Injection of Contrast Media V7 – 2010 13 5
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Amidotrizoic Acid/Barium Sulfate 1477 Imbalance Should Be Corrected Before Contrast Media Are Given
Amidotrizoic Acid/Barium Sulfate 1477 imbalance should be corrected before contrast media are given. management of adhesive small bowel obstruction;2 they allow pyloric stenosis or lesions that may predispose to obstruction. Particular care is needed in patients with multiple myeloma since identification of patients who require surgery and, although they Adequate hydration should be ensured after the procedure to pre- dehydration resulting from use of contrast media may cause pre- have not been shown to relieve obstruction, they may reduce vent severe constipation. cipitation of protein in the renal tubules, leading to anuria and length of hospital stay in patients treated without surgery. It is contra-indicated in patients with gastrointestinal perforation, fatal renal failure. 1. Murshed R, et al. Meconium ileus: a ten-year review of thirty-six and should be avoided, particularly when given rectally, in those Caution is also necessary in patients with severe hypertension, patients. Eur J Pediatr Surg 1997; 7: 275–7. at risk of perforation, such as patients with acute ulcerative colitis advanced cardiac disease, phaeochromocytoma, sickle-cell dis- 2. Abbas S, et al. Oral water soluble contrast for the management or diverticulitis and after rectal or colonic biopsy, sigmoidosco- of adhesive small bowel obstruction. Available in The Cochrane ease, or hyperthyroidism or epilepsy, and in debilitated, severely Database of Systematic Reviews; Issue 3. Chichester: John Wi- py, or radiotherapy. ill, very old, or very young patients. ley; 2007 (accessed 14/07/08). Uses and Administration Amidotrizoates and other hypertonic contrast media are neuro- Preparations Barium sulfate is used as a radiographic contrast medium toxic and should not be given intrathecally; patients with sub- (p.1474) for X-ray examination of the gastrointestinal tract in- arachnoid haemorrhage may be at risk with any intravascular BP 2008: Meglumine Amidotrizoate Injection; Sodium Amidotrizoate In- jection; volving single- or double-contrast techniques or computed tom- use. -

Intrathecal Gadolinium-Enhanced MR Cisternography in the Evaluation Of
Intrathecal Gadolinium-Enhanced MR ORIGINAL RESEARCH Cisternography in the Evaluation of CSF Leakage H. Selcuk BACKROUND AND PURPOSE: Radiologic identification of the location of the CSF leakage is important S. Albayram for proper surgical planning and increases the chance of dural repair. This article describes our experience in analyzing clinically suspected cranial CSF fistulas by using MR imaging combined with H. Ozer the intrathecal administration of a gadolinium-based contrast agent. S. Ulus MATERIALS AND METHODS: A total of 85 consecutive patients with suspected CSF fistulas who G.Z. Sanus presented with persistent or intermittent rhinorrhea or otorrhea lasting for more than 1 month between M.Y. Kaynar 2003 and 2007 were included in this study. N. Kocer RESULTS: We observed objective CSF leakage in 64 of 85 patients (75%). The CSF leak was located C. Islak in the ethmoidal region in 37 patients (58%), in the superior wall of the sphenoid sinus in 8 patients (13%), in the posterior wall of the frontal sinus in 10 patients (15%), in the superior wall of the mastoid air cells in 6 patients (9%), and from the skull base into the infratemporal fossa in 1 patient (2%). Two patients (3%) showed leakage into Ͼ1 paranasal sinus. CONCLUSIONS: MR cisternography after the intrathecal administration of gadopentate dimeglumine represents an effective and minimally invasive method for evaluating suspected CSF fistulas along the skull base. It provides multiplanar capabilities without risk of radiation exposure and is an excellent approach to depict the anatomy of CSF spaces and CSF fistulas. SF leakage implies abnormal communication between the using this technique.19,20 In addition, the combination of CT Csubarachnoid space and the nasal or middle ear cavity. -

The National Drugs List
^ ^ ^ ^ ^[ ^ The National Drugs List Of Syrian Arab Republic Sexth Edition 2006 ! " # "$ % &'() " # * +$, -. / & 0 /+12 3 4" 5 "$ . "$ 67"5,) 0 " /! !2 4? @ % 88 9 3: " # "$ ;+<=2 – G# H H2 I) – 6( – 65 : A B C "5 : , D )* . J!* HK"3 H"$ T ) 4 B K<) +$ LMA N O 3 4P<B &Q / RS ) H< C4VH /430 / 1988 V W* < C A GQ ") 4V / 1000 / C4VH /820 / 2001 V XX K<# C ,V /500 / 1992 V "!X V /946 / 2004 V Z < C V /914 / 2003 V ) < ] +$, [2 / ,) @# @ S%Q2 J"= [ &<\ @ +$ LMA 1 O \ . S X '( ^ & M_ `AB @ &' 3 4" + @ V= 4 )\ " : N " # "$ 6 ) G" 3Q + a C G /<"B d3: C K7 e , fM 4 Q b"$ " < $\ c"7: 5) G . HHH3Q J # Hg ' V"h 6< G* H5 !" # $%" & $' ,* ( )* + 2 ا اوا ادو +% 5 j 2 i1 6 B J' 6<X " 6"[ i2 "$ "< * i3 10 6 i4 11 6! ^ i5 13 6<X "!# * i6 15 7 G!, 6 - k 24"$d dl ?K V *4V h 63[46 ' i8 19 Adl 20 "( 2 i9 20 G Q) 6 i10 20 a 6 m[, 6 i11 21 ?K V $n i12 21 "% * i13 23 b+ 6 i14 23 oe C * i15 24 !, 2 6\ i16 25 C V pq * i17 26 ( S 6) 1, ++ &"r i19 3 +% 27 G 6 ""% i19 28 ^ Ks 2 i20 31 % Ks 2 i21 32 s * i22 35 " " * i23 37 "$ * i24 38 6" i25 39 V t h Gu* v!* 2 i26 39 ( 2 i27 40 B w< Ks 2 i28 40 d C &"r i29 42 "' 6 i30 42 " * i31 42 ":< * i32 5 ./ 0" -33 4 : ANAESTHETICS $ 1 2 -1 :GENERAL ANAESTHETICS AND OXYGEN 4 $1 2 2- ATRACURIUM BESYLATE DROPERIDOL ETHER FENTANYL HALOTHANE ISOFLURANE KETAMINE HCL NITROUS OXIDE OXYGEN PROPOFOL REMIFENTANIL SEVOFLURANE SUFENTANIL THIOPENTAL :LOCAL ANAESTHETICS !67$1 2 -5 AMYLEINE HCL=AMYLOCAINE ARTICAINE BENZOCAINE BUPIVACAINE CINCHOCAINE LIDOCAINE MEPIVACAINE OXETHAZAINE PRAMOXINE PRILOCAINE PREOPERATIVE MEDICATION & SEDATION FOR 9*: ;< " 2 -8 : : SHORT -TERM PROCEDURES ATROPINE DIAZEPAM INJ. -

The Study Programme for the Quality Management of Essential Medicines - Good Manufacturing Practical (GMP) and Inspection
The Study Programme for the Quality Management of Essential Medicines - Good Manufacturing Practical (GMP) and Inspection - Country Reports Japan International Corporation of Welfare Services (JICWELS) Contents 1. Cambodia 1 2. Indonesia 70 3. Malaysia 91 4. Philippines 116 5. Sri Lanka 141 6. Thailand 161 The Study Programme for the Quality Management of Essential Medicines - Good Manufacturing Practical (GMP) and Inspection - Cambodia -1- KINGDOM OF CAMBODIA Nation Religion King Ministry of Health Department of Drugs and Food Country Report The Study Program on Quality Management of Essential Medicines Good Manufacturing Practice (GMP) and Inspection November 4, 2012 – November 30, 2012 Sponsored by : The Government of Japan Japan International Cooperation Agency (JICA) Department of Drugs and Food Ministry of Health, Cambodia. -2- I- COUNTRY PROFILE -3- A-Geography Cambodia is an agricultural country located in South East Asia which bordering the Gulf of Thailand, between Thailand, Vietnam, and Laos. Its approximate geographical coordinates are 13°N 105°E. Its 2,572 km border is split among Vietnam (1,228 km), Thailand (803 km) and Laos (541 km), as well as 443 km of coastline. Cambodia covers 181,035 square kilometers in the southwestern part of the Indochina, Cambodia lies completely within the tropics; its southernmost points are only slightly more than 10° above the equator. The country is bounded on the north by Thailand and by Laos, on the east and southeast by Vietnam, and on the west by the Gulf of Thailand and by Thailand. It consists of the Tonle Sap Basin and the Mekong Lowlands. To the southeast of this great basin is the Mekong Delta, which extends through Vietnam to the South China Sea. -

MDCT and Contrast Media: What Are the Risks?
071_078_00_Thomsen:Thomsen 13-02-2008 9:32 Pagina 71 MDCT and Contrast Media: What are the Risks? Henrik S. Thomsen Department of Diagnostic Radiology, Copenhagen University Hospital Herlev, Herlev Department of Diagnostic Sciences, Faculty of Health Sciences, University of Copenhagen, Denmark Introduction Renal Adverse Reactions With the advent of multi-detector computed to- Contrast-material-induced kidney damage is imme- mography (MDCT) technology, the number of pa- diate, starting as soon as the first CM molecule reach- tients undergoing contrast-enhanced CT (CECT) es the kidney; however, it takes several hours or days studies has steadily grown in the last 6 years. In for a deterioration of renal function to be detected. 2005, approximately 22 million CECT examinations Despite more than 30 years of research, the patho- were carried out in the European Union, and 32 mil- physiology of CM-induced nephropathy (CIN) is lion in the United States (The Imaging Market Guide poorly elucidated. Nonetheless, several risk factors 2005. Arlington Medical Resources, Inc., Philadel- are well-known and can be divided into CM- and pa- phia, PA). Unfortunately, post-contrast-material-re- tient-related factors. lated adverse events, i.e., all those unintended and unfavorable signs, symptoms, or diseases temporally associated with the use of an iodinated contrast ma- Contrast-Medium-Related Factors terial (CM), are a common occurrence in radiology departments. Most adverse events occur within the More than 25 years ago, Barrett and Carlisle [1] first 60 min following CM administration (“imme- showed that the incidence of CIN is significantly diate” or “acute” adverse events), with the greatest higher after the administration of high-osmolarity risk in the first 20 min. -
List of Union Reference Dates A
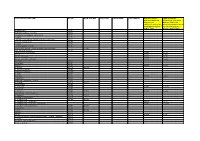
Active substance name (INN) EU DLP BfArM / BAH DLP yearly PSUR 6-month-PSUR yearly PSUR bis DLP (List of Union PSUR Submission Reference Dates and Frequency (List of Union Frequency of Reference Dates and submission of Periodic Frequency of submission of Safety Update Reports, Periodic Safety Update 30 Nov. 2012) Reports, 30 Nov. -

Guideline on Core Smpc and Package Leaflet for Gadoteric Acid EMA/CHMP/337820/2016 Page 2/23
1 26 May 2016 2 EMA/CHMP/337820/2016 3 Committee for Medicinal Products for Human Use (CHMP) 4 Guideline on core SmPC and Package Leaflet for gadoteric 5 acid 6 Draft Draft agreed by Radiopharmaceutical Drafting Group April 2016 Adopted by CHMP for release for consultation 26 May 2016 Start of public consultation 1 June 2016 End of consultation (deadline for comments) 30 September 2016 7 Comments should be provided using this template. The completed comments form should be sent to [email protected]. 8 Keywords Magnetic resonance, contrast media, gadolinium compounds, core SmPC, core Package Leaflet, gadoteric acid 9 30 Churchill Place ● Canary Wharf ● London E14 5EU ● United Kingdom Telephone +44 (0)20 3660 6000 Facsimile +44 (0)20 3660 5555 Send a question via our website www.ema.europa.eu/contact An agency of the European Union © European Medicines Agency, 2016. Reproduction is authorised provided the source is acknowledged. 10 Guideline on core SmPC and Package Leaflet for gadoteric 11 acid 12 Table of contents 13 Executive summary ..................................................................................... 3 14 1. Introduction (background) ...................................................................... 3 15 2. Scope....................................................................................................... 3 16 3. Legal basis .............................................................................................. 3 17 4. Core SmPC and Package Leaflet for gadoteric acid ................................. -

Pharmacologyonline 2: 727-753 (2010) Ewsletter Bradu and Rossini
Pharmacologyonline 2: 727-753 (2010) ewsletter Bradu and Rossini COTRAST AGETS - IODIATED PRODUCTS. SECOD WHO-ITA / ITA-OMS 2010 COTRIBUTIO O AGGREGATE WHO SYSTEM-ORGA CLASS DISORDERS AD/OR CLUSTERIG BASED O REPORTED ADVERSE REACTIOS/EVETS Dan Bradu and Luigi Rossini* Servizio Nazionale Collaborativo WHO-ITA / ITA-OMS, Università Politecnica delle Marche e Progetto di Farmacotossicovigilanza, Azienda Ospedaliera Universitaria Ospedali Riuniti di Ancona, Regione Marche, Italia Summary From the 2010 total basic adverse reactions and events collected as ADRs preferred names in the WHO-Uppsala Drug Monitoring Programme, subdivided in its first two twenty years periods as for the first seven iodinated products diagnostic contrast agents amidotrizoate, iodamide, iotalamate, iodoxamate, ioxaglate, iohexsol and iopamidol, their 30 WHO-system organ class disorders (SOCDs) aggregates had been compared. Their common maximum 97% levels identified six SOCDs only, apt to evaluate the most frequent single ADRs for each class, and their percentual normalization profiles for each product. The WILKS's chi square statistics for the related contingency tables, and Gabriel’s STP procedure applied to the extracted double data sets then produced profile binary clustering, as well as Euclidean confirmatory plots. They finally showed similar objectively evaluated autoclassificative trends of these products, which do not completely correspond to their actual ATC V08A A, B and C subdivision: while amidotrizoate and iotalamate, and respectively iohesol and iopamidol are confirmed to belong to the A and B subgroups, ioxaglate behaves fluctuating within A, B and C, but iodamide looks surprizingly, constantly positioned together with iodoxamate as binary/ternary C associated. In view of the recent work of Campillos et al (Science, 2008) which throws light on the subject, the above discrepancies do not appear anymore unexpected or alarming. -

Drug-Induced Anaphylaxis in China: a 10 Year Retrospective Analysis of The
Int J Clin Pharm DOI 10.1007/s11096-017-0535-2 RESEARCH ARTICLE Drug‑induced anaphylaxis in China: a 10 year retrospective analysis of the Beijing Pharmacovigilance Database Ying Zhao1,2,3 · Shusen Sun4 · Xiaotong Li1,3 · Xiang Ma1 · Huilin Tang5 · Lulu Sun2 · Suodi Zhai1 · Tiansheng Wang1,3,6 Received: 9 May 2017 / Accepted: 19 September 2017 © The Author(s) 2017. This article is an open access publication Abstract Background Few studies on the causes of (50.1%), mucocutaneous (47.4%), and gastrointestinal symp- drug-induced anaphylaxis (DIA) in the hospital setting are toms (31.3%). A total of 249 diferent drugs were involved. available. Objective We aimed to use the Beijing Pharma- DIAs were mainly caused by antibiotics (39.3%), traditional covigilance Database (BPD) to identify the causes of DIA Chinese medicines (TCM) (11.9%), radiocontrast agents in Beijing, China. Setting Anaphylactic case reports from (11.9%), and antineoplastic agents (10.3%). Cephalospor- the BPD provided by the Beijing Center for Adverse Drug ins accounted for majority (34.5%) of antibiotic-induced Reaction Monitoring. Method DIA cases collected by the anaphylaxis, followed by fuoroquinolones (29.6%), beta- BPD from January 2004 to December 2014 were adjudi- lactam/beta-lactamase inhibitors (15.4%) and penicillins cated. Cases were analyzed for demographics, causative (7.9%). Blood products and biological agents (3.1%), and drugs and route of administration, and clinical signs and plasma substitutes (2.1%) were also important contributors outcomes. Main outcome measure Drugs implicated in DIAs to DIAs. Conclusion A variety of drug classes were impli- were identifed and the signs and symptoms of the DIA cases cated in DIAs. -

Title 16. Crimes and Offenses Chapter 13. Controlled Substances Article 1
TITLE 16. CRIMES AND OFFENSES CHAPTER 13. CONTROLLED SUBSTANCES ARTICLE 1. GENERAL PROVISIONS § 16-13-1. Drug related objects (a) As used in this Code section, the term: (1) "Controlled substance" shall have the same meaning as defined in Article 2 of this chapter, relating to controlled substances. For the purposes of this Code section, the term "controlled substance" shall include marijuana as defined by paragraph (16) of Code Section 16-13-21. (2) "Dangerous drug" shall have the same meaning as defined in Article 3 of this chapter, relating to dangerous drugs. (3) "Drug related object" means any machine, instrument, tool, equipment, contrivance, or device which an average person would reasonably conclude is intended to be used for one or more of the following purposes: (A) To introduce into the human body any dangerous drug or controlled substance under circumstances in violation of the laws of this state; (B) To enhance the effect on the human body of any dangerous drug or controlled substance under circumstances in violation of the laws of this state; (C) To conceal any quantity of any dangerous drug or controlled substance under circumstances in violation of the laws of this state; or (D) To test the strength, effectiveness, or purity of any dangerous drug or controlled substance under circumstances in violation of the laws of this state. (4) "Knowingly" means having general knowledge that a machine, instrument, tool, item of equipment, contrivance, or device is a drug related object or having reasonable grounds to believe that any such object is or may, to an average person, appear to be a drug related object. -

Page 1 Note: Within Nine Months from the Publication of the Mention
Europäisches Patentamt (19) European Patent Office & Office européen des brevets (11) EP 1 411 992 B1 (12) EUROPEAN PATENT SPECIFICATION (45) Date of publication and mention (51) Int Cl.: of the grant of the patent: A61K 49/04 (2006.01) A61K 49/18 (2006.01) 13.12.2006 Bulletin 2006/50 (86) International application number: (21) Application number: 02758379.8 PCT/EP2002/008183 (22) Date of filing: 23.07.2002 (87) International publication number: WO 2003/013616 (20.02.2003 Gazette 2003/08) (54) IONIC AND NON-IONIC RADIOGRAPHIC CONTRAST AGENTS FOR USE IN COMBINED X-RAY AND NUCLEAR MAGNETIC RESONANCE DIAGNOSTICS IONISCHES UND NICHT-IONISCHES RADIOGRAPHISCHES KONTRASTMITTEL ZUR VERWENDUNG IN DER KOMBINIERTEN ROENTGEN- UND KERNSPINTOMOGRAPHIEDIAGNOSTIK SUBSTANCES IONIQUES ET NON-IONIQUES DE CONTRASTE RADIOGRAPHIQUE UTILISEES POUR ETABLIR DES DIAGNOSTICS FAISANT APPEL AUX RAYONS X ET A L’IMAGERIE PAR RESONANCE MAGNETIQUE (84) Designated Contracting States: (74) Representative: Minoja, Fabrizio AT BE BG CH CY CZ DE DK EE ES FI FR GB GR Bianchetti Bracco Minoja S.r.l. IE IT LI LU MC NL PT SE SK TR Via Plinio, 63 20129 Milano (IT) (30) Priority: 03.08.2001 IT MI20011706 (56) References cited: (43) Date of publication of application: EP-A- 0 759 785 WO-A-00/75141 28.04.2004 Bulletin 2004/18 US-A- 5 648 536 (73) Proprietor: BRACCO IMAGING S.p.A. • K HERGAN, W. DORINGER, M. LÄNGLE W.OSER: 20134 Milano (IT) "Effects of iodinated contrast agents in MR imaging" EUROPEAN JOURNAL OF (72) Inventors: RADIOLOGY, vol. 21, 1995, pages 11-17, • AIME, Silvio XP002227102 20134 Milano (IT) • K.M. -

207/2015 3 Lääkeluettelon Aineet, Liite 1. Ämnena I Läkemedelsförteckningen, Bilaga 1
207/2015 3 LÄÄKELUETTELON AINEET, LIITE 1. ÄMNENA I LÄKEMEDELSFÖRTECKNINGEN, BILAGA 1. Latinankielinen nimi, Suomenkielinen nimi, Ruotsinkielinen nimi, Englanninkielinen nimi, Latinskt namn Finskt namn Svenskt namn Engelskt namn (N)-Hydroxy- (N)-Hydroksietyyli- (N)-Hydroxietyl- (N)-Hydroxyethyl- aethylprometazinum prometatsiini prometazin promethazine 2,4-Dichlorbenzyl- 2,4-Diklooribentsyyli- 2,4-Diklorbensylalkohol 2,4-Dichlorobenzyl alcoholum alkoholi alcohol 2-Isopropoxyphenyl-N- 2-Isopropoksifenyyli-N- 2-Isopropoxifenyl-N- 2-Isopropoxyphenyl-N- methylcarbamas metyylikarbamaatti metylkarbamat methylcarbamate 4-Dimethyl- ami- 4-Dimetyyliaminofenoli 4-Dimetylaminofenol 4-Dimethylaminophenol nophenolum Abacavirum Abakaviiri Abakavir Abacavir Abarelixum Abareliksi Abarelix Abarelix Abataceptum Abatasepti Abatacept Abatacept Abciximabum Absiksimabi Absiximab Abciximab Abirateronum Abirateroni Abirateron Abiraterone Acamprosatum Akamprosaatti Acamprosat Acamprosate Acarbosum Akarboosi Akarbos Acarbose Acebutololum Asebutololi Acebutolol Acebutolol Aceclofenacum Aseklofenaakki Aceklofenak Aceclofenac Acediasulfonum natricum Asediasulfoni natrium Acediasulfon natrium Acediasulfone sodium Acenocoumarolum Asenokumaroli Acenokumarol Acenocumarol Acepromazinum Asepromatsiini Acepromazin Acepromazine Acetarsolum Asetarsoli Acetarsol Acetarsol Acetazolamidum Asetatsoliamidi Acetazolamid Acetazolamide Acetohexamidum Asetoheksamidi Acetohexamid Acetohexamide Acetophenazinum Asetofenatsiini Acetofenazin Acetophenazine Acetphenolisatinum Asetofenoli-isatiini