of London Borough of Hounslow Land adjacent to 20 Byfield Road, Isleworth, TW7 7AF • Plot of land with excellent development potential • GLA’s Small Sites Small Builders Programme • Long leasehold for sale via informal tender • Unconditional and subject to planning offers invited Introduction and Background Small Sites, Small Builders The Greater London Authority’s Small Sites, Small Builders programme aims to bring forward small publicly-owned plots of land for residential development by small-sized housebuilders, housing associations, community-led housing groups and other small-scale developing organisations. As part of this programme, the London Borough of Hounslow is releasing a number of small sites to the market, specifically for sale to Registered Providers. Description and Location The site is located on the corner of Byfield Road and Carrick Close in Isleworth, adjacent to 18 and 20 Byfield Road. It is approximately 0.9 miles to the south east of Isleworth Station, which is served by regular South Western Railway trains to London Waterloo, Weybridge and Mortlake. The local bus network is accessible from nearby South Street, Twickenham Road and Richmond Road. The predominant use in the immediate locality is residential. The wider area is mixed use with a number of commercial, religious and educational facilities along Twickenham Road. In total, the site is approximately 0.048 acres (0.0197 ha) in size and comprises a row of six garages and hardstanding. The site is bound by the side wall of a garage to the north. A row of terraced houses facing Carrick Close sit to the east of the site. -

Brentford & Isleworth Locality Patient Community Group Minutes Of
Brentford & Isleworth Locality Patient Community Group Minutes of Meeting held on Tuesday 27th January 1-2pm Committee Room, Brentford Health Centre Present In Attendance Julia Chalmers Watson: GP / Locality Chair Sue Jeffers: HCCG Managing Director Sue Joyce: Patient Clive Chalk: HCCG Lay Member Nigel Edwards: Patient Dilo Lalande: HCCG Engagement & Comms Barbara Stryjak: Patient Manager Sarah Felstead: Patient Danny Rybowski: Patient Barbara Benedek: HCCG PCRG Chair George Foster: Patient Alma Chisholm: Practice Manager Mystica Thiruchelvam: Healthwatch Kusum Joshi: Healthwatch Apologies Not in Attendance Robert Flann: HCCG Patient Engagement Officer Agenda Item Action 1. Welcome, Introductions & Apologies JCW welcomed members to the meeting and apologies were noted. PPG INFO FOR BB introduced herself as the chair of Hounslow’s PCRG and LPPG.pptx explained briefly what this entails. She went on to ask how the group feedback. It was explained that a member of the LPPG will sit on the CCGs public and patient engagement committee. SJ introduced herself and explained that she was attending at least one PPG in each locality to gain feedback on the PMS review CC described his role within the CCG, explaining that he was there as a critical friend of the CCG to ensure that quality, complaints and engagement involvement are rigorous and the work that we do is joined up and always benefits the patient. ACTION – Robert to distribute to the group – PMS presentation, map of localities and diagram of accountabilities, where PPGs sit. Page 1 of 4 2. Personal Medical Services (PMS) Review Sue Jeffers Managing Director for Hounslow CCG and Clive Chalk PMS indicators for Engagement Lay Member for Hounslow CCG presented the PMS patient engagement.pp review (see attached) to the group. -

PADDLING TRAIL River Thames: Putney to Old Isleworth
PADDLING TRAIL River Thames: Putney to Old Isleworth Key Information Start: Putney Slipway, Putney Portages: 0 For more Embankment, Putney, Time: 2-4 hours information scan SW15 1JW Distance: 8 miles the QR code or Finish: Isleworth Draw Dock, OS Map: Explorer 161 https://bit.ly/2Lyh5 Church St, Old Isleworth, London South k1 TW7 6BG & 173 London North This is a busy and tidal part of the River Thames. You must visit boatingonthethames.co.uk to check tide times and safety advice before undertaking this trail. The trail covers the Upper Tideway in south west London, with sweeping aspects of the river. The course of the annual University Boat Race forms part of the trail. 1. We recommend you paddle with the assistance of the tidal flow, departing from Putney in the first 2 hours of the flood tide. Closely timing the tides can allow a return trip. Put in at the public slipway, crossing to the Football Stadium side of the river and turning left, for correct rules of travel. 2. Approaching Hammersmith Bridge the London Wetland Centre is behind the tree line on the opposite bank. Beware of the tide pushing you into Dove Pier after the b ridge. 3. Between Hammersmith and Chiswick Ait the river is flanked by elegant houses. At Chiswick Ait an option is to take the inside channel; usually passable after an hour or so of a flood tide. 4. Chiswick Pier signals a crossing point for a change in navigation rules. Keep the green marker buoys on your right on this sweeping bend of the river to Chiswick Bridge. -

Travel to British Standards Institution
L D A V E C R S D E A T E S R A N Based on Bartholomews mapping. ReproducedB by permissionB Di L W S R E NEWTON AV U R st A Y O of HarperCollins Publishers Ltd., Bishopbriggs, Glasgow.Y 2012 r E A ic 272 D R A D A t R A RO V N C M 272 LD www.bartholomewmaps.com Y E L T HA Route27 until NovBBO 2012 in AN D O N A O C V C By Train e U L N E Digital Cartography by Pindar Creative n w L Getting to BSI mi alk 15 ing N A Acton0- t Route27 from Nov 2012 E V 1 imE Q • The London Overground runs between L e B491 D E ROAD N t e SOUTHFIELD E Ya Town f R U mR B 440 r B E i O o (subject to confirmation) Address: Chiswick Tower, Richmond and Stratford stopping at Travel to E U x L AD mD R o B L A R S O RO O r E Y R R G R s SPELDHUR E p EY L ID i ST R 389 Chiswick High Road, London W4 4AL. Gunnersbury. A R R O M NR B E t AD O p NU N H e A B E LLO C L A SU O T Y British Standards D RG B E T E ERSE 91 N L SOM T N F BEDFORD U N SOUTH H All visitors must enter the building through • The ‘Hounslow Loop’ has stations at E3 G ROAD B44 E B O R PARK the main entrance on Chiswick High Road Kew Bridge, Richmond, Weybridge, NE O Institution A ACTON L D L S A A D A R N E O E O 272 fields E U D EL A E V R E T U 94 and report to Reception on arrival. -

West London Orbital Rail Technical Analysis and Conclusions
WEST LONDON ORBITAL RAIL TECHNICAL ANALYSIS AND CONCLUSIONS OCTOBER 2017 WEST LONDON ORBITAL RAIL TECHNICAL ANALYSIS AND CONCLUSIONS West London Alliance Report Project no: 70034419 Date: October 2017 WSP WSP House, 70 Chancery Lane London WC2A 1AF www.wsp.com QUALITY MANAGEMENT ISSUE/REVISION FIRST ISSUE REVISION 1 REVISION 2 FINAL Remarks Draft for comments Final draft Incorporation of client Final comments Date 27 July 2017 1 September 2017 8 September 2017 17 October 2017 Prepared by NL, JM NL, JM, CB, LE CW EOL, NL Checked by CW CW EO’L EOL Authorised by EO’L EO’L EO’L CW Project number 70034419 70034419 70034419 70034419 Report number Draft v1.0 Draft v2.0 Draft v3.0 FINAL File reference 70034419 - Services on Dudding Hill Line\02 WIP\TP Transport planning\03 Document\Technical Report Issued\ ii TABLE OF CONTENTS 1 INTRODUCTION .........................................................................10 1.1 CONTEXT ..................................................................................................... 10 1.2 THIS DOCUMENT ........................................................................................ 11 2 STRATEGIC OPTIONS ..............................................................12 2.1 INTRODUCTION ........................................................................................... 12 2.2 CONSIDERATION OF STRATEGIC OPTIONS ............................................. 12 2.3 FINDINGS OF ASSESSMENT ...................................................................... 12 3 DEMAND ANALYSIS: APPROACH -

ACC/1399 Page 1 Reference Description Dates ISLEWOR
LONDON METROPOLITAN ARCHIVES Page 1 WATNEY COMBE REID AND COMPANY LIMITED {BREWERS} ACC/1399 Reference Description Dates ISLEWORTH BREWERY: PROPERTY RECORDS Deeds and related papers ACC/1399/001 Mortgage (by lease and release), 7-8 July 1726 - 1731 1726. 1. John Atfield of Old Brentford, clockmaker. 2. Richard Clements of Isleworth, gardener. Premises: messuage and tenement with appurts. and close of land (3½a.) in Isleworth. Consideration: £150. Endorsement: receipt, 25 Sept 1731, of (2) for £159. 7s. 6d. received of Mr. William Harvest at direction of (1), in discharge of mortgage, (2) will hold premises in trust until directed to convey to William Harvest. ACC/1399/002 Lease and release. 1731 28 - 29 1. Richard Clements of Isleworth, gardener. Sep 2. John Atfield of Old Brentford, clockmaker. 3. William Harvest of Isleworth, brewer. Premises: as in ACC/1399/001a-b. Consideration: £159. 7s. 6d. LONDON METROPOLITAN ARCHIVES Page 2 WATNEY COMBE REID AND COMPANY LIMITED {BREWERS} ACC/1399 Reference Description Dates ACC/1399/003 Deed to lead uses of common recovery and 1767 covenant to release copyhold. (attested copies) 18-19 Jan [1747/8]. 1. Margaret Harvest of Woking, Surrey, widow of William Harvest of Woking, brewer, deceased. 2. William Harvest of Chiswick, brewer, son and heir of William Harvest. 3. George Harvest of St. Bride, London, distiller, et al. 4. Forbench Bradford of Shere, Surrey, gent., grandson of William Harvest. 5. William Nicholls of Shepperton, gent and Matthew Nicholls of Shepperton, brewer. 6. John Easted of Worplesdon, Surrey, gent. and wife Elizabeth. 7. John Biscoe of Inner Temple, gent.