Diagnostic Performance of Gadoxetic Acid
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

List of Union Reference Dates A
Active substance name (INN) EU DLP BfArM / BAH DLP yearly PSUR 6-month-PSUR yearly PSUR bis DLP (List of Union PSUR Submission Reference Dates and Frequency (List of Union Frequency of Reference Dates and submission of Periodic Frequency of submission of Safety Update Reports, Periodic Safety Update 30 Nov. 2012) Reports, 30 Nov. -

Pharmacologyonline 2: 727-753 (2010) Ewsletter Bradu and Rossini
Pharmacologyonline 2: 727-753 (2010) ewsletter Bradu and Rossini COTRAST AGETS - IODIATED PRODUCTS. SECOD WHO-ITA / ITA-OMS 2010 COTRIBUTIO O AGGREGATE WHO SYSTEM-ORGA CLASS DISORDERS AD/OR CLUSTERIG BASED O REPORTED ADVERSE REACTIOS/EVETS Dan Bradu and Luigi Rossini* Servizio Nazionale Collaborativo WHO-ITA / ITA-OMS, Università Politecnica delle Marche e Progetto di Farmacotossicovigilanza, Azienda Ospedaliera Universitaria Ospedali Riuniti di Ancona, Regione Marche, Italia Summary From the 2010 total basic adverse reactions and events collected as ADRs preferred names in the WHO-Uppsala Drug Monitoring Programme, subdivided in its first two twenty years periods as for the first seven iodinated products diagnostic contrast agents amidotrizoate, iodamide, iotalamate, iodoxamate, ioxaglate, iohexsol and iopamidol, their 30 WHO-system organ class disorders (SOCDs) aggregates had been compared. Their common maximum 97% levels identified six SOCDs only, apt to evaluate the most frequent single ADRs for each class, and their percentual normalization profiles for each product. The WILKS's chi square statistics for the related contingency tables, and Gabriel’s STP procedure applied to the extracted double data sets then produced profile binary clustering, as well as Euclidean confirmatory plots. They finally showed similar objectively evaluated autoclassificative trends of these products, which do not completely correspond to their actual ATC V08A A, B and C subdivision: while amidotrizoate and iotalamate, and respectively iohesol and iopamidol are confirmed to belong to the A and B subgroups, ioxaglate behaves fluctuating within A, B and C, but iodamide looks surprizingly, constantly positioned together with iodoxamate as binary/ternary C associated. In view of the recent work of Campillos et al (Science, 2008) which throws light on the subject, the above discrepancies do not appear anymore unexpected or alarming. -

ACR Manual on Contrast Media
ACR Manual On Contrast Media 2021 ACR Committee on Drugs and Contrast Media Preface 2 ACR Manual on Contrast Media 2021 ACR Committee on Drugs and Contrast Media © Copyright 2021 American College of Radiology ISBN: 978-1-55903-012-0 TABLE OF CONTENTS Topic Page 1. Preface 1 2. Version History 2 3. Introduction 4 4. Patient Selection and Preparation Strategies Before Contrast 5 Medium Administration 5. Fasting Prior to Intravascular Contrast Media Administration 14 6. Safe Injection of Contrast Media 15 7. Extravasation of Contrast Media 18 8. Allergic-Like And Physiologic Reactions to Intravascular 22 Iodinated Contrast Media 9. Contrast Media Warming 29 10. Contrast-Associated Acute Kidney Injury and Contrast 33 Induced Acute Kidney Injury in Adults 11. Metformin 45 12. Contrast Media in Children 48 13. Gastrointestinal (GI) Contrast Media in Adults: Indications and 57 Guidelines 14. ACR–ASNR Position Statement On the Use of Gadolinium 78 Contrast Agents 15. Adverse Reactions To Gadolinium-Based Contrast Media 79 16. Nephrogenic Systemic Fibrosis (NSF) 83 17. Ultrasound Contrast Media 92 18. Treatment of Contrast Reactions 95 19. Administration of Contrast Media to Pregnant or Potentially 97 Pregnant Patients 20. Administration of Contrast Media to Women Who are Breast- 101 Feeding Table 1 – Categories Of Acute Reactions 103 Table 2 – Treatment Of Acute Reactions To Contrast Media In 105 Children Table 3 – Management Of Acute Reactions To Contrast Media In 114 Adults Table 4 – Equipment For Contrast Reaction Kits In Radiology 122 Appendix A – Contrast Media Specifications 124 PREFACE This edition of the ACR Manual on Contrast Media replaces all earlier editions. -

Gadolinium Based Contrast Agents
CE Credits Available CONSIDERATIONS IN THE SELECTION OF A NEW GADOLINIUM-BASED CONTRAST AGENT SUPPLEMENT TO MAY 2014 THE JOURNAL OF PRACTICAL MEDICAL IMAGING AND MANAGEMENT Considerations in the Selection of a New Gadolinium-Based Contrast Agent Michael F. Tweedle, PhD Emanuel Kanal, MD, FACR, FISMRM Robert Muller, PhD Stefanie Spielman Professor of Radiology Professor of Radiology and Neuroradiology Department of General, Organic & The Ohio State University University of Pittsburgh Medical Center Biochemical Chemistry Columbus, OH Pittsburgh, PA University of Mons Mons, Belgium Supported by an unrestricted educational grant from © May 2014 www.appliedradiology.com SUPPLEMENT TO APPLIED RADIOLOGY n 1 Publisher Kieran Anderson Executive Editor Cristen Bolan Art and Production Barbara A. Shopiro Applied Radiology and this supplement, Considerations in the Selection of a New Gadolinium-Based Contrast Agent, are published by Anderson Publishing, Ltd. The journal does not warrant the expertise of any author in a particular field, nor is it responsible for any statements by such authors. The opinions expressed in this supplement are those of the authors. They do not imply endorsement of advertised products and do not necessarily reflect the opinions or recommendations of our sponsors or the editors and staff of Applied Radiology. Copyright © 2014 by Anderson Publishing, Ltd., 180 Glenside Avenue, Scotch Plains, NJ 07076 All rights reserved. Cover images courtesy of Howard A. Rowley, MD. Considerations in the Selection of a New Gadolinium-Based Contrast Agent Our 3 esteemed faculty summarize the similarities and differences among the gadolinium-based contrast agents (GBCAs) currently utilized for magnetic resonance imaging (MRI), with emphasis on stability and relaxivity. -

Advisory Committee Briefing Document Medical Imaging Drugs Advisory Committee (MIDAC) September 8, 2017
Dotarem® (gadoterate meglumine) Injection – NDA# 204781 Advisory Committee Optimark® (gadoversetamide) Injection - NDAs# 020937, 020975 & 020976 Briefing Document Advisory Committee Briefing Document Medical Imaging Drugs Advisory Committee (MIDAC) September 8, 2017 DOTAREM® (gadoterate meglumine) Injection NDA 204781 Guerbet LLC, 821 Alexander Rd, Princeton, NJ 08540 OPTIMARK® (gadoversetamide) Injection NDAs 020937, 020975 & 020976 Liebel-Flarsheim Company LLC, 1034 Brentwood Blvd., Richmond Heights, MO 63117 ADVISORY COMMITTEE BRIEFING MATERIALS AVAILABLE FOR PUBLIC RELEASE Information provided within this briefing document is based upon medical and scientific information available to date. ADVISORY COMMITTEE BRIEFING MATERIALS AVAILABLE FOR PUBLIC RELEASE Page 1 / 168 Dotarem® (gadoterate meglumine) Injection – NDA# 204781 Advisory Committee Optimark® (gadoversetamide) Injection - NDAs# 020937, 020975 & 020976 Briefing Document EXECUTIVE SUMMARY Gadolinium-based contrast agents (GdCAs) are essential for use in magnetic resonance imaging (MRI). Although non-contrast-enhanced MRI may be sufficient for use in some clinical conditions, contrast-enhanced MRI (CE-MRI) using GdCA provides additional vital diagnostic information in a number of diseases. It is widely recognized that CE-MRI increases diagnostic accuracy and confidence, and thus can impact the medical and/or surgical management of patients. Based on the chemical structure of the complexing ligand, GdCA are classified as linear (L-GdCA) or macrocyclic (M-GdCA) and can be ionic or nonionic and those characteristics have a dramatic influence on the stability of the GdCA. Dotarem®, a M-GdCA, was first approved in France in 1989. US-FDA approval was obtained in March 2013 for “intravenous use with MRI of the brain (intracranial), spine and associated tissues in adult and pediatric patients (2 years of age and older) to detect and visualize areas with disruption of the blood brain barrier (BBB) and/or abnormal vascularity”, at the dose of 0.1 mmol/kg BW. -

Estonian Statistics on Medicines 2016 1/41
Estonian Statistics on Medicines 2016 ATC code ATC group / Active substance (rout of admin.) Quantity sold Unit DDD Unit DDD/1000/ day A ALIMENTARY TRACT AND METABOLISM 167,8985 A01 STOMATOLOGICAL PREPARATIONS 0,0738 A01A STOMATOLOGICAL PREPARATIONS 0,0738 A01AB Antiinfectives and antiseptics for local oral treatment 0,0738 A01AB09 Miconazole (O) 7088 g 0,2 g 0,0738 A01AB12 Hexetidine (O) 1951200 ml A01AB81 Neomycin+ Benzocaine (dental) 30200 pieces A01AB82 Demeclocycline+ Triamcinolone (dental) 680 g A01AC Corticosteroids for local oral treatment A01AC81 Dexamethasone+ Thymol (dental) 3094 ml A01AD Other agents for local oral treatment A01AD80 Lidocaine+ Cetylpyridinium chloride (gingival) 227150 g A01AD81 Lidocaine+ Cetrimide (O) 30900 g A01AD82 Choline salicylate (O) 864720 pieces A01AD83 Lidocaine+ Chamomille extract (O) 370080 g A01AD90 Lidocaine+ Paraformaldehyde (dental) 405 g A02 DRUGS FOR ACID RELATED DISORDERS 47,1312 A02A ANTACIDS 1,0133 Combinations and complexes of aluminium, calcium and A02AD 1,0133 magnesium compounds A02AD81 Aluminium hydroxide+ Magnesium hydroxide (O) 811120 pieces 10 pieces 0,1689 A02AD81 Aluminium hydroxide+ Magnesium hydroxide (O) 3101974 ml 50 ml 0,1292 A02AD83 Calcium carbonate+ Magnesium carbonate (O) 3434232 pieces 10 pieces 0,7152 DRUGS FOR PEPTIC ULCER AND GASTRO- A02B 46,1179 OESOPHAGEAL REFLUX DISEASE (GORD) A02BA H2-receptor antagonists 2,3855 A02BA02 Ranitidine (O) 340327,5 g 0,3 g 2,3624 A02BA02 Ranitidine (P) 3318,25 g 0,3 g 0,0230 A02BC Proton pump inhibitors 43,7324 A02BC01 Omeprazole -

Injection of Contrast Media V7 – 2010 13 5
ACR Manual on Contrast Media Version 8 2012 ACR Committee on Drugs and Contrast Media ACR Manual on Contrast Media Version 8 2012 ACR Committee on Drugs and Contrast Media © Copyright 2012 American College of Radiology ISBN: 978-1-55903-009-0 Table of Contents Topic Last Updated Page 1. Preface. V8 – 2012 . 3 2. Introduction . V7 – 2010 . 4 3. Patient Selection and Preparation Strategies . V7 – 2010 . 5 4. Injection of Contrast Media . V7 – 2010 . 13 5. Extravasation of Contrast Media . V7 – 2010 . 17 6. Adverse Events After Intravascular Iodinated Contrast Media . V8 – 2012 . 21 Administration 7. Contrast Media Warming . V8 – 2012 . 29 8. Contrast-Induced Nephrotoxicity . V8 – 2012 . 33 9. Metformin . V7 – 2010 . 43 10. Contrast Media in Children . V7 – 2010 . 47 11. Iodinated Gastrointestinal Contrast Media in Adults: Indications . V7 – 2010 . 55 and Guidelines 12. Adverse Reactions to Gadolinium-Based Contrast Media . V7 – 2010 . 59 13. Nephrogenic Systemic Fibrosis (NSF) . V8 – 2012 . 63 14. Treatment of Contrast Reactions . V8 – 2012 . 73 15. Administration of Contrast Media to Pregnant or Potentially . V6 – 2008. 75 Pregnant Patients 16. Administration of Contrast Media to Breast-Feeding Mothers . V6 – 2008 . 79 Table 1 – Indications for Use of Iodinated Contrast Media . V6 – 2008 . 81 Table 2 – Organ or System-Specific Adverse Effects from the Administration . V7 – 2010 . 82 of Iodine-Based or Gadolinium-Based Contrast Agents Table 3 – Categories of Reactions . V7 – 2010 . 83 Table 4 – Management of Acute Reactions in Children . V7 – 2010 . 84 Table 5 – Management of Acute Reactions in Adults . V6 – 2008 . 86 Table 6 – Equipment for Emergency Carts . V6 – 2008 . -

Art. 31 Gadolinium
Annex I List of nationally authorised medicinal products 1 Annex IA – medicinal products containing intravenous gadobenic acid, gadobutrol, gadoteric acid, gadoteridol, gadoxetic acid and intra-articular gadopentetic acid and intra-articular gadoteric acid Member State Marketing Invented name INN + Strength Pharmaceutical form Route of EU/EEA authorisation holder administration Austria Bayer Austria GmbH Magnevist Gadopentetate solution for injection intra-aintra-articular use Dimeglumine 1.876mg/Ml Austria Bayer Austria GmbH Dotagraf Gadoteric Acid solution for injection intravenous use 279.32mg/Ml Austria Bayer Austria GmbH Gadovist Gadobutrol solution for injection intravenous use 604.72mg/Ml Austria Bayer Austria GmbH Primovist Gadoxetic Acid, solution for injection intravenous use Disodium 181.43mg/Ml Austria Bracco Imaging S.p.A. Prohance Gadoteridol solution for injection intravenous use 279.3mg/Ml Austria Guerbet Artirem Gadoteric Acid solution for injection intra-articular use 1.397mg/Ml Austria Guerbet Dotarem Gadoteric Acid solution for injection intravenous use 279.32mg/Ml Austria Sanochemia Cyclolux Gadoteric Acid solution for injection intravenous use Pharmazeutika AG 0.5mmol/Ml Austria Bracco Imaging S.p.A. Multihance Gadobenate solution for injection intravenous use Dimeglumine 529mg/Ml Belgium Agfa Healthcare Imaging Dotagita Gadoteric Acid solution for injection intravenous use Agents GmbH 279.32mg/Ml Belgium Bayer SA NV Dotagraph Gadoteric Acid solution for injection intravenous use 279.32mg/Ml 2 Member State Marketing -

Public Assessment Report for Paediatric Studies Submitted in Accordance with Article 46 of Regulation (EC) No1901/2006, As Amended
Public Assessment Report for paediatric studies submitted in accordance with Article 46 of Regulation (EC) No1901/2006, as amended Eovist/Primovist (Gadoxetic acid) SE/W/0021/pdWS/001 Marketing Authorisation Holder: Bayer Pharma AG Rapporteur: SE Finalisation procedure (day 120): 2015-03-04 SE/W/0021/pdWS/001-Eovist/Primovist Page 1/25 ADMINISTRATIVE INFORMATION Invented name of the medicinal Eovist/Primovist product: INN (or common name) of the active Gadoxetic acid substance(s): MAH: Bayer Pharma AG Currently approved Indication(s) Magnetic resonance contrast imaging Pharmaco-therapeutic group V08CA10 (ATC Code): Pharmaceutical form(s) and Solution for injection strength(s): SE/W/0021/pdWS/001-Eovist/Primovist Page 2/25 I. EXECUTIVE SUMMARY Changes to sections 4.2 and 5.1 of the SmPC with corresponding changes in the package leaflet are recommended. II. RECOMMENDATION1 Currently Primovist is not approved for the use in the paediatric population in the European Union. The MAH has submitted data from a company sponsored paediatric clinical study and the results from a literature review focusing on children below 18 years of age. Based on the submitted data it can be concluded that beneficial effects of Primovist enhanced liver MRI in paediatric patients have been seen. Due to the relatively small number of patients the data cannot be considered to be confirmatory regarding the efficacy and safety of Primovist in the paediatric population. The proposed rephrasing of section 4.2 of the SmPC, with the deletion of “cannot be recommended” in the paediatric population and addition of a cross reference to section 5.1 is acceptable. -

Active Moiety Name FDA Established Pharmacologic Class (EPC) Text
FDA Established Pharmacologic Class (EPC) Text Phrase PLR regulations require that the following statement is included in the Highlights Indications and Usage heading if a drug is a member of an EPC [see 21 CFR 201.57(a)(6)]: Active Moiety Name “(Drug) is a (FDA EPC Text Phrase) indicated for [indication(s)].” For each listed active moiety, the associated FDA EPC text phrase is included in this document. For more information about how FDA determines the EPC Text Phrase, see the 2009 "Determining EPC for Use in the Highlights" guidance and 2013 "Determining EPC for Use in the Highlights" MAPP 7400.13. -

Premedication for Contrast Medium Allergies Factfinder
Published March 2014 Premedication for Contrast Medium Allergies FactFinder Committed to providing helpful information to International Spine Intervention Society members about key patient safety issues, the Society’s Patient Safety Committee has developed a FactFinder series. FactFinders will explore and debunk myths surrounding patient safety issues. The intent of this FactFinder is to present the evidence regarding the effectiveness of premedication for contrast medium allergies that impact the delivery of spinal procedures. Myth #1: In patients with radiocontrast media (RCM) allergy, it is safe to proceed with RCM injection as long as the patient is premedicated with steroids and antihistamines. Fact: Although premedication likely reduces the risks associated with injecting RCM, no premedication regimen has been proven safe for a RCM allergic reaction. Conclusions & Recommendations The International Spine Intervention Society Guidelines recommend the use of RCM for nearly all spinal diagnostic and treatment procedures.1 An understanding of the severity and frequency of reactions to RCM is paramount prior to discussing premedication. Reactions to RCM are immediate, defined as within the first hour, with 70% occurring within the first five minutes; or late, occurring between one hour and one week later. The late reactions are typically cutaneous.2 There are three types of immediate reactions: mild, moderate, and severe. Mild reactions: include nausea, vomiting, and mild urticaria. These signs and symptoms appear self-limited without evidence of progression. Treatment usually entails only observation and reassurance, however, these reactions may progress into a more severe category. Moderate reactions: include moderate urticaria, vasovagal reaction, mild bronchospasm, and tachycardia. These reactions require treatment, but are not immediately life threatening. -
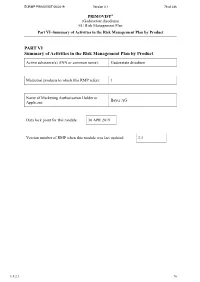
PART VI Summary of Activities in the Risk Management Plan by Product
EURMP PRIMOVIST 06/2019 Version 3.1 76 of 236 PRIMOVIST® (Gadoxetate disodium) EU Risk Management Plan Part VI–Summary of Activities in the Risk Management Plan by Product PART VI Summary of Activities in the Risk Management Plan by Product Active substance(s) (INN or common name): Gadoxetate disodium Medicinal products to which this RMP refers: 1 Name of Marketing Authorisation Holder or Bayer AG Applicant: Data lock point for this module 30 APR 2019 Version number of RMP when this module was last updated 3.1 1.8.2.1 76 EURMP PRIMOVIST 06/2019 Version 3.1 77 of 236 PRIMOVIST® (Gadoxetate disodium) EU Risk Management Plan Part VI–Summary of Activities in the Risk Management Plan by Product Summary of Risk Management Plan for Primovist (Gadoxetate disodium) This is a summary of the Risk Management Plan (RMP) for Primovist. The RMP details important risks associated with Primovist, how these risks can be minimised, and how more information will be obtained about Primovist’s risks and uncertainties (missing information). Primovist’s Summary of Product Characteristics (SmPC) and its package leaflet gives essential information to healthcare professionals and patients on how Primovist should be used. Important new concerns or changes to the current ones will be included in updates of the Primovist’s RMP. 1. The medicine and what it is used for Primovist is authorised for diagnostic use. Primovist is a gadolinium-containing contrast agent for T1-weighted magnetic resonance imaging (MRI) of the liver (see SmPC for the full indication). It contains gadoxetate disodium (gadoxetic acid, Gd-EOB-DTPA) as the active substance and is given by the intravenous route of administration as a solution for injection.