Vaccinations for Infants and Children, Age 0-10 Years
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

For Schools and Parents: K-12 Immunization Requirements
FOR SCHOOLS AND PARENTS: K-12 IMMUNIZATION REQUIREMENTS NJ Department of Health (NJDOH) Vaccine Preventable Disease Program Summary of NJ School Immunization Requirements Listed in the chart below are the minimum required number of doses your child must have to attend a NJ school.* This is strictly a summary document. Exceptions to these requirements (i.e. provisional admission, grace periods, and exemptions) are specified in the Immunization of Pupils in School rules, New Jersey Administrative Code (N.J.A.C. 8:57-4). Please reference the administrative rules for more details https://www.nj.gov/health/cd/imm_requirements/acode/. Additional vaccines are recommended by Advisory Committee on Immunization Practices (ACIP) for optimal protection. For the complete ACIP Recommended Immunization Schedule, please visit http://www.cdc.gov/vaccines/schedules/index.html. Minimum Number of Doses for Each Vaccine Grade/level child DTaP Polio MMR Varicella Hepatitis Meningococcal Tdap enters school: Diphtheria, Tetanus, acellular Pertussis Inactivated (Measles, (Chickenpox) B (Tetanus, Polio Vaccine Mumps, diphtheria, (IPV) Rubella) acellular pertussis) § | Kindergarten – A total of 4 doses with one of these doses A total of 3 2 doses 1 dose 3 doses None None 1st grade on or after the 4th birthday doses with one OR any 5 doses† of these doses given on or after the 4th birthday ‡ OR any 4 doses nd th † 2 – 5 grade 3 doses 3 doses 2 doses 1 dose 3 doses None See footnote NOTE: Children 7 years of age and older, who have not been previously vaccinated with the primary DTaP series, should receive 3 doses of Td. -

Mmrv Vaccine
VACCINE INFORMATION STATEMENT (Measles, Mumps, Many Vaccine Information Statements are available in Spanish and other languages. MMRV Vaccine Rubella and See www.immunize.org/vis Varicella) Hojas de información sobre vacunas están disponibles en español y en muchos otros What You Need to Know idiomas. Visite www.immunize.org/vis These are recommended ages. But children can get the Measles, Mumps, Rubella and second dose up through 12 years as long as it is at least 1 Varicella 3 months after the first dose. Measles, Mumps, Rubella, and Varicella (chickenpox) can be serious diseases: Children may also get these vaccines as 2 separate shots: MMR (measles, mumps and rubella) and Measles varicella vaccines. • Causes rash, cough, runny nose, eye irritation, fever. • Can lead to ear infection, pneumonia, seizures, brain 1 Shot (MMRV) or 2 Shots (MMR & Varicella)? damage, and death. • Both options give the same protection. Mumps • One less shot with MMRV. • Causes fever, headache, swollen glands. • Children who got the first dose as MMRV have • Can lead to deafness, meningitis (infection of the brain had more fevers and fever-related seizures (about and spinal cord covering), infection of the pancreas, 1 in 1,250) than children who got the first dose as painful swelling of the testicles or ovaries, and, rarely, separate shots of MMR and varicella vaccines on death. the same day (about 1 in 2,500). Rubella (German Measles) Your doctor can give you more information, • Causes rash and mild fever; and can cause arthritis, including the Vaccine Information Statements for (mostly in women). MMR and Varicella vaccines. -

(ACIP) General Best Guidance for Immunization
8. Altered Immunocompetence Updates This section incorporates general content from the Infectious Diseases Society of America policy statement, 2013 IDSA Clinical Practice Guideline for Vaccination of the Immunocompromised Host (1), to which CDC provided input in November 2011. The evidence supporting this guidance is based on expert opinion and arrived at by consensus. General Principles Altered immunocompetence, a term often used synonymously with immunosuppression, immunodeficiency, and immunocompromise, can be classified as primary or secondary. Primary immunodeficiencies generally are inherited and include conditions defined by an inherent absence or quantitative deficiency of cellular, humoral, or both components that provide immunity. Examples include congenital immunodeficiency diseases such as X- linked agammaglobulinemia, SCID, and chronic granulomatous disease. Secondary immunodeficiency is acquired and is defined by loss or qualitative deficiency in cellular or humoral immune components that occurs as a result of a disease process or its therapy. Examples of secondary immunodeficiency include HIV infection, hematopoietic malignancies, treatment with radiation, and treatment with immunosuppressive drugs. The degree to which immunosuppressive drugs cause clinically significant immunodeficiency generally is dose related and varies by drug. Primary and secondary immunodeficiencies might include a combination of deficits in both cellular and humoral immunity. Certain conditions like asplenia and chronic renal disease also can cause altered immunocompetence. Determination of altered immunocompetence is important to the vaccine provider because incidence or severity of some vaccine-preventable diseases is higher in persons with altered immunocompetence; therefore, certain vaccines (e.g., inactivated influenza vaccine, pneumococcal vaccines) are recommended specifically for persons with these diseases (2,3). Administration of live vaccines might need to be deferred until immune function has improved. -

Candidate Rotavirus Vaccine Recommendations for Consideration by the WHO Strategic Advisory Group of Experts (SAGE) on Immunization
Candidate rotavirus vaccine recommendations for consideration by the WHO Strategic Advisory Group of Experts (SAGE) on Immunization 1. Overall recommendation WHO strongly recommends the inclusion of rotavirus vaccination into the national immunization programmes of all regions of the world. In particular, countries where deaths among children due to diarrhoeal diseases account for ≥10% of under-5 mortality rate should prioritize the introduction of rotavirus vaccination. Countries where deaths among children due to diarrhoeal diseases account for <10% of under-5 mortality rate should also consider the introduction of rotavirus vaccination based on anticipated reduction in mortality and morbidity from diarrhoea, savings in health care costs, and the cost-effectiveness of vaccination. Justification: Rotavirus is a major cause of mortality in countries with high diarrhoeal disease mortality among children under five years of age. Every year, rotavirus gastroenteritis is estimated to cause approximately 527,000 (475,000-580,000) deaths globally among children <5 years old. Most of these deaths occur in developing countries and 90% of the rotavirus- associated fatalities occur in Africa and Asia alone. Globally, >2 million children are hospitalized each year for rotavirus infections. In a recent report of sentinel hospital-based rotavirus surveillance from 35 nations representing each of the six WHO regions between 2001 and 2008, an average of 40% (range= 34%-45%) of hospitalizations for diarrhea among children < 5 years old were attributable to rotavirus infection. 2. Detailed recommendation: Extrapolating efficacy data from a rotavirus vaccine study performed in one population to use of same rotavirus vaccine in other populations Efficacy/effectiveness data from a rotavirus vaccine study performed in a population from one of three under-5 mortality rate categories* can be extrapolated for use in populations in the same under-5 mortality rate category. -

Rotavirus Vaccine: Questions and Answers for Health Care Providers
Rotavirus Vaccine Questions and Answers for Health Care Providers In April 2014, Manitoba Health, Seniors and Active Living launched a publicly-funded Rotavirus Immunization Program for infants born on or after March 1, 2014. In 2018, Manitoba, along with the rest of Canada, switched from RotarixTM to RotaTeq®. As of May 15, 2021, Manitoba has switched back to Rotarix®, for use in its publicly-funded Rotavirus Immunization Program, for infants born on or after April 1, 2021. This document includes an updated list of questions and answers for your reference. 1. Why is there a Rotavirus Immunization Program in Manitoba? 2. Who qualifies for publicly-funded rotavirus vaccine? 3. Which rotavirus vaccine does Manitoba use? 4. Why does the vaccine series need to be completed before eight months of age? 5. How is Rotarix® packaged? 6. How are the oral tube and cap disposed of after use? 7. Should a spit-up dose of vaccine be repeated? 8. Are there any precautions that health care providers should take when administering the oral rotavirus vaccine? 9. Oral rotavirus vaccine contains sucrose in an amount expected to have an effect on immunization injection pain. When should Rotarix® be given in relation to other vaccines to elicit a reduction in pain? 10. How do I administer Rotarix®? 11. Is additional screening for potential contraindications required prior to administering rotavirus vaccine? 12. Can infants born to mothers on immunosuppressive medication be immunized? 13. Are there any issues related to circulating maternal antibodies interfering with the response to the live attenuated vaccine? 14. Are the two rotavirus vaccines, RotaTeq® and Rotarix™, interchangeable? 15. -

Case Studies Controversies in Vaccination
European Review, Vol. 21, No. S1, S56–S61 r 2013 Academia Europæa. The online version of this article is published within an Open Access environment subject to the conditions of the Creative Commons Attribution license ,http://creativecommons.org/licenses/by/3.0/.. doi:10.1017/S1062798713000227 Session 3 – Case Studies Controversies in Vaccination ROMAN PRYMULA University Hospital Hradec Kralove, Sokolska 581, 500 05 Hradec Kralove, Czech Republic. E-mail: [email protected] Infectious diseases still jeopardize human health and even lives. In spite of the variety of advanced treatment methods, prevention is considered to be the most effective way to fight infections, and vaccination, no doubt, is one of the most effective preventive measures in the history of mankind. The vaccine controversy is based on a dispute over morality, ethics, effectiveness, and/or safety. There is no 100% safe or effective vaccine; however, benefits clearly overweigh risks. Ironically, as the numbers of cases of vaccine- preventable infectious diseases are falling, the controversies relating to vaccine safety are growing. Vaccines are generally victims of their own success. Controversies can afflict the positive acceptance of immunization, decrease the coverage and uptake and finally threaten the health of children and adults. The advent of vaccination has proven to be one of the most effective preventive measures in the history of medicine. Vaccines play a significant role in the prevention of debili- tating and, in many cases, life-threatening infectious diseases. Vaccines also provide important benefits in terms of reducing or avoiding costs associated with illness, both direct and indirect. In spite of the absence of any kind of ideal global healthcare system and lack of resources, the World Health Organisation (WHO) and the United Nations Children’s Fund (UNICEF) were able, in 1974, to establish a major global project called the Expanded Programme on Immunization (EPI). -

Polio Vaccine May Be Given at the Same Time As Other Paralysis (Can’T Move Arm Or Leg)
POLIO VVPOLIO AAACCINECCINECCINE (_________ W H A T Y O U N E E D T O K N O W ) (_I111 ________What is polio? ) (_I ________Who should get polio ) 333 vaccine and when? Polio is a disease caused by a virus. It enters a child’s (or adult’s) body through the mouth. Sometimes it does IPV is a shot, given in the leg or arm, depending on age. not cause serious illness. But sometimes it causes Polio vaccine may be given at the same time as other paralysis (can’t move arm or leg). It can kill people who vaccines. get it, usually by paralyzing the muscles that help them Children breathe. Most people should get polio vaccine when they are Polio used to be very common in the United States. It children. Children get 4 doses of IPV, at these ages: paralyzed and killed thousands of people a year before we 333 A dose at 2 months 333 A dose at 6-18 months had a vaccine for it. 333 A dose at 4 months 333 A booster dose at 4-6 years 222 Why get vaccinated? ) Adults c I Most adults do not need polio vaccine because they were Inactivated Polio Vaccine (IPV) can prevent polio. already vaccinated as children. But three groups of adults are at higher risk and should consider polio vaccination: History: A 1916 polio epidemic in the United States killed (1) people traveling to areas of the world where polio is 6,000 people and paralyzed 27,000 more. In the early common, 1950’s there were more than 20,000 cases of polio each (2) laboratory workers who might handle polio virus, and year. -

Vaccine Information for PARENTS and CAREGIVERS
NATIONAL INSTITUTE FOR COMMUNICABLE DISEASES Division of the National Health Laboratory Service VACCINE INFOR MATION FOR PARENTS & CAREGIVERS First Edition November 2016 Editors-in-Chief Nkengafac Villyen Motaze (MD, MSc, PhD fellow), Melinda Suchard (MBBCh, FCPath (SA), MMed) Edited by: Cheryl Cohen, (MBBCh, FCPath (SA) Micro, DTM&H, MSc (Epi), Phd) Lee Baker, (Dip Pharm) Lucille Blumberg, (MBBCh, MMed (Micro) ID (SA) FFTM (RCPS, Glasgow) DTM&H DOH DCH) Published by: Ideas Wise and Wonderful (IWW) for National Institute for Communicable Diseases (NICD) First Edition: Copyright © 2016 Contributions by: Clement Adu-Gyamfi (BSc Hons, MSc), Jayendrie Thaver (BSc), Kerrigan McCarthy, (MBBCh, FCPath (SA), DTM&H, MPhil (Theol) Kirsten Redman (BSc Hons), Nishi Prabdial-Sing (PhD), Nonhlanhla Mbenenge (MBBCh, MMED) Philippa Hime (midwife), Vania Duxbury (BSc Hons), Wayne Howard (BSc Hons) Acknowledgments: Amayeza, Vaccine Information Centre (http://www.amayeza-info.co.za/) Centre for Communicable Diseases Fact Sheets (http://www.cdc.gov/vaccines/hcp/vis/) World Health Organization Fact Sheets (http://www.who.int/mediacentre/factsheets/en/) National Department of Health, South Africa (http://www.health.gov.za/) Disclaimer This book is intended as an educational tool only. Information may be subject to change as schedules or formulations are updated. Summarized and simplified information is presented in this booklet. For full prescribing information and contraindications for vaccinations, please consult individual package inserts. There has been -

Swine Flu and Polio Vaccines: Some Parallels and Some Differences
Swine Fluand Polio Vaccines: Some Parallelsand Some Differences Howard B. Baumel College of Staten Island of the City Universityof New York Staten Island 10301 The swine flu vaccinationprogram vaccine could be successfullydevel- facturedby a single pharmaceutical generated debate in scientific and oped. company.The cause of this outbreak medical circlesthat extended to the Salkrelied heavily on his previous was never clearly established. Be- Downloaded from http://online.ucpress.edu/abt/article-pdf/39/9/550/36038/4446085.pdf by guest on 29 September 2021 general public.The controversythat experience as he attemptedto pro- cause bottles of tissue culture fluid centered on the vaccine's effective- duce a killedvirus polio vaccine.He containingthe virushad been stored ness and safety was reminiscentof used formalinto kill the virus and priorto being treated with formalin, the problemsthat accompaniedthe isolated one strain for each of the it was possiblethat bits of tissue had development of the polio vaccine three knowntypes of polio virus.To settled to the bottom covering the years ago. A review of that earlier determineif any live virusremained viruses and protecting them from scientific achievement can provide after the exposure to formalin,the the formalin.To prevent this, the insightsinto the swineflu dilemma. treated virus was injected into the tissue culture fluid was filtered to By the mid-1930's,only threeviral brain of a monkey. If the monkey remove the debris before exposure diseases,smallpox, rabies, and yellow contracted polio, it was concluded to formalin. fever, had yielded to vaccines. In that live viruswas present.To deter- HeraldCox and HilaryKoprowski each of these cases, the vaccine mine if the treated virus was effec- (1955, 1956) had developed an consisted of a live virus. -

Polio Fact Sheet
Polio Fact Sheet 1. What is Polio? - Polio is a disease caused by a virus that lives in the human throat and intestinal tract. It is spread by exposure to infected human stool: e.g. from poor sanitation practices. The 1952 Polio epidemic was the worst outbreak in the nation's history. Of nearly 58,000 cases reported that year, 3,145 people died and 21,269 were left with mild to disabling paralysis, with most of the victims being children. The "public reaction was to a plague", said historian William O'Neill. "Citizens of urban areas were to be terrified every summer when this frightful visitor returned.” A Polio vaccine first became available in 1955. 2. What are the symptoms of Polio? - Up to 95 % of people infected with Polio virus are not aware they are infected, but can still transmit it to others. While some develop just a fever, sore throat, upset stomach, and/or flu-like symptoms and have no paralysis or other serious symptoms, others get a stiffness of the back or legs, and experience increased sensitivity. However, a few develop life-threatening paralysis of muscles. The risk of developing serious symptoms increases with the age of the ill person. 3. Is Polio still a disease seen in the United States? - The last naturally occurring cases of Polio in the United States were in 1979, when an outbreak occurred among the Amish in several states including Pennsylvania. 4. What kinds of Polio vaccines are used in the United States? - There is now only one kind of Polio vaccine used in the United States: the Inactivated Polio vaccine (IPV) is given as an injection (shot). -

Pink Book Webinar Series: Rotavirus and Hepatitis a Slides
Centers for Disease Control and Prevention National Center for Immunization and Respiratory Diseases Rotavirus and Hepatitis A Pink Book Webinar Series 2018 Mark Freedman, DVM, MPH Veterinary Medical Officer Photographs and images included in this presentation are licensed solely for CDC/NCIRD online and presentation use. No rights are implied or extended for use in printing or any use by other CDC CIOs or any external audiences. Rotavirus: Disease and Vaccine Rotavirus . First identified as a cause of diarrhea in 1973 . Most common cause of severe gastroenteritis in infants and young children . Nearly universal infection by age 5 years . Responsible for up to 500,000 diarrheal deaths each year worldwide Rotavirus . Two important outer shell proteins—VP7, or G-protein, and VP4, or P-protein define the serotype of the virus . From 1996–2005, five predominate strains in the U.S. (G1–G4, G9) accounted for 90% of the isolates . G1 strain accounts for 75% of infections . Very stable and may remain viable for weeks or months if not disinfected Rotavirus Immunity . Antibody against VP7 and VP4 probably important for protection • Cell-mediated immunity probably plays a role in recovery and immunity . First infection usually does not lead to permanent immunity . Reinfection can occur at any age . Subsequent infections generally less severe Rotavirus Clinical Features . Short incubation period . First infection after 3 months of age generally most severe . May be asymptomatic or result in severe, dehydrating diarrhea with fever and vomiting . Gastrointestinal symptoms generally resolve in 3–7 days Rotavirus Complications . Infection can lead to severe diarrhea, dehydration, electrolyte imbalance, and metabolic acidosis . -
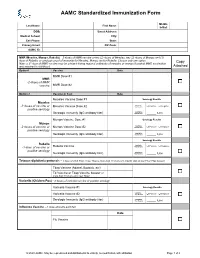
AAMC Standardized Immunization Form
AAMC Standardized Immunization Form Middle Last Name: First Name: Initial: DOB: Street Address: Medical School: City: Cell Phone: State: Primary Email: ZIP Code: AAMC ID: MMR (Measles, Mumps, Rubella) – 2 doses of MMR vaccine or two (2) doses of Measles, two (2) doses of Mumps and (1) dose of Rubella; or serologic proof of immunity for Measles, Mumps and/or Rubella. Choose only one option. Copy Note: a 3rd dose of MMR vaccine may be advised during regional outbreaks of measles or mumps if original MMR vaccination was received in childhood. Attached Option1 Vaccine Date MMR Dose #1 MMR -2 doses of MMR vaccine MMR Dose #2 Option 2 Vaccine or Test Date Measles Vaccine Dose #1 Serology Results Measles Qualitative -2 doses of vaccine or Measles Vaccine Dose #2 Titer Results: Positive Negative positive serology Quantitative Serologic Immunity (IgG antibody titer) Titer Results: _____ IU/ml Mumps Vaccine Dose #1 Serology Results Mumps Qualitative -2 doses of vaccine or Mumps Vaccine Dose #2 Titer Results: Positive Negative positive serology Quantitative Serologic Immunity (IgG antibody titer) Titer Results: _____ IU/ml Serology Results Rubella Qualitative Positive Negative -1 dose of vaccine or Rubella Vaccine Titer Results: positive serology Quantitative Serologic Immunity (IgG antibody titer) Titer Results: _____ IU/ml Tetanus-diphtheria-pertussis – 1 dose of adult Tdap; if last Tdap is more than 10 years old, provide date of last Td or Tdap booster Tdap Vaccine (Adacel, Boostrix, etc) Td Vaccine or Tdap Vaccine booster (if more than 10 years since last Tdap) Varicella (Chicken Pox) - 2 doses of varicella vaccine or positive serology Varicella Vaccine #1 Serology Results Qualitative Varicella Vaccine #2 Titer Results: Positive Negative Serologic Immunity (IgG antibody titer) Quantitative Titer Results: _____ IU/ml Influenza Vaccine --1 dose annually each fall Date Flu Vaccine © 2020 AAMC.