2021 Recommended Child and Adolescent Immunization Schedule
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Vaccine to Prevent Human Papillomavirus
Resolution No. 6/20-1 ADVISORY COMMITTEE ON IMMUNIZATION PRACTICES VACCINES FOR CHILDREN PROGRAM VACCINES TO PREVENT MENINGOCOCCAL DISEASE The purpose of this resolution is to update the resolution to reflect currently available meningococcal conjugate vaccines that can be used to prevent meningococcal disease attributable to serogroups A, C, W, and Y. VFC resolution 6/19-7 is repealed and replaced by the following: Meningococcal Conjugate Vaccines (MenACWY) Eligible Groups • Children aged 2 months through 10 years who are at increased risk for meningococcal disease attributable to serogroups A, C, W, and Y, including: o Children who have persistent complement component deficiencies (including inherited or chronic deficiencies in C3, C5-C9, properdin, factor H, or factor D) o Children taking a complement inhibitor (e.g., eculizumab [Soliris], ravulizumab [Ultomiris]) o Children who have anatomic or functional asplenia, including sickle cell disease o Children infected with human immunodeficiency virus (HIV) o Children traveling to or residing in countries in which meningococcal disease is hyperendemic or epidemic, particularly if contact with local population will be prolonged o Children identified to be at increased risk because of a meningococcal disease outbreak attributable to serogroups A, C, W, or Y • All children aged 11 through 18 years 1 Recommended Vaccination Schedule and Intervals The table below lists meningococcal conjugate vaccines currently available to prevent meningococcal disease attributable to serogroups A, C, W, and -

An Atlas of Potentially Water-Related Diseases in South Africa
AN ATLAS OF POTENTIALLY WATER-RELATED DISEASES IN SOUTH AFRICA Volume 2 Bibliography Report to the WATER RESEARCH COMMISSION by N Coetzee and D E Bourne Department of Community Health University of Cape Town Medical School WRC Report no. 584/2/96 ISBN 1 86845 245 X ISBN Set No 1 86845 246 8 1 CONTENTS VOLUME 2 BIBLIOGRAPHY 1 Introduction 2 2 Amoebiasis 3 3 Arthropod-borne viral diseases 7 4 Cholera 10 5 Diarrhoeal diseases in childhood 14 6 Viral hepatitis A and E 17 7 Leptospirosis 20 3 Pediculosis 22 9 Malaria 23 10 Poliomyelitis 29 11 Scabies 33 12 Schistosomiasis 35 13 Trachoma 39 14 Typhoid Fever 42 15 Intestinal helminthiasis 46 1. INTRODUCTION As many professionals involved in the management of water resources do not have a medical or public health background, it was thought that an explanatory bibliography of the major water related diseases in South Africa would be of use. Each section of the bibliography has (where appropriate) the following sections: 1. Aetiology 2. Transmission 3. Preventive and curative steps 4. South African data 5. References The MEDLINE data base of the national Library of Medicine, Washington DC, and the WATERLIT data base of the CSIR were searched. These were supplemented by South African journals and reports not appearing in the MEDLINE data base. 3 2. AMOEBIASIS 2.1. Aetiology The protozoan parasite Entamoeba histolytica which causes amoebiasis may exist as a hardy infective cyst or a more fragile and potentially pathogenic trophozoite (the "amoebic" form). Amoebiasis most commonly affects the colon and rectum as primary sitas of infection, with extraintestinal (most commonly liver abscesses), local or systemic, spread possible if not treated early. -

362.Full.Pdf
AMERICAN ACADEMY OF PEDIATRICS Committee on Infectious Diseases Policy Statement: Recommendations for the Prevention of Pneumococcal Infections, Including the Use of Pneumococcal Conjugate Vaccine (Prevnar), Pneumococcal Polysaccharide Vaccine, and Antibiotic Prophylaxis ABSTRACT. Heptavalent pneumococcal conjugate vac- lular pertussis; HbOC, Haemophilus influenzae type b conjugate cine (PCV7) is recommended for universal use in chil- vaccine; HIV, human immunodeficiency virus; AOM, acute otitis dren 23 months and younger, to be given concurrently media. with other recommended childhood vaccines at 2, 4, 6, and 12 to 15 months of age. For children 7 to 23 months he purpose of this report is to provide recom- old who have not received previous doses of PCV7, ad- ministration of a reduced number of doses is recom- mendations for use of the heptavalent pneumo- mended. Two doses of PCV7 are recommended for chil- Tcoccal conjugate vaccine (PCV7), Prevnar (Led- dren 24 to 59 months old at high risk of invasive erle Laboratories, Pearl River, NY; Wyeth-Ayerst pneumococcal infection—including children with func- Pharmaceuticals, Marietta, PA), and 23-valent pneumo- tional, anatomic, or congenital asplenia; infection with coccal polysaccharide (23PS) vaccines. In addition, rec- human immunodeficiency virus; and other predisposing ommendations for the continuing use of antibiotic pro- conditions—who have not been immunized previously phylaxis in children with sickle cell disease (SCD) and with PCV7. Recommendations have been made for use of asplenia will be given, and the use of antibiotics and 23-valent pneumococcal polysaccharide (23PS) vaccine in vaccines in children who attend out-of-home care will high-risk children to expand serotype coverage. -
Food Handler Exclusion Guidelines
Food Handler Exclusion Guidelines A guide for determining suitable exclusion periods for ill food handlers November 2017 Food handler exclusion guidelines Published by the State of Queensland (Queensland Health), November 2017 This document is licensed under a Creative Commons Attribution 3.0 Australia licence. To view a copy of this licence, visit creativecommons.org/licenses/by/3.0/au © State of Queensland (Queensland Health) 2017 You are free to copy, communicate and adapt the work, as long as you attribute the State of Queensland (Queensland Health). For more information contact: Food Safety Standards and Regulation, Department of Health, GPO Box 48, Brisbane QLD 4001, email [email protected], phone 07 3328 9310. An electronic version of this document is available at www.health.qld.gov.au. Disclaimer: The content presented in this publication is distributed by the Queensland Government as an information source only. The State of Queensland makes no statements, representations or warranties about the accuracy, completeness or reliability of any information contained in this publication. The State of Queensland disclaims all responsibility and all liability (including without limitation for liability in negligence) for all expenses, losses, damages and costs you might incur as a result of the information being inaccurate or incomplete in any way, and for any reason reliance was placed on such information. Food Handler Exclusion Guidelines - ii - Contents 1. Introduction ............................................................................................... -

PEDIARIX Is a Vaccine
HIGHLIGHTS OF PRESCRIBING INFORMATION • If Guillain-Barré syndrome occurs within 6 weeks of receipt of a prior These highlights do not include all the information needed to use vaccine containing tetanus toxoid, the decision to give PEDIARIX should PEDIARIX safely and effectively. See full prescribing information for be based on potential benefits and risks. (5.2) PEDIARIX. • The tip caps of the prefilled syringes contain natural rubber latex which may cause allergic reactions. (5.3) PEDIARIX [Diphtheria and Tetanus Toxoids and Acellular Pertussis • Syncope (fainting) can occur in association with administration of Adsorbed, Hepatitis B (Recombinant) and Inactivated Poliovirus injectable vaccines, including PEDIARIX. Procedures should be in place Vaccine], Suspension for Intramuscular Injection to avoid falling injury and to restore cerebral perfusion following Initial U.S. Approval: 2002 syncope. (5.4) • If temperature ≥105°F, collapse or shock-like state, or persistent, ----------------------------- INDICATIONS AND USAGE ---------------------------- PEDIARIX is a vaccine indicated for active immunization against diphtheria, inconsolable crying lasting ≥3 hours have occurred within 48 hours after tetanus, pertussis, infection caused by all known subtypes of hepatitis B virus, receipt of a pertussis-containing vaccine, or if seizures have occurred and poliomyelitis. PEDIARIX is approved for use as a 3-dose series in infants within 3 days after receipt of a pertussis-containing vaccine, the decision born of hepatitis B surface antigen (HBsAg)-negative mothers. PEDIARIX to give PEDIARIX should be based on potential benefits and risks. (5.5) may be given as early as 6 weeks of age through 6 years of age (prior to the • For children at higher risk for seizures, an antipyretic may be 7th birthday). -

CLINICAL TRIALS Safety and Immunogenicity of a Nicotine Conjugate Vaccine in Current Smokers
CLINICAL TRIALS Safety and immunogenicity of a nicotine conjugate vaccine in current smokers Immunotherapy is a novel potential treatment for nicotine addiction. The aim of this study was to assess the safety and immunogenicity of a nicotine conjugate vaccine, NicVAX, and its effects on smoking behavior. were recruited for a noncessation treatment study and assigned to 1 of 3 doses of the (68 ؍ Smokers (N nicotine vaccine (50, 100, or 200 g) or placebo. They were injected on days 0, 28, 56, and 182 and monitored for a period of 38 weeks. Results showed that the nicotine vaccine was safe and well tolerated. Vaccine immunogenicity was dose-related (P < .001), with the highest dose eliciting antibody concentrations within the anticipated range of efficacy. There was no evidence of compensatory smoking or precipitation of nicotine withdrawal with the nicotine vaccine. The 30-day abstinence rate was significantly different across with the highest rate of abstinence occurring with 200 g. The nicotine vaccine appears ,(02. ؍ the 4 doses (P to be a promising medication for tobacco dependence. (Clin Pharmacol Ther 2005;78:456-67.) Dorothy K. Hatsukami, PhD, Stephen Rennard, MD, Douglas Jorenby, PhD, Michael Fiore, MD, MPH, Joseph Koopmeiners, Arjen de Vos, MD, PhD, Gary Horwith, MD, and Paul R. Pentel, MD Minneapolis, Minn, Omaha, Neb, Madison, Wis, and Rockville, Md Surveys show that, although about 41% of smokers apy, is about 25% on average.2 Moreover, these per- make a quit attempt each year, less than 5% of smokers centages most likely exaggerate the efficacy of are successful at remaining abstinent for 3 months to a intervention because these trials are typically composed year.1 Smokers seeking available behavioral and phar- of subjects who are highly motivated to quit and who macologic therapies can enhance successful quit rates are free of complicating diagnoses such as depression 2 by 2- to 3-fold over control conditions. -

The Hepatitis B Vaccine Is the Most Widely Used Vaccine in the World, with Over 1 Billion Doses Given
Hepatitis B Vaccine Protect Yourself and Those You Love What is Hepatitis B? Hepatitis B is the most common serious liver infection in the world. It is caused by the hepatitis B virus (HBV), which attacks liver cells and can lead to liver failure, cirrhosis (scarring), or liver cancer later in life. The virus is transmitted through direct contact with infected blood and bodily fluids, and from an infected woman to her newborn at birth. Is there a safe vaccine for hepatitis B? YES! The good news is that there is a safe and effective vaccine for hepatitis B. The vaccine is a series, typically given as three shots over a six-month period that will provide a lifetime of protection. You cannot get hepatitis B from the vaccine – there is no human blood or live virus in the vaccine. The hepatitis B vaccine is the most widely used vaccine in the world, with over 1 billion doses given. The hepatitis B vaccine is the first "anti-cancer" vaccine because it can help prevent liver cancer! Who should be vaccinated against hepatitis B? The World Health Organization (WHO) and the U.S. Centers for Disease Control and Prevention (CDC) recommend the hepatitis B vaccine for all newborns and children up to 18 years of age, and all high-risk adults. All infants should receive the first dose of the vaccine in the delivery room or in the first 24 hours of life, preferably within 12 hours. (CDC recommends the first dose within 12 hours vs. the WHO recommendation of 24 hours.) The HBV vaccine is recommended to anyone who is at high risk of infection. -

Engerix-B Data Sheet
NEW ZEALAND DATA SHEET 1. PRODUCT NAME ENGERIX-B 20 micrograms/mL, suspension for injection. ENGERIX-B paediatric 10 micrograms/0.5 mL, suspension for injection. 2. QUALITATIVE AND QUANTITATIVE COMPOSITION ENGERIX-B paediatric dose: 10 microgram (µg) dose vaccine 1 dose (0.5 mL) contains: Hepatitis B surface antigen 1, 2 10 micrograms 1Adsorbed on aluminium hydroxide, hydrated Total: 0.25 milligrams Al3+ 2Produced in yeast cells (Saccharomyces cerevisiae) by recombinant DNA technology ENGERIX-B: 20 microgram (µg) dose vaccine 1 dose (1 mL) contains: Hepatitis B surface antigen1, 2 20 micrograms 1Adsorbed on aluminium hydroxide, hydrated Total: 0.50 milligrams Al3+ 2Produced in yeast cells (Saccharomyces cerevisiae) by recombinant DNA technology The vaccine is highly purified, and meets the WHO requirements for recombinant hepatitis B vaccines. No substances of human origin are used in its manufacture. For the full list of excipients, see section 6.1 List of excipients. 3. PHARMACEUTICAL FORM Suspension for injection. ENGERIX-B is a turbid white suspension. Upon storage, a fine white deposit with a clear colourless supernatant may be observed. 4. CLINICAL PARTICULARS 4.1 Therapeutic indications ENGERIX-B is indicated for active immunisation against hepatitis B virus infection. As part of the national immunisation schedule, the New Zealand Ministry of Health* recommend all infants, unvaccinated children up to the age of 16 years, and household and sexual contacts of known hepatitis B carriers receive a primary course of vaccination against hepatitis B. 1 Immunisation is also recommended for seronegative persons who are at substantial risk and have been demonstrated or judged to be susceptible to the hepatitis B virus (HBV). -

Inhibition of HIV-1 by an Anti-Integrase Single-Chain Variable
Gene Therapy (1999) 6, 660–666 1999 Stockton Press All rights reserved 0969-7128/99 $12.00 http://www.stockton-press.co.uk/gt Inhibition of HIV-1 by an anti-integrase single-chain variable fragment (SFv): delivery by SV40 provides durable protection against HIV-1 and does not require selection M BouHamdan1, L-X Duan1, RJ Pomerantz1 and DS Strayer1,2 1The Dorrance H Hamilton Laboratories, Center for Human Virology, Division of Infectious Diseases, Department of Medicine; and 2Department of Pathology, Anatomy and Cell Biology, Jefferson Medical College, Thomas Jefferson University, Philadelphia, PA, USA Human immunodeficiency virus type I (HIV-1) encodes the SFv-IN was confirmed by Western blotting and several proteins that are packaged into virus particles. Inte- immunofluorescence staining, which showed that Ͼ90% of grase (IN) is an essential retroviral enzyme, which has SupT1 T-lymphocytic cells treated with SV(Aw) expressed been a target for developing agents to inhibit virus repli- the SFv-IN protein without selection. When challenged, cation. In previous studies, we showed that intracellular HIV-1 replication, as measured by HIV-1 p24 antigen expression of single-chain variable antibody fragments expression and syncytium formation, was potently inhibited (SFvs) that bind IN, delivered via retroviral expression vec- in cells expressing SV40-delivered SFv-IN. Levels of inhi- tors, provided resistance to productive HIV-1 infection in bition of HIV-1 infection achieved using this approach were T-lymphocytic cells. In the current studies, we evaluated comparable to those achieved using murine leukemia virus simian-virus 40 (SV40) as a delivery vehicle for anti-IN (MLV) as a transduction vector, the major difference being therapy of HIV-1 infection. -

Evolution of Hepatitis B Serological Markers in HIV Coinfected Patients: a Case Study
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Cadernos Espinosanos (E-Journal) Rev Saúde Pública 2017;51:24 Artigo Original http://www.rsp.fsp.usp.br/ Evolution of hepatitis B serological markers in HIV coinfected patients: a case study Ana Luiza de Castro Conde ToscanoI,II, Maria Cássia Mendes CorrêaII,III I Instituto de Infectologia Emílio Ribas. São Paulo, SP, Brasil II Departamento de Doenças Infecciosas. Faculdade de Medicina. Universidade de São Paulo. São Paulo, SP, Brasil III Instituto de Medicina Tropical de São Paulo. Laboratório de Investigação Médica 52. São Paulo, SP, Brasil ABSTRACT OBJECTIVE: To describe the evolution of serological markers among HIV and hepatitis B coinfected patients, with emphasis on evaluating the reactivation or seroreversion of these markers. METHODS: The study population consisted of patients met in an AIDS Outpatient Clinic in São Paulo State, Brazil. We included in the analysis all HIV-infected and who underwent at least two positive hepatitis B surface antigen serological testing during clinical follow up, with tests taken six months apart. Patients were tested with commercial kits available for hepatitis B serological markers by microparticle enzyme immunoassay. Clinical variables were collected: age, sex, CD4+ T-cell count, HIV viral load, alanine aminotransferase level, exposure to antiretroviral drugs including lamivudine and/or tenofovir. RESULTS: Among 2,242 HIV positive patients, we identified 105 (4.7%) patients with chronic hepatitis B. Follow up time for these patients varied from six months to 20.5 years. All patients underwent antiretroviral therapy during follow-up. Among patients with chronic hepatitis B, 58% were hepatitis B “e” antigen positive at the first assessment. -
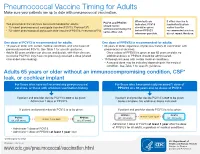
Pneumococcal Vaccine Timing for Adults Make Sure Your Patients Are up to Date with Pneumococcal Vaccination
Pneumococcal Vaccine Timing for Adults Make sure your patients are up to date with pneumococcal vaccination. When both are If either vaccine is PCV13 and PPSV23 Two pneumococcal vaccines are recommended for adults: indicated, PCV13 inadvertently given should not be 13-valent pneumococcal conjugate vaccine (PCV13, Prevnar13®) should be given earlier than the administered during the ® before PPSV23 recommended window, 23-valent pneumococcal polysaccharide vaccine (PPSV23, Pneumovax 23) same office visit. whenever possible. do not repeat the dose. One dose of PCV13 is recommended for adults: One dose of PPSV23 is recommended for adults: 19 years or older with certain medical conditions and who have not 65 years or older, regardless of previous history of vaccination with previously received PCV13. See Table 1 for specific guidance. pneumococcal vaccines. Adults 65 years or older can discuss and decide, with their clinician, – Once a dose of PPSV23 is given at age 65 years or older, no to receive PCV13 if they have not previously received a dose (shared additional doses of PPSV23 should be administered. clinical decision-making). 19 through 64 years with certain medical conditions. – A second dose may be indicated depending on the medical condition. See Table 1 for specific guidance. Adults 65 years or older without an immunocompromising condition, CSF* leak, or cochlear implant For those who have not received any pneumococcal For those who have previously received 1 dose of vaccines, or those with unknown vaccination history PPSV23 at ≥ 65 years and no doses of PCV13 If patient and provider decide PCV13 is not to be given: If patient and provider decide PCV13 is not to be given: Administer 1 dose of PPSV23. -
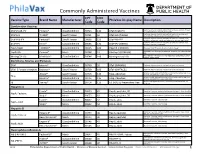
Commonly Administered Vaccines
Commonly Administered Vaccines CPT CVX Vaccine Type Brand Name Manufacturer PhilaVax Display Name Description Code Code Combination Vaccines Diptheria, tetanus toxoids and acellular pertussis vaccine, Hepati- DTaP-HepB-IPV Pediarix® GlaxoSmithKline 90723 110 DTaP-HepB-IPV tis B and poliovirus vaccine, inactivated Diptheria, tetanus toxoids and acellular pertussis vaccine and DTaP-Hib TriHIBit® Sanofi Pasteur 90721 50 DTaP-Hib (TriHIBit) Haemophilus influenzae type b conjugate vaccine Diptheria, tetanus toxoids and acellular pertussis vaccine, Hae- DTaP-Hib-IPV Pentacel® Sanofi Pasteur 90698 120 DTaP-Hib-IPV mophilus influenzae type b, and poliovirus vaccine, inactivated Diptheria, tetanus toxoids and acellular pertussis vaccine, and DTaP-IPV Kinrix® GlaxoSmithKline 90696 130 DTaP-IPV (KINRIX) poliovirus vaccine, inactivated HepA-HepB TWINRIX® GlaxoSmithKline 90636 104 HepA/B (TWINRIX) Hepatisis A and Hepatitis B vaccine, adult dosage Hepatitis B and Hemophilus influenza b vaccine, for intramuscular HepB-Hib Comvax® Merck 90748 51 Hib-Hep B (COMVAX) use Haemophilus influenza b and meningococcal sero groups C and Y MeningC/Y-Hib Menhibrix® GlaxoSmithKline 90644 148 Meningococcal-Hib vaccine, 4 dose series Diphtheria, Tetanus and Pertussis DTaP Infanrix® GlaxoSmithKline 90700 20 DTaP (INFANRIX) Diptheria, tetanus toxoids and acellular pertussis vaccine DTaP, 5 Pertussis Antigens Daptacel® Sanofi Pasteur 90700 106 DTaP (DAPTACEL) Diptheria, tetanus toxoids and acellular pertussis vaccine Tetanus toxoid, reduced diphtheria toxoid, and acellular