Analysis of Malaria Epidemiological Characteristics in Tengchong
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Studies on the Relationships of the Curie Surface with Heat Flow And
Wen et al. Earth, Planets and Space (2019) 71:85 https://doi.org/10.1186/s40623-019-1063-1 FULL PAPER Open Access Studies on the relationships of the Curie surface with heat fow and crustal structures in Yunnan Province, China, and its adjacent areas Limin Wen, Guofa Kang, Chunhua Bai and Guoming Gao* Abstract A Curie surface indicates the distribution of the thermal felds underground, providing a clear marker for the thermo- dynamic efect in the crust and mantle. In this paper, based on a geomagnetic feld model (NGDC-720) and aeromag- netic data, we use power spectrum analysis of magnetic anomalies to estimate the Curie surface in Yunnan Province, China, and its adjacent areas. By combining the distribution of the Curie surface with regional heat fow, the geo- thermal gradient, crustal wave velocity ratio anomalies, high-conductivity layer anomalies, and the Moho surface, we reveal the connection between the undulation of the magnetic basement and the crustal structures. The results indi- cate that the uplift and depression of the Curie surface in the research area are distinct. The Curie surface is approxi- mately inversely correlated to the surface heat fow. The Lijiang-Jianchuan-Baoshan-Tengchong and Jianchuan- Chux- iong- Kunming-Yuxi zones are two Curie surface uplift zones, and their crust-mantle heat fows are relatively high. The Curie surface uplift zone along the Lijiang-Xiaojinhe fault and Red River fault is consistent with the heading direction of the fault zone and is partially in agreement with the eastward mass fow of the Tibetan Plateau. The Curie surface uplift zone is consistent with the high wave velocity ratio and high-conductivity layer anomaly region of the crust. -

Project News: a New Green Line December 2020 — Issue #3 FAO / MWR-CN FAO ©
Project News: A New Green Line December 2020 — Issue #3 FAO / MWR-CN FAO © Mainstreaming Biodiversity Conservation Objective and GCP/CPR/057/GFF Practices into China’s Water Resources Management September 2020) GCP/CPR/052/GFF 2020 PSC meeting project delivery, learn from achievements and enhance communications with each other. The knowledge products could be helpful for “Strengthening Supervision” in the The 2020 annual meeting of the Project Steering water sector. They can also be shared at the 15th meeting Committee (PSC) was held in Beijing on September 11. Shi of the Conference of the Parties to the Convention on Qiuchi, Director-General of the International Economic and Biological Diversity, which will be held in Kunming, Yunnan Technical Cooperation and Exchange Center (INTCE), Province in 2021. chaired the meeting. Participants included Li Ge, Executive Deputy Director of the Project Steering Committee and Deputy Director-General of the Department of International Cooperation and Science and Technology under the Ministry of Water Resources (MWR), PSC members and representatives of China GEF Secretariat, Food and Agriculture Organization of the United Nations (FAO), and The Nature Conservancy (TNC). Representatives of Project Management Offices (PMOs) from MWR, Chongqing and Yunnan, as well as project experts attended CN - the meeting. Participants outside Beijing joined the meeting online. FAO/MWR © PMOs of MWR, Yunnan and Chongqing reported project The 2020 annual PSC meeting was held in Beijing on September progress at the meeting. The PSC reviewed and discussed 11, 2020 the 2020 project work plan and budget submitted by the PMO of MWR, the recommended Participatory Theory of A two-year project extension approved Change and indicator targets to be adjusted, as well as the proposal to develop Exit Strategy. -

Report on Domestic Animal Genetic Resources in China
Country Report for the Preparation of the First Report on the State of the World’s Animal Genetic Resources Report on Domestic Animal Genetic Resources in China June 2003 Beijing CONTENTS Executive Summary Biological diversity is the basis for the existence and development of human society and has aroused the increasing great attention of international society. In June 1992, more than 150 countries including China had jointly signed the "Pact of Biological Diversity". Domestic animal genetic resources are an important component of biological diversity, precious resources formed through long-term evolution, and also the closest and most direct part of relation with human beings. Therefore, in order to realize a sustainable, stable and high-efficient animal production, it is of great significance to meet even higher demand for animal and poultry product varieties and quality by human society, strengthen conservation, and effective, rational and sustainable utilization of animal and poultry genetic resources. The "Report on Domestic Animal Genetic Resources in China" (hereinafter referred to as the "Report") was compiled in accordance with the requirements of the "World Status of Animal Genetic Resource " compiled by the FAO. The Ministry of Agriculture" (MOA) has attached great importance to the compilation of the Report, organized nearly 20 experts from administrative, technical extension, research institutes and universities to participate in the compilation team. In 1999, the first meeting of the compilation staff members had been held in the National Animal Husbandry and Veterinary Service, discussed on the compilation outline and division of labor in the Report compilation, and smoothly fulfilled the tasks to each of the compilers. -

The Dragon's Roar: Traveling the Burma Road
DBW-17 EAST ASIA Daniel Wright is an Institute Fellow studying ICWA the people and societies of inland China. LETTERS The Dragon’s Roar — Traveling the Burma Road — Since 1925 the Institute of RUILI, China March 1999 Current World Affairs (the Crane- Rogers Foundation) has provided Mr. Peter Bird Martin long-term fellowships to enable Executive Director outstanding young professionals Institute of Current World Affairs 4 West Wheelock St. to live outside the United States Hanover, New Hampshire 03755 USA and write about international areas and issues. An exempt Dear Peter, operating foundation endowed by the late Charles R. Crane, the Somewhere in China’s far west, high in the Tibetan plateau, five of Asia’s Institute is also supported by great rivers — the Yellow, the Yangtze, the Mekong, the Salween and the contributions from like-minded Irrawaddy — emerge from beneath the earth’s surface. Flowing east, then individuals and foundations. fanning south and north, the waterways cut deep gorges before sprawling wide through lowlands and spilling into distant oceans. TRUSTEES Bryn Barnard These rivers irrigate some of Asia’s most abundant natural resources, the Carole Beaulieu most generously endowed of which are in Myanmar, formerly Burma. Mary Lynne Bird Peter Geithner “Myanmar is Asia’s last great treasure-trove,” a Yangon-based western dip- Thomas Hughes lomat told me during a recent visit to this land of contradiction that shares a 1 Stephen Maly border with southwest China’s Yunnan Province. Peter Bird Martin Judith Mayer Flush with jade, rubies, sapphires, natural gas and three-quarters of the Dorothy S. -
中國貴金屬資源控股有限公司 (Incorporated in the Cayman Islands with Limited Liability) (Stock Code: 1194)
THIS CIRCULAR IS IMPORTANT AND REQUIRES YOUR IMMEDIATE ATTENTION If you are in any doubt as to any aspect of this circular or as to the action to be taken, you should consult your licensed securities dealer, registered institution in securities, bank manager, solicitor, professional accountant or other professional adviser. If you have sold or transferred all your shares in China Precious Metal Resources Holdings Co., Ltd. (the “Company”), you should at once hand this circular to the purchaser or the transferee or to the bank, licensed securities dealer, registered institution in securities or other agent through whom the sale or transfer was effected for transmission to the purchaser or the transferee. Hong Kong Exchanges and Clearing Limited and The Stock Exchange of Hong Kong Limited take no responsibility for the contents of this circular, make no representation as to its accuracy or completeness and expressly disclaim any liability whatsoever for any loss howsoever arising from or in reliance upon the whole or any part of the contents of this circular. This circular appears for information purpose only and does not constitute an invitation or offer to acquire, purchase or subscribe for securities of China Precious Metal Resources Holdings Co., Ltd. CHINA PRECIOUS METAL RESOURCES HOLDINGS CO., LTD. 中國貴金屬資源控股有限公司 (Incorporated in the Cayman Islands with limited liability) (Stock code: 1194) MAJOR ACQUISITION RELATING TO ACQUISITION OF GOLD MINES IN THE PRC Financial Adviser to China Precious Metal Resources Holdings Co., Ltd. A letter from the board of directors of the Company is set out from pages 6 to 36 of this circular. -

11D Yunnan Yuxi Pu-Er Xishuang-Banna Tengchong Ruili
1 Park Road, #03-09 People’s Park Complex, Singapore 059108 Tel: 6438 7478 Fax: 6438 9794 www.newaytravel.com.sg Exclusive of Neway Travel 11D Yunnan Yuxi Pu-Er Xishuang-Banna Tengchong Ruili Colorful Ethnic Experience Tour TOUR CODE: KMG11M 【Colorful Ethnic Experience】: To enter deeply into Dai,Naxi,Bai,Bulang,Wa Peoples Culture,Language, Costumes and ect. 【High Light】:Yuxi,Pu-Er,Xishuang Banna,Cangyuan,Tengchong,Ruili 【Local Flavor】:Steam Chicken+ Guoqiao Rice Noodle,Tengchong Local Style,Dai Flavor 【Shopping】: Yunnan Puer Tea Shop,Jade Shop Tengchong. D1:SIN KMG/YUXI (L/D) Accommodation:Gaodeng Hotel or similar 4Star Assemble at Singapore Changi Airport for our flight to Kunming, capital of Yunnan Province. Upon arrival, transfer to Yuxi. Yuxi Cigarette Company (Hongta Group) has become a famous cigarette making company. Its product brands such as Hongtashan, Ashima and Hongmei have been popular for many years in China. Upon arrival, the area also has beautiful natural sceneries and colorful cultures. Upon arrival, visit Hongta District. Next proceed to Pu-Er. : ( ) : D2 Pu-Er/Xishuang-Banna B/L/D Accommodation King Land Hotel or similar 4Star Pu'er is the birthplace of Pu Er Tea, a very famous international tea brand. Tea culture is an attractive tourist factor of Puer City visit the Pr-Er Tea Exhibition Garden. The garden is built on the Yinpan Mountain,29 km from downtown Puer, Against the background of a vast tea garden, it is made up of Pu'er Tea Museum, Pu'er Tea Making workshop, tea-picking zone, tea appraisal garden and some other facilities to comprehensively show the history of Pu'er Tea, and how to plant and produce as well. -
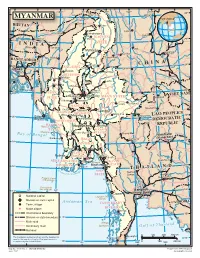
Map of Myanmar
94 96 98 J 100 102 ° ° Indian ° i ° ° 28 n ° Line s Xichang Chinese h a MYANMAR Line J MYANMAR i a n Tinsukia g BHUTAN Putao Lijiang aputra Jorhat Shingbwiyang M hm e ra k Dukou B KACHIN o Guwahati Makaw n 26 26 g ° ° INDIA STATE n Shillong Lumding i w d Dali in Myitkyina h Kunming C Baoshan BANGLADE Imphal Hopin Tengchong SH INA Bhamo C H 24° 24° SAGAING Dhaka Katha Lincang Mawlaik L Namhkam a n DIVISION c Y a uan Gejiu Kalemya n (R Falam g ed I ) Barisal r ( r Lashio M a S e w k a o a Hakha l n Shwebo w d g d e ) Chittagong y e n 22° 22° CHIN Monywa Maymyo Jinghong Sagaing Mandalay VIET NAM STATE SHAN STATE Pongsali Pakokku Myingyan Ta-kaw- Kengtung MANDALAY Muang Xai Chauk Meiktila MAGWAY Taunggyi DIVISION Möng-Pan PEOPLE'S Minbu Magway Houayxay LAO 20° 20° Sittwe (Akyab) Taungdwingyi DEMOCRATIC DIVISION y d EPUBLIC RAKHINE d R Ramree I. a Naypyitaw Loikaw w a KAYAH STATE r r Cheduba I. I Prome (Pye) STATE e Bay Chiang Mai M kong of Bengal Vientiane Sandoway (Viangchan) BAGO Lampang 18 18° ° DIVISION M a e Henzada N Bago a m YANGON P i f n n o aThaton Pathein g DIVISION f b l a u t Pa-an r G a A M Khon Kaen YEYARWARDY YangonBilugyin I. KAYIN ATE 16 16 DIVISION Mawlamyine ST ° ° Pyapon Amherst AND M THAIL o ut dy MON hs o wad Nakhon f the Irra STATE Sawan Nakhon Preparis Island Ratchasima (MYANMAR) Ye Coco Islands 92 (MYANMAR) 94 Bangkok 14° 14° ° ° Dawei (Krung Thep) National capital Launglon Bok Islands Division or state capital Andaman Sea CAMBODIA Town, village TANINTHARYI Major airport DIVISION Mergui International boundary 12° Division or state boundary 12° Main road Mergui n d Secondary road Archipelago G u l f o f T h a i l a Railroad 0 100 200 300 km Chumphon The boundaries and names shown and the designations Kawthuang 10 used on this map do not imply official endorsement or ° acceptance by the United Nations. -

Kahrl Navigating the Border Final
CHINA AND FOREST TRADE IN THE ASIA-PACIFIC REGION: IMPLICATIONS FOR FORESTS AND LIVELIHOODS NAVIGATING THE BORDER: AN ANALYSIS OF THE CHINA- MYANMAR TIMBER TRADE Fredrich Kahrl Horst Weyerhaeuser Su Yufang FO RE ST FO RE ST TR E ND S TR E ND S COLLABORATING INSTITUTIONS Forest Trends (http://www.forest-trends.org): Forest Trends is a non-profit organization that advances sustainable forestry and forestry’s contribution to community livelihoods worldwide. It aims to expand the focus of forestry beyond timber and promotes markets for ecosystem services provided by forests such as watershed protection, biodiversity and carbon storage. Forest Trends analyzes strategic market and policy issues, catalyzes connections between forward-looking producers, communities, and investors and develops new financial tools to help markets work for conservation and people. It was created in 1999 by an international group of leaders from forest industry, environmental NGOs and investment institutions. Center for International Forestry Research (http://www.cifor.cgiar.org): The Center for International Forestry Research (CIFOR), based in Bogor, Indonesia, was established in 1993 as a part of the Consultative Group on International Agricultural Research (CGIAR) in response to global concerns about the social, environmental, and economic consequences of forest loss and degradation. CIFOR research produces knowledge and methods needed to improve the wellbeing of forest-dependent people and to help tropical countries manage their forests wisely for sustained benefits. This research is conducted in more than two dozen countries, in partnership with numerous partners. Since it was founded, CIFOR has also played a central role in influencing global and national forestry policies. -

Yunnan Provincial Highway Bureau
IPP740 REV World Bank-financed Yunnan Highway Assets management Project Public Disclosure Authorized Ethnic Minority Development Plan of the Yunnan Highway Assets Management Project Public Disclosure Authorized Public Disclosure Authorized Yunnan Provincial Highway Bureau July 2014 Public Disclosure Authorized EMDP of the Yunnan Highway Assets management Project Summary of the EMDP A. Introduction 1. According to the Feasibility Study Report and RF, the Project involves neither land acquisition nor house demolition, and involves temporary land occupation only. This report aims to strengthen the development of ethnic minorities in the project area, and includes mitigation and benefit enhancing measures, and funding sources. The project area involves a number of ethnic minorities, including Yi, Hani and Lisu. B. Socioeconomic profile of ethnic minorities 2. Poverty and income: The Project involves 16 cities/prefectures in Yunnan Province. In 2013, there were 6.61 million poor population in Yunnan Province, which accounting for 17.54% of total population. In 2013, the per capita net income of rural residents in Yunnan Province was 6,141 yuan. 3. Gender Heads of households are usually men, reflecting the superior status of men. Both men and women do farm work, where men usually do more physically demanding farm work, such as fertilization, cultivation, pesticide application, watering, harvesting and transport, while women usually do housework or less physically demanding farm work, such as washing clothes, cooking, taking care of old people and children, feeding livestock, and field management. In Lijiang and Dali, Bai and Naxi women also do physically demanding labor, which is related to ethnic customs. Means of production are usually purchased by men, while daily necessities usually by women. -

Three-Dimensional Velocity Structure of Crust and Upper Mantle In
JOURNAL OF GEOPHYSICAL RESEARCH, VOL. 108, NO. B9, 2442, doi:10.1029/2002JB001973, 2003 Three-dimensional velocity structure of crust and upper mantle in southwestern China and its tectonic implications Chun-Yong Wang Institute of Geophysics, China Seismological Bureau, Beijing, China W. Winston Chan Multimax, Inc., Largo, Maryland, USA Walter D. Mooney U.S. Geological Survey, Menlo Park, California, USA Received 13 May 2002; revised 17 March 2003; accepted 29 April 2003; published 25 September 2003. [1] Using P and S arrival times from 4625 local and regional earthquakes recorded at 174 seismic stations and associated geophysical investigations, this paper presents a three- dimensional crustal and upper mantle velocity structure of southwestern China (21°– 34°N, 97°–105°E). Southwestern China lies in the transition zone between the uplifted Tibetan plateau to the west and the Yangtze continental platform to the east. In the upper crust a positive velocity anomaly exists in the Sichuan Basin, whereas a large-scale negative velocity anomaly exists in the western Sichuan Plateau, consistent with the upper crustal structure under the southern Tibetan plateau. The boundary between these two anomaly zones is the Longmen Shan Fault. The negative velocity anomalies at 50-km depth in the Tengchong volcanic area and the Panxi tectonic zone appear to be associated with temperature and composition variations in the upper mantle. The Red River Fault is the boundary between the positive and negative velocity anomalies at 50-km depth. The overall features of the crustal and the upper mantle structures in southwestern China are a low average velocity, large crustal thickness variations, the existence of a high- conductivity layer in the crust or/and upper mantle, and a high heat flow value. -

From Kunming to Mandalay: the New “Burma Road”
AsieAsie VVisionsisions 2525 From Kunming to Mandalay: The New “Burma Road” Developments along the Sino-Myanmar border since 1988 Hélène Le Bail Abel Tournier March 2010 Centre Asie Ifri The Institut français des relations internationales (Ifri) is a research center and a forum for debate on major international political and economic issues. Headed by Thierry de Montbrial since its founding in 1979, Ifri is a non-governmental and a non-profit organization. As an independent think tank, Ifri sets its own research agenda, publishing its findings regularly for a global audience. Using an interdisciplinary approach, Ifri brings together political and economic decision-makers, researchers and internationally renowned experts to animate its debate and research activities. With offices in Paris and Brussels, Ifri stands out as one of the rare French think tanks to have positioned itself at the very heart of European debate. The opinions expressed in this text are the responsibility of the authors alone. ISBN : 978-2-86592-675-6 © All rights reserved, Ifri, 2010 IFRI IFRI-BRUXELLES 27 RUE DE LA PROCESSION RUE MARIE-THÉRÈSE, 21 75740 PARIS CEDEX 15 - FRANCE 1000 - BRUXELLES, BELGIQUE PH. : +33 (0)1 40 61 60 00 PH. : +32 (2) 238 51 10 FAX: +33 (0)1 40 61 60 60 FAX: +32 (2) 238 51 15 Email: [email protected] Email: [email protected] WEBSITE: Ifri.org China Program, Centre Asie/Ifri The Ifri China Program’s objectives are: . To organize regular exchanges with Chinese elites and enhance mutual trust through the organization of 4 annual seminars in Paris or Brussels around Chinese participants. -

Tengchongto the Border EDITOR’S Letter
NOV/DEC 2017 NOV/DEC 008 SKYInflight Magazine TIMES LISTENING TO THE SOUNDS OF OLD BEIJING DAY AT THE MUSEUMS American Airlines Tightens Ties with China PRODUCING THE PERFECT POTTERY TengchongTo the Border EDITOR’S Letter Food, Fun and Festivities very autumn, the water level of the Yangtze River in Hubei begins to drop and the nearby lakes become thick bogs covered in webs of detritus. Men come in little boats, paddling their way across the Esinking river in the dim, blue-grey light before sunrise. They are looking for lotus root, the starchy staple that is a highlight of much Chinese cooking, and gives a sweetish solidity to a winter soup. This is the one segment of my favorite documentary TV series A Bite of China, which introduced the history and stories behind food, eating and cooking, and aroused lots of people’s interests in it. Food is always a hot topic, and everyone has something to say about it. Just like United States celebrity cook Rachael Ray said: “Never be a food snob. Learn from everyone you meet — the fish guy at your market, the lady at the local diner, farmers and cheese makers. Ask questions, try everything and eat up!” In our November/December edition, we are talking food. We bring you a warm and interesting story, focusing on six food lovers and the gourmet dishes of their hometowns. They include pilots, flight attendants, an air traffic controller and a head chef. Even though they come from different places, with diversified cultures, they share the same feelings about food.