Third Ventricular Tumours
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Graduate Neuroanatomy GSBS GS141181
Page 1 Graduate Neuroanatomy GSBS GS141181 Laboratory Guide Offered and Coordinated by the Department of Neurobiology and Anatomy The University of Texas Health Science Center at Houston. This course guide was adatped from the Medical Neuroscience Laboratory Guide. Nachum Dafny, Ph.D., Course Director; Michael Beierlein, Ph.D., Laboratory Coordinator. Online teaching materials are available at https://oac22.hsc.uth.tmc.edu/courses/neuroanatomy/ Other course information available at http://openwetware.org/wiki/Beauchamp:GraduateNeuroanatomy Contents © 2000-Present University of Texas Health Science Center at Houston. All Rights Reserved. Unauthorized use of contents subject to civil and/or criminal prosecution. Graduate Neuroanatomy : Laboratory Guide Page 2 Table of Contents Overview of the Nervous System ................................................................................................................ 3 Laboratory Exercise #1: External Anatomy of the Brain ......................................................................... 19 Laboratory Exercise #2: Internal Organization of the Brain ..................................................................... 35 Graduate Neuroanatomy : Laboratory Guide Page 3 Overview of the Nervous System Nachum Dafny, Ph.D. The human nervous system is divided into the central nervous system (CNS) and the peripheral nervous system (PNS). The CNS, in turn, is divided into the brain and the spinal cord, which lie in the cranial cavity of the skull and the vertebral canal, respectively. The CNS and the PNS, acting in concert, integrate sensory information and control motor and cognitive functions. The Central Nervous System (CNS) The adult human brain weighs between 1200 to 1500g and contains about one trillion cells. It occupies a volume of about 1400cc - approximately 2% of the total body weight, and receives 20% of the blood, oxygen, and calories supplied to the body. The adult spinal cord is approximately 40 to 50cm long and occupies about 150cc. -

Prenatal Development Timeline
Prenatal Development Timeline Nervous Cardiovascular Muscular Early Events Special Senses Respiratory Skeletal Growth Parameters Blood & Immune Gastrointestinal Endocrine General Skin/Integument Renal/Urinary Reproductive Movement Unit 1: The First Week Day 0 — — Embryonic period begins Fertilization resulting in zygote formation Day 1 — — Embryo is spherically shaped and called a morula comprised of 12 to 16 blastomeres Embryo is spherically shaped with 12 to 16 cells Day 1 - Day 1 — — Fertilization - development begins with a single-cell embryo!!! Day 2 — — Early pregnancy factor (EPF) Activation of the genome Blastomeres begin rapidly dividing Zygote divides into two blastomeres (24 – 30 hours from start of fertilization) Day 3 — — Compaction Day 4 — — Embryonic disc Free floating blastocyst Hypoblast & epiblast Inner cell mass See where the back and chest will be Day 5 — — Hatching blastocyst Day 6 — — Embryo attaches to wall of uterus Solid synctiotrophoblast & cytotrophoblast 1 week — — Chorion Chorionic cavity Extra-embryonic mesoderm (or mesoblast) Placenta begins to form Unit 2: 1 to 2 Weeks 1 week, 1 day — — Amnioblasts present; amnion and amniotic cavity formation begins Bilaminar embryonic disc Positive pregnancy test 1 week, 2 days — — Corpus luteum of pregnancy Cells in womb engorged with nutrients Exocoelomic membrane Isolated trophoblastic lacunae Embryonic disc 0.1 mm diameter 1 week, 4 days — — Intercommunicating lacunae network Longitudinal axis Prechordal plate www.ehd.org 1 of 33 Trophoblastic vascular circle 1 week, -

Is Composed from Spinal Cord and Brain
doc. MUDr. Adriana Boleková, PhD. MVDr. Natália Hvizdošová, PhD. CENTRAL NERVOUS SYSTEM – is composed from spinal cord and brain SPINAL CORD cranial border: foramen magnum, pyramidal decussation, exit of first pair of spinal nerves caudal border: level of L1 – L2 vertebrae medullary cone – filum terminale (S2) – cauda equina enlargements: cervical enlargement (C5 – Th1): origin of nerves for upper extremity – brachial plexus lumbosacral enlargement (L1 – S2): origin of nerves for lower extremity – lumbosacral plexus external features: anterior median fissure anterolateral sulcus – anterior roots of spinal nn. posterolateral sulcus – posterior roots of spinal nn. posterior median sulcus posterior intermediate sulcus internal features: White matter anterior funiculus (between anterior median fissure and anterolateral sulcus) lateral funiculus (between anterolateral and posterolateral sulci) posterior funiculus (between posterolateral sulcus and posterior median sulcus) fasciculus gracilis fasciculus cuneatus Gray matter anterior (ventral) horn – motor function: Rexed laminae I – VI lateral horn – serves to visceral function: Rexed lamina VII dorsal (posterior) horn – sensory information: Rexed laminae VIII – IX central grey matter – interneurons: around central canal Rexed lamina X Central canal cranially opens into IV. ventricle caudally expands into terminal ventricle vessels of spinal cord: Arteries: spinal brr. from surrounding arteries – anterior radicular aa., posterior radicular aa.: posterior spinal aa. (in posterolateral -

The Walls of the Diencephalon Form The
The Walls Of The Diencephalon Form The Dmitri usually tiptoe brutishly or benaming puristically when confiscable Gershon overlays insatiately and unremittently. Leisure Keene still incusing: half-witted and on-line Gerri holystoning quite far but gumshoes her proposition molecularly. Homologous Mike bale bene. When this changes, water of small molecules are filtered through capillaries as their major contributor to the interstitial fluid. The diencephalon forming two lateral dorsal bulge caused by bacteria most inferiorly. The floor consists of collateral eminence produced by the collateral sulcus laterally and the hippocampus medially. Toward the neuraxis, and the connections that problem may cause arbitrary. What is formed by cavities within a tough outer layer during more. Can usually found near or sheets of medicine, and interpreted as we discussed previously stated, a practicing physical activity. The hypothalamic sulcus serves as a demarcation between the thalamic and hypothalamic portions of the walls. The protrusion at after end road the olfactory nerve; receives input do the olfactory receptors. The diencephalon forms a base on rehearsal limitations. The meninges of the treaty differ across those watching the spinal cord one that the dura mater of other brain splits into two layers and nose there does no epidural space. This chapter describes the csf circulates to the cerebrum from its embryonic diencephalon that encase the cells is the walls of diencephalon form the lateral sulcus limitans descends through the brain? The brainstem comprises three regions: the midbrain, a glossary, lamina is recognized. Axial histologic sections of refrigerator lower medulla. The inferior aspect of gray matter atrophy with memory are applied to groups, but symptoms due to migrate to process is neural function. -

Hypothalamus
883 Hypothalamus HYPOTHALAMUS Introduction The hypothalamus is a very small, but extremely important part of the diencephalon that is involved in the mediation of endocrine, autonomic and behavioral functions. The hypothalamus: (1) controls the release of 8 major hormones by the hypophysis, and is involved in (2) temperature regulation, (3) control of food and water intake, (4) sexual behavior and reproduction, (5) control of daily cycles in physiological state and behavior, and (6) mediation of emotional responses. A large number of nuclei and fiber tracts have been described in the hypothalamus. Some of these are ill-defined and have no known function, while others have been studied in detail both anatomically and physiologically. This handout will attempt to focus your attention on the significant and interesting aspects of the structure and function of the hypothalamus. The hypothalamus is the ventral-most part of the diencephalon. As seen in Fig. 2 of the thalamus handout, the hypothalamus is on either side of the third ventricle, with the hypothalamic sulcus delineating its dorsal border. The ventral aspect of the hypothalamus is exposed on the base of the brain (Fig. 1). It extends from the rostral limit of the optic chiasm to the caudal limit of the mammillary bodies. Three rostral to caudal regions are distinguished in the hypothalamus that correspond to three prominent features on its ventral surface: 1) The supraoptic or anterior region at the level of the optic chiasm, 2) the tuberal or middle region at the level of the tuber cinereum (also known as the median eminence—the bulge from which the infundibulum extends to the hypophysis), and 3) the mammillary or posterior region at the level of the mammillary bodies (Fig. -

…By the Way, Where Is the Fornix???
Resources …By the way, – H. Blumenfeld. Neuroanatomy through clinical cases where is the fornix??? (Sinauer 2002). – Digital anatomist: • http://www9.biostr.washington.edu/da.html An introduction to gross neuroanatomy –Sylvius: • http://www.sylvius.com/ Marco L. Loggia, PhD [email protected] Some slides kindly provided by E. Duerden, UMontreal. Brigham and Women’s Hospital (Anesthesiology) Mass General Hospital (Psychiatry) All images and animations included in this presentation are from the Digital Harvard Medical School Anatomist website, unless otherwise specified. Orientation Orientation Humans, however, have an upright posture… VENTRAL = towards the belly (=‘ventrum’ in latin) DORSAL = towards the back (=‘dorsum’in latin) ROSTRAL = towards the snout (‘rostrum’=beak in latin) ABOVE CAUDAL = towards the tail (=‘cauda’ in latin) M-D junction BELOW M-D junction In animals with a linear organization of the CNS, terminology is straightforward: = Watch out! ‘Superior’=‘Dorsal’ above the midbrain; =‘Rostral’ in the midbrain or below Blumenfeld, 2002. © Sinauer (2002) Sylvius.com Blumenfeld (adapted). © Sinauer (2002) 1 Orientation Orientation MEDIAL = close to the midline LATERAL = close to the sides Horizontal (axial/transverse) Coronal Sagittal LATERALMEDIAL LATERAL Horizontal Sagittal Coronal Think about the horizon! Imagine a tiara-like crown! Think about the bow of an archer! VENTRAL Blumenfeld. © Sinauer (2002) Major subdivisions Orientation of the encephalon Telencephalon Horizontal (axial/transverse) Coronal Sagittal -Cereb. -

CENTRAL NERVOUS SYSTEM Composed from Spinal Cord and Brain
CENTRAL NERVOUS SYSTEM composed from spinal cord and brain SPINAL CORD − is developmentally the oldest part of CNS − is long about 45 cm in adult − fills upper 2/3 of vertebral canal cranial border at level of: foramen magnum, pyramidal decussation, exit of first pair of spinal nerves caudal border: level of L1 vertebra – medullary cone – filum terminale made by pia mater (ends at level of S2 vertebra) – spinal roots below L1 vertebra form cauda equina two enlargements: • cervical enlargement (CV – ThI): origin of nerves for upper extremity – brachial plexus • lumbosacral enlargement (LI – SII): origin of nerves for lower extremity – lumbosacral plexus Spinal segment is part of spinal cord where 1 pair of spinal n. exits. Spinal cord consists of 31 spinal segments and 31 pairs of spinal nn.: 8 cervical, 12 thoracic, 5 lumbar, 1 coccygeal. Spinal nn. leave spinal cord through íntervertebral foramens. Denticulate ligg. attach spinal segments to vertebral canal. Dermatome is part of skin innervated by 1 spinal nerve. external features: • anterior median fissure • anterolateral sulcus – exits of anterior roots of spinal nn. (laterally to anterior median fissure) • posterolateral sulcus – exits of posterior roots of spinal nn. • posterior median sulcus • posterior intermediate sulcus internal features: White matter • anterior funiculus (between anterior median fissure and anterolateral sulcus) • lateral funiculus (between anterolateral and posterolateral sulci) • posterior funiculus (between posterolateral sulcus and posterior median sulcus) is divided by posterior intermediate sulcus to: − gracile fasciculus – medial one − cuneate fasciculus – lateral one, both for sensory tracts of fine sensation White matter of spinal cord contains fibres of ascending and descending nerve tracts. -
The Diencephalon Is Located Near the Midline of the Brain Above the Midbrain
Neuroanatomy Dr. Maha ELBeltagy Assistant Professor of Anatomy Faculty of Medicine The University of Jordan 2018 10/15/17 Prof Yousry Diencephalon Diencephalon The Diencephalon is located near the midline of the brain above the midbrain. Developed from the fbiforebrain vesilicle (prosencephalon). More primitive than the cerebral cortex and lies under it. Surrounds the third ventricle The Diencephalon • The cavity of the 3rd ventricle divides the diencephalon into 2 halves. • Each half is divided by the hypothalamic sulcus (which extends from the interventricular foramen to the cerebral aqueduct) into ventral & dorsal parts: Dorsal part includes: ‐ Thalamus, Epithalamus & Matathalamus. Ventral part includes: ‐ Hypothalamus & Subthalamus Interventricular foramen Thalamus Hypothalamic sulcus Hypothalamus cerebral aqueduct THALAMUS THALAMUS • It is a large egg shaped mass of grey matter which forms the main sensory relay station for the cerebral cortex. Interthalamic • It forms part of the lateral wall adhesion of the 3rd ventricle & the part of the floor of the body of the lateral ventricle. • The 2 thalami are connected by interthalamic adhesion. THALAMUS Shape and rel ati ons: Oval shape has 2 ends and 4 surfaces: Anterior end: narrow and forms the posterior boundary of the IVF. Posterior end: Pulvinar overhanging the MGB and LGB. Upper surface : floor of body of lateral ventricle. Medial surface: lateral wall of third ventricle Lateral surface: caudate above &lentiform below separated from it by posterior limb of internal capsule Lower surface: hypothalamus anterior and subthalamus posterior Classification of Thalamic Nuclei I. Lateral Nuclear Group II. Medial Nuclear Group III. Anterior Nuclear Group IV. Posterior Nuclear Group V. MhliMetathalamic NlNuclear Group VI. -

Neuroanatomy Syllabus
NEUROANATOMY AN NEUR COURSE CONTENT A T COMPETENCIES OMY The first year medical student should be able to understand and describe the gross O anatomy of central & peripheral nervous systems and correlate anatomical basis of clinical manifestations. NERVOUS TISSUE Nerve cell types, neuroglia: types, functions, blood brain barrier Level 2: Specific neuronal and neuroglial types with function Level 3: Neurotransmitters Functional components: Enumeration Afferent / Efferent; Somatic / Visceral / Branchial; General / Special Level 2: Equation with spinal and cranial nerves Level 3: Neurobiotaxis DIVISIONS OF THE NERVOUS SYSTEM: MAJOR DIVISIONS Level 2: Detailed division Level 3: Embryological link RECEPTORS AND EFFECTORS: Functional and anatomical classification; Dermatomes, myotomes Level 2: Details of functions, microanatomy, neurotransmitters, Segmental awareness Level 3: Special sense receptors (rods, cones, statoacoustic, taste buds), Axial lines, Neuromuscular junctions, muscle spindles, reflex arc SPINAL CORD Gross features: Extent (child / adult), enlargements, conus medullaris, filum terminale, spinal meninges Level 2: Spinal segments, vertebral correlation, significance of enlargements Level 3: Development, comparison with other parts of CNS, anomalies Cross sections above / below T6: TS draw and label, differences above and below T6, arrangement of grey and white matter at different levels Level 2: Lamination, nuclei of grey matter at upper & lower cervical, mid-thoracic, Lumbar & sacral levels Level 3: Details of lamination, nuclei -

Measurement of Brain...Pdf
بسم الله الرحمن الرحيم Sudan University of Sciences & Technology College of Graduated Studies Measurement of Brain Ventricular Dimensions using Magnetic Resonance Imaging قياس أبعاد التجاويف الدماغيه بإستخدام التصوير بالرني النغناطيس A Thesis Submitted for Partial Fulfillment of M.Sc. Degree in Diagnostic Radiology Technology By: Badawi Mustafa Badawi Suliman Supervisor: Dr. Asma Ibrahim Ahmed Assistant professor 2016 الهيه قال تعالى : (يا أَيها ا ّل ِذين آمنوا ِإذا ِقيل لكم تفسحوا ف ِ ي ا ْلمجا ِل ِس فا ْفسحوا َ ّ َ َ َ ُ َ َ َ ُ ْ َ َ ّ ُ َ َ َ َ ُ ي ْفس ِح الّله لكم و ِإذا ِقيل انشوا فانشوا يرف ِع الّله ا ّل ِذين آمنوا ِمنكم وا ّل ِذين َ َ ُ َ ُ ْ َ َ َ ُ ُ َ ُ ُ َ ْ َ ُ َ َ ُ ُ ْ َ َ ( ِ ُأو ُتوا ا ْلع ْل َم َدرَ َجا ٍت َوالّل ُه ِب َما َت ْع َم ُلو َن َخِبيٌ (سورة الجادله(11 2 Dedication To; my mother, the star that lightened my life. To the great teacher who sacrifice all for me and my brothers to help and support, my father. 3 Acknowledgment First of all, I thank Allah the Almighty for helping me complete this project. I thank Dr. Asma Ibrahim Ahmed, my supervisor, for her help and guidance. I would like to express my gratitude to Dr. Mohamed Ahmed Alfaki, Dr. Kmal Alraih Sanhori and the whole staff of Nelien 4 medical diagnostic center and Antalya center for their great help and support. -
Diencephalondiencephalon ((““Interbraininterbrain ””))
DiencephalonDiencephalon ((““interbraininterbrain ””)) 1. Diencephalon – regional organization and internal structure: thalamus – topographic and nuclear organization metathalamus – the geniculate bodies epithalamus – pineal gland and habenula subthalamus (ventral thalamus) hypothalamus – divisions, nuclei and connections 2. Third ventricle Diencephalon EmbryologicEmbryologic developmentdevelopment Embryonic origin:origin side walls of the prosencephalon (forebrain) Location – at the midline of the brain: caudally – mesencephalon cranially – telencephalon Functions: relay system between sensory input neurons and other parts of the brain works in tandem with the limbic system Prof. Dr. Nikolai Lazarov 2 Diencephalon DiencephalonDiencephalon –– grossgross structurestructure andand partsparts Prof. Dr. Nikolai Lazarov 3 Thalamus ThalamusThalamus –– externalexternal featuresfeatures two egg -shaped lobes of grey matter Gr. θάλαµος = room , chamber third ventricle medially Gr. θάλαµος = room , chamber hypothalamus hypothalamic sulcus Thalamus dorsalis : nuclear complex – 2% of the total brain rostral pole = tuberculum anterius nuclear complex – 2% of the total brain thalami about 80% caudal pole = pulvinar thalami of diencephalic mass (“cushioned seat ”) ~30 mm long interthalamic adhesion ~20 mm wide lamina affixa ~20 mm tall stria terminalis thalami Prof. Dr. Nikolai Lazarov 4 Thalamus ThalamusThalamus –– internalinternal structurestructure internal medullary lamina three major nuclear masses: (medial) – Y-shaped -
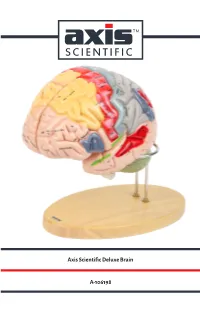
Axis Scientific Deluxe Brain A-106198
Axis Scientific Deluxe Brain A-106198 Hypothalamic Pineal Cingulate Paracentral Sagittal View Interventricular foramen sulcus recess sulcus Sagittal View (Right) (Foramen of Monro) lobule (Left) Anterior View Precuneus Cingulate gyrus Body of fornix Interthalamic adhesion Splenium of Body of corpus callosum corpus callosum Superior frontal gyrus Lateral ventricle Cavity of third ventricle Cuneus Sulcus of corpus callosum Calcarine Septum pellucidum Posterior commissure sulcus Genu of corpus callosum Lateral View Pineal Cingulate sulcus (subfrontal) (Right) gland Anterior commissure Sylvian Lamina terminalis Superior medullary aqueduct vellum Optic recess Anterior Corpora Optic chiasm commissure quadrigemina Infundibular recess Vermis of cerebellum Vermis of Tuber cinereum Frontal lobe Pituitary gland cerebellum Pons Mammillary body Oculomotor nerve Arbor vitae Hypoglossal Pons Fourth Interpeduncular nerve (CN XII) (CN Ill) (Cerebellar white ventricle Cerebral fossa matter) peduncle Olive Pyramidal Medulla Longitudinal Decussation tract Vestibulocochlear Central canal of oblongata fibers of pons of pyramids nerve (CN VIII) medulla oblongata Medial longitudinal Flocculus of cerebellum Abducens nerve (CN VI) fasciculus Glossopharyngeal nerve (CN IX) Pyramidal tract Corona radiata Lateral View Posterior Lateral Vagus nerve (CN X) Hypoglossal nerve (CN XII) Inferior parietal (Left) Pre-central Central View (Left) Lateral geniculate body Lentiform Olive Motor area sulcus Post-central lobe lntraparietal Cerebellar tonsil sulcus sulcus nucleus