PEDIARIX Is a Vaccine
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Corporate Governance
Strategic report Governance and remuneration Financial statements Investor information Corporate Governance In this section Chairman’s Governance statement 78 The Board 80 Corporate Executive Team 83 Board architecture 85 Board roles and responsibilities 86 Board activity and principal decisions 87 Our purpose, values and culture 90 The Board’s approach to engagement 91 Board performance 94 Board Committee information 96 Our Board Committee reports 97 Section 172 statement 108 Directors’ report 109 GSK Annual Report 2020 77 Chairman’s Governance statement In last year’s Governance statement, I explained that our primary Education and focus on Science objective for 2020 was to ensure there was clarity between the Given the critical importance of strengthening the pipeline, Board and management on GSK’s execution of strategy and its the Board has benefitted from devoting a higher proportion of operational priorities. We have aligned our long-term priorities its time in understanding the science behind our strategy and of Innovation, Performance and Trust powered by culture testing its application. It is important that the Board has a and agreed on the metrics to measure delivery against them. working understanding of the key strategic themes upon The Board’s annual cycle of meetings ensures that all major which our R&D strategy is based. These themes have been components of our strategy are reviewed over the course complemented by Board R&D science thematic deep dives. of the year. Our focus was on the fundamentals of our strategy: human The COVID-19 pandemic impacted and dominated all our genetics, the immune system and AI and ML, as well as to lives for the majority of 2020. -
Food Handler Exclusion Guidelines
Food Handler Exclusion Guidelines A guide for determining suitable exclusion periods for ill food handlers November 2017 Food handler exclusion guidelines Published by the State of Queensland (Queensland Health), November 2017 This document is licensed under a Creative Commons Attribution 3.0 Australia licence. To view a copy of this licence, visit creativecommons.org/licenses/by/3.0/au © State of Queensland (Queensland Health) 2017 You are free to copy, communicate and adapt the work, as long as you attribute the State of Queensland (Queensland Health). For more information contact: Food Safety Standards and Regulation, Department of Health, GPO Box 48, Brisbane QLD 4001, email [email protected], phone 07 3328 9310. An electronic version of this document is available at www.health.qld.gov.au. Disclaimer: The content presented in this publication is distributed by the Queensland Government as an information source only. The State of Queensland makes no statements, representations or warranties about the accuracy, completeness or reliability of any information contained in this publication. The State of Queensland disclaims all responsibility and all liability (including without limitation for liability in negligence) for all expenses, losses, damages and costs you might incur as a result of the information being inaccurate or incomplete in any way, and for any reason reliance was placed on such information. Food Handler Exclusion Guidelines - ii - Contents 1. Introduction ............................................................................................... -

Final Attendee List
Jennifer Abnet GlaxoSmithKline I GlaxoSmithKline I Jane Arboleda APRN Guardant I Molly Benson Sanjiv Agarwala MD Puma Biotechnology I Cancer Expert Now I Joe Arminger AbbVie I Seth Berkowitz LCSW, Manmeet Ahluwalia MD, CCLS MBA Patricia Armstrong The Leukemia & Lymphoma Miami Cancer Institute I Novartis I Society V Steve Albers Kim Arnold APRN CPNP Barry Berman MD, MS Alexion V CPHON Florida Cancer Specialists I Servier Pharmaceuticals I Maritza Alencar DNP, Tizano Bernard MBA, APRN, BMTCN Sheila Arrington MSN, Cancer Care Centers of Miami Cancer Institute V APRN, NP-C, AOCN Brevard I Puma Biotechnology I Carmen Allen MSIT Ana Mari Bernardini Pharmavoxx V Shannon Ashmon Novartis Oncology I Eisai, Inc I Luly Almeida Bernard Berry MBA Incyte Corporation I Sarah Ashton MS AstraZeneca Pharmaceuticals Guardant Health I I Talat Almukhtar MD Orlando Health Cancer Melissa Austin Jason Bever Institute I Cancer Care Centers of Oncopeptides I Brevard I Beatrice Alvarado Roberts Amy Bignon MD Garland Avera Doyle Caris Life Sciences I University of Florida I Jazz Pharmaceuticals I Nadeem Bilani MD Tadeu Ambros MD Francie Babcock Cleveland Clinic I FCS I AMAG Pharmaceuticals/Covis I Angela Bilik RN BSN Douglas Anderson AstraZeneca I Incyte Corporation I Craig Bailey Astra Zeneca I Jamie Bilsky BS Blesson Andrews Genentech V Genentech I Kevin Barr Daiichi Sankyo I Rohit Bishnoi MD Ollie Annum PharmD University of Florida I BHMCR I Leonard Bennett PharmD EMD Serono I Brady Blackman Susmitha Apuri MD MorphoSys I Florida Cancer Specialists I Michael Bennett As of 4-22-21 Kimberly Blandon RN MSN Rick Breitenstein Memorial Cancer Institute I Apellis Pharmaceuticals I Denise Capo Karyopharm Therapeutics I Taryn Boiteau GlaxoSmithKline I Amanda Bridges Florida Society of Clinical Heidi Caravetta Tracy Bonds RN, BSN, Oncology I Exelixis, Inc. -
Diphtheria, Tetanus, Pertussis, Polio, Hib and Hepatitis B Vaccine for Babies and Children
Diphtheria, Tetanus, Pertussis, Polio, Hib and Hepatitis B vaccine for babies and children This leaflet tells you about the DTaP/IPV/Hib/ HepB vaccine, also known as “6 in 1” as it protects against six diseases, diphtheria, tetanus, pertussis (whooping cough), polio, Haemophilus influenzae type b and hepatitis B (HepB) disease. What does the vaccine protect against? Diphtheria Diphtheria is a serious disease that usually begins with a sore throat and can quickly cause breathing problems. It can damage the heart and nervous system and, in severe cases, can kill. Before diphtheria vaccine was introduced in the UK, there were up to 70,000 cases of diphtheria and around 5,000 deaths a year. Diphtheria can be spread from person to person through close contact. Tetanus Tetanus is a disease affecting the nervous system which can cause muscle spasms and breathing problems and can kill. It is caused when germs found in soil and manure get into the body through wounds or burns. Tetanus cannot be passed from person to person. 2 Published June 2018 Pertussis (whooping cough) Whooping cough is a disease that can cause long bouts of coughing and choking, making it hard to breathe. It can last for up to 10 weeks and babies under one year of age are most at risk. The disease is very serious and can kill. Before the pertussis vaccine was introduced, the average number of cases reported each year in the UK was 120,000 and 92 children died in the year before the vaccine was introduced. Whooping cough is usually spread by coughs and sneezes. -

GLAXOSMITHKLINE LLC V. TEVA PHARMACEUTICALS USA, INC
Case: 18-1976 Document: 111 Page: 1 Filed: 10/02/2020 United States Court of Appeals for the Federal Circuit ______________________ GLAXOSMITHKLINE LLC, SMITHKLINE BEECHAM (CORK) LIMITED, Plaintiffs-Appellants v. TEVA PHARMACEUTICALS USA, INC., Defendant-Cross-Appellant ______________________ 2018-1976, 2018-2023 ______________________ Appeals from the United States District Court for the District of Delaware in No. 1:14-cv-00878-LPS-CJB, Chief Judge Leonard P. Stark. ______________________ Decided: October 2, 2020 ______________________ JUANITA ROSE BROOKS, Fish & Richardson, PC, San Diego, CA, argued for plaintiffs-appellants. Also represented by MICHAEL ARI AMON, CRAIG E. COUNTRYMAN, JONATHAN ELLIOT SINGER; ELIZABETH M. FLANAGAN, MICHAEL J. KANE, WILLIAM WOODFORD, Minneapolis, MN; DOUGLAS E. MCCANN, Wilmington, DE. WILLIAM M. JAY, Goodwin Procter LLP, Washington, DC, argued for defendant-cross-appellant. Also represented by JAIME ANN SANTOS; ELAINE BLAIS, J. Case: 18-1976 Document: 111 Page: 2 Filed: 10/02/2020 2 GLAXOSMITHKLINE LLC v. TEVA PHARMACEUTICALS USA, INC. ANTHONY DOWNS, ROBERT FREDERICKSON, III, CHRISTOPHER T. HOLDING, ALEXANDRA LU, LANA S. SHIFERMAN, DARYL L. WIESEN, Boston, MA; IRA J. LEVY, New York, NY. HANSJORG SAUER, Biotechnology Innovation Organization, Washington, DC, for amicus curiae Biotechnology Innovation Organization. Also represented by MELISSA A. BRAND; BRIAN PAUL BARRETT, Eli Lilly and Company, Indianapolis, IN. MICHAEL N. KENNEDY, Covington & Burling LLP, Washington, DC, for amicus curiae Pharmaceutical Research and Manufacturers of America. Also represented by STEVEN JOHN WINKELMAN; DAVID EVAN KORN, Pharmaceutical Research and Manufacturers Association of America, Washington, DC. ANDREW CURTIS NICHOLS, Winston & Strawn LLP, Washington, DC, for amicus curiae Association for Accessible Medicines. Also represented by GEORGE C. -

Press Release Sanofi Pasteur Sanofi Pasteur Mounts Emergency
Press release Sanofi Pasteur Lyon, France, February 26, 2008 Sanofi Pasteur: www.sanofipasteur.com Media Relations: Tel.: + 33 4 37 37 50 38 Media Relations US: Tel.: + 1 570 839 44 46 Sanofi Pasteur Mounts Emergency Response to Yellow Fever Epidemic in Latin America - Six Million Doses of StamarilTM vaccine shipped in record time to Brazil and Paraguay - Sanofi Pasteur, the vaccines division of the sanofi-aventis Group, announced today that six million doses of StamarilTM1 yellow fever vaccine have been shipped upon UNICEF’s request to respond to the yellow fever epidemic in Latin America. Brazil received four million doses of StamarilTM vaccine early February and an additional two million doses were shipped to Paraguay over the weekend in response to urgent requests from Health Authorities. “Sanofi Pasteur mobilized its teams to make this public health emergency a priority,” said Wayne Pisano, President and Chief Executive Officer of Sanofi Pasteur. “This ability to respond to an emergency in record time illustrates the company’s commitment to global health.” The yellow fever vaccine that was provided to Brazil and Paraguay is part of the UNICEF vaccine stockpile which is reserved for outbreak responses. Sanofi Pasteur is currently the only vaccine supplier to the UNICEF yellow fever vaccine stockpile. Sanofi Pasteur is the largest provider of yellow fever vaccine worldwide with 200 million doses of vaccine provided to 150 countries over the past 20 years. About yellow fever Yellow fever is a viral disease that occurs in both rural and urban areas in Africa and South America. There is no treatment for yellow fever, only prevention by immunization. -

Declarations of Interest Thorax: First Published As 10.1136/Thoraxjnl-2016-209333.476 on 15 November 2016
Declarations of interest Thorax: first published as 10.1136/thoraxjnl-2016-209333.476 on 15 November 2016. Downloaded from KF Rabe reports financial for support for consultancy work P297 LUNG-FUNCTION PROFILE BEFORE AND AFTER THE from AstraZeneca, Chiesi, Novartis, MSD and GlaxoSmithKline, FIRST MODERATE TO SEVERE EXACERBATION DURING and grants from Altana, Novartis, AstraZeneca, MSD and THE WISDOM STUDY Nycomed. F Maltais reports financial support from Boehringer Ingelheim 10.1136/thoraxjnl-2016-209333.476 during the conduct of the study and, outside of the submitted work, financial support from Boehringer Ingelheim and GlaxoS- E Wouters, outside of the submitted work, reports personal fees mithKline for attendance at advisory boards, financial support from AstraZeneca, GlaxoSmithKline, Novartis, Takeda, Pfizer from Boehringer Ingelheim, GlaxoSmithKline, AstraZeneca and and Boehringer Ingelheim, and grants from AstraZeneca, GlaxoS- Novartis for speaking activities, and research support from Boeh- mithKline and Novartis. ringer Ingelheim, GlaxoSmithKline, AstraZeneca, Nycomed and H Magnussen received funding from Almirall, AstraZeneca, Novartis. Boehringer Ingelheim, Chiesi, GlaxoSmithKline, Merck, Novar- tis, Takeda and Roche to conduct clinical studies, and has spoken at meetings and is a member of advisory boards for these and P295 EFFICACY AND SAFETY OF TIOTROPIUM/OLODATEROL other companies. IN PATIENTS WITH COPD BY ATS CATEGORY R Rodriguez-Roisin reports personal fees from AstraZeneca, Boehringer Ingelheim, Mylan, Pearl Therapeutics, Takeda, Teva 10.1136/thoraxjnl-2016-209333.474 and Ferrer, and grants and personal fees from Menarini and Almirall. F Maltais reports financial support from Boehringer Ingelheim K Tetzlaff and S Bell are employees of Boehringer Ingelheim during the conduct of the study and, outside of the submitted Pharma GmbH & Co. -
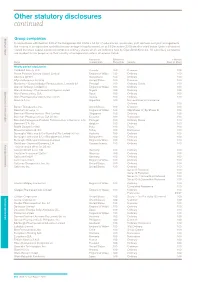
Other Statutory Disclosures Continued
Other statutory disclosures continued Strategic reportGroup companies Governance & remuneration Financial statements In accordance with Section 409 of the Companies Act 2006 a full list of subsidiaries, associates, joint ventures and joint arrangements, the country of incorporation and effective percentage of equity owned, as at 31 December 2015 are disclosed below. Unless otherwise stated the share capital disclosed comprises ordinary shares which are indirectly held by GlaxoSmithKline plc. All subsidiary companies are resident for tax purposes in their country of incorporation unless otherwise stated. Country of Effective % % Held by Name incorporation Ownership Security Class of Share Wholly owned subsidiaries 1506369 Alberta ULC Canada 100 Common 100 Action Potential Venture Capital Limited England & Wales 100 Ordinary 100 Adechsa GmbH Switzerland 100 Ordinary 100 Affymax Research Institute United States 100 Common 100 Alenfarma – Especialidades Farmaceuticas, Limitada (iv) Portugal 100 Ordinary Quota 100 Allen & Hanburys Limited (iv) England & Wales 100 Ordinary 100 Allen & Hanburys Pharmaceutical Nigeria Limited Nigeria 100 Ordinary 100 Allen Farmaceutica, S.A. Spain 100 Ordinary 100 Allen Pharmazeutika Gesellschaft m.b.H. Austria 100 Ordinary 100 Aners S.A (iv) Argentina 100 Non-endorsable Nominative Ordinary 100 Barrier Therapeutics, Inc. United States 100 Common 100 Beecham Group p l c England & Wales 100 20p Shares 'A'; 5p Shares B 100 Beecham Pharmaceuticals (Pte) Limited Singapore 100 Ordinary 100 Beecham Pharmaceuticals S.A (iv) (vi) Ecuador 100 Nominative 100 Beecham Portuguesa-Produtos Farmaceuticos e Quimicos, Lda Portugal 100 Ordinary Quota 100 Beecham S.A. (iv) Belgium 100 Ordinary 100 Biddle Sawyer Limited India 100 Equity 100 Biovesta Ilaçlari Ltd. Sti. Turkey 100 Nominative 100 Burroughs Wellcome & Co (Australia) Pty Limited (iv) (vi) Australia 100 Ordinary 100 Burroughs Wellcome & Co (Bangladesh) Limited Bangladesh 100 Ordinary 100 Burroughs Wellcome International Limited England & Wales 100 Ordinary 100 Caribbean Chemical Company, Ltd. -

Hepatitis B? HEPATITIS B Hepatitis B Is a Contagious Liver Disease That Results from Infection with the Hepatitis B Virus
What is Hepatitis B? HEPATITIS B Hepatitis B is a contagious liver disease that results from infection with the Hepatitis B virus. When first infected, a person can develop Are you at risk? an “acute” infection, which can range in severity from a very mild illness with few or no symptoms to a serious condition requiring hospitalization. Acute Hepatitis B refers to the first 6 months after someone is exposed to the Hepatitis B virus. Some people are able to fight the infection and clear the virus. For others, the infection remains and leads to a “chronic,” or lifelong, illness. Chronic Hepatitis B refers to the illness that occurs when the Hepatitis B virus remains in a person’s body. Over time, the infection can cause serious health problems. How is Hepatitis B spread? Hepatitis B is usually spread when blood, semen, or other body fluids from a person infected with the Hepatitis B virus enter the body of someone who is not infected. This can happen through having sex with an infected partner; sharing needles, syringes, or other injection drug equipment; or from direct contact with the blood or open sores of an infected person. Hepatitis B can also be passed from an infected mother to her baby at birth. Who should be tested for Hepatitis B? Approximately 1.2 million people in the United States and 350 million people worldwide have Hepatitis B. Testing for Hepatitis B is recommended for certain groups of people, including: Most are unaware of their infection. ■ People born in Asia, Africa, and other regions with moderate or high rates Is Hepatitis B common? of Hepatitis B (see map) Yes. -

Hepatitis A, B, and C: Learn the Differences
Hepatitis A, B, and C: Learn the Differences Hepatitis A Hepatitis B Hepatitis C caused by the hepatitis A virus (HAV) caused by the hepatitis B virus (HBV) caused by the hepatitis C virus (HCV) HAV is found in the feces (poop) of people with hepa- HBV is found in blood and certain body fluids. The virus is spread HCV is found in blood and certain body fluids. The titis A and is usually spread by close personal contact when blood or body fluid from an infected person enters the body virus is spread when blood or body fluid from an HCV- (including sex or living in the same household). It of a person who is not immune. HBV is spread through having infected person enters another person’s body. HCV can also be spread by eating food or drinking water unprotected sex with an infected person, sharing needles or is spread through sharing needles or “works” when contaminated with HAV. “works” when shooting drugs, exposure to needlesticks or sharps shooting drugs, through exposure to needlesticks on the job, or from an infected mother to her baby during birth. or sharps on the job, or sometimes from an infected How is it spread? Exposure to infected blood in ANY situation can be a risk for mother to her baby during birth. It is possible to trans- transmission. mit HCV during sex, but it is not common. • People who wish to be protected from HAV infection • All infants, children, and teens ages 0 through 18 years There is no vaccine to prevent HCV. -

Hepatitis B Vaccine – Frequently Asked Questions (Information from the CDC)
AAMC Standardized Immunization Form 2020 Hepatitis B Vaccine – Frequently Asked Questions (Information from the CDC) 1. What are the hepatitis B vaccines licensed for use in the United States? Three single-antigen vaccines and two combination vaccines are currently licensed in the United States. Single-antigen hepatitis B vaccines: • ENGERIX-B® • RECOMBIVAX HB® • HEPLISAV-B™ Combination vaccines: • PEDIARIX®: Combined hepatitis B, diphtheria, tetanus, acellular pertussis (DTaP), and inactivated poliovirus (IPV) vaccine. Cannot be administered before age 6 weeks or after age 7 years. • TWINRIX®: Combined Hepatitis A and hepatitis B vaccine. Recommended for people aged ≥18 years who are at increased risk for both HAV and HBV infections. 2. What are the recommended schedules for hepatitis B vaccination? The vaccination schedule most often used for children and adults is three doses given at 0, 1, and 6 months. Alternate schedules have been approved for certain vaccines and/or populations. A new formulation, Heplisav-B (HepB-CpG), is approved to be given as two doses one month apart. 3. If there is an interruption between doses of hepatitis B vaccine, does the vaccine series need to be restarted? No. The series does not need to be restarted but the following should be considered: • If the vaccine series was interrupted after the first dose, the second dose should be administered as soon as possible. • The second and third doses should be separated by an interval of at least 8 weeks. • If only the third dose is delayed, it should be administered as soon as possible. 4. Is it harmful to administer an extra dose of hepatitis B vaccine or to repeat the entire vaccine series if documentation of the vaccination history is unavailable or the serology test is negative? No, administering extra doses of single-antigen hepatitis B vaccine is not harmful. -

Package Inserts
Individuals using assistive technology may not be able to fully access the information contained in this file. For assistance, please send an e-mail to: [email protected] and include 508 Accommodation and the title of the document in the subject line of your e-mail. HIGHLIGHTS OF PRESCRIBING INFORMATION -----------------------WARNINGS AND PRECAUTIONS------------------------ These highlights do not include all the information needed to use • Carefully consider benefits and risks before administering VAXELIS to VAXELIS safely and effectively. See full prescribing information for persons with a history of: VAXELIS. - fever ≥40.5°C (≥105°F), hypotonic-hyporesponsive episode (HHE) or VAXELISTM (Diphtheria and Tetanus Toxoids and Acellular Pertussis, persistent, inconsolable crying lasting ≥3 hours within 48 hours after a Inactivated Poliovirus, Haemophilus b Conjugate and Hepatitis B previous pertussis-containing vaccine. (5.2) Vaccine) - seizures within 3 days after a previous pertussis-containing vaccine. (5.2) Suspension for Intramuscular Injection Initial U.S. Approval: 2018 • If Guillain-Barré syndrome occurred within 6 weeks of receipt of a prior vaccine containing tetanus toxoid, the risk for Guillain-Barré syndrome ----------------------------RECENT MAJOR CHANGES ------------------------ may be increased following VAXELIS. (5.3) Dosage and Administration (2.2) 09/2020 • Apnea following intramuscular vaccination has been observed in some ----------------------------INDICATIONS AND USAGE--------------------------- infants born prematurely. The decision about when to administer an VAXELIS is a vaccine indicated for active immunization to prevent intramuscular vaccine, including VAXELIS, to an infant born prematurely diphtheria, tetanus, pertussis, poliomyelitis, hepatitis B, and invasive disease should be based on consideration of the individual infant’s medical status due to Haemophilus influenzae type b.