Focus-On-Mental-Health-Booklet.Pdf
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

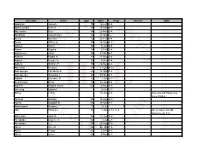
Start Wave Race Colour Race No. First Name Surname
To find your name, click 'ctrl' + 'F' and type your surname. If you entered after 20/02/20 you will not appear on this list, an updated version will be put online on or around the 28/02/20. Runners cannot move into an earlier wave, but you are welcome to move back to a later wave. You do NOT need to inform us of your decision to do this. If you have any problems, please get in touch by phoning 01522 699950. COLOUR RACE APPROX TO THE START WAVE NO. START TIME 1 BLUE A 09:10 2 RED A 09:10 3 PINK A 09:15 4 GREEN A 09:20 5 BLUE B 09:32 6 RED B 09:36 7 PINK B 09:40 8 GREEN B 09:44 9 BLUE C 09:48 10 RED C 09:52 11 PINK C 09:56 12 GREEN C 10:00 VIP BLACK Start Wave Race Colour Race No. First name Surname 11 Pink 1889 Rebecca Aarons Any Black 1890 Jakob Abada 2 Red 4 Susannah Abayomi 3 Pink 1891 Yassen Abbas 6 Red 1892 Nick Abbey 10 Red 1823 Hannah Abblitt 10 Red 1893 Clare Abbott 4 Green 1894 Jon Abbott 8 Green 1895 Jonny Abbott 12 Green 11043 Pamela Abbott 6 Red 11044 Rebecca Abbott 11 Pink 1896 Leanne Abbott-Jones 9 Blue 1897 Emilie Abby Any Black 1898 Jennifer Abecina 6 Red 1899 Philip Abel 7 Pink 1900 Jon Abell 10 Red 600 Kirsty Aberdein 6 Red 11045 Andrew Abery Any Black 1901 Erwann ABIVEN 11 Pink 1902 marie joan ablat 8 Green 1903 Teresa Ablewhite 9 Blue 1904 Ahid Abood 6 Red 1905 Alvin Abraham 9 Blue 1906 Deborah Abraham 6 Red 1907 Sophie Abraham 1 Blue 11046 Mitchell Abrams 4 Green 1908 David Abreu 11 Pink 11047 Kathleen Abuda 10 Red 11048 Annalisa Accascina 4 Green 1909 Luis Acedo 10 Red 11049 Vikas Acharya 11 Pink 11050 Catriona Ackermann -

The Elucidation of Stress Memory Inheritance in Brassica Rapa Plants
ORIGINAL RESEARCH ARTICLE published: 21 January 2015 doi: 10.3389/fpls.2015.00005 The elucidation of stress memory inheritance in Brassica rapa plants Andriy Bilichak 1, Yaroslav Ilnytskyy 2, Rafal Wóycicki 2, Nina Kepeshchuk 2,DawsonFogen2 and Igor Kovalchuk 2* 1 Lethbridge Research Centre, Agriculture and Agri-Food Canada, Lethbridge, AB, Canada 2 Department of Biological Sciences, University of Lethbridge, Lethbridge, AB, Canada Edited by: Plants are able to maintain the memory of stress exposure throughout their ontogenesis Shawn Kaeppler, University of and faithfully propagate it into the next generation. Recent evidence argues for the Wisconsin-Madison, USA epigenetic nature of this phenomenon. Small RNAs (smRNAs) are one of the vital Reviewed by: epigenetic factors because they can both affect gene expression at the place of Rajandeep Sekhon, Clemson University, USA their generation and maintain non-cell-autonomous gene regulation. Here, we have Thelma Farai Madzima, Florida State made an attempt to decipher the contribution of smRNAs to the heat-shock-induced University, USA transgenerational inheritance in Brassica rapa plants using sequencing technology. To *Correspondence: do this, we have generated comprehensive profiles of a transcriptome and a small Igor Kovalchuk, Department of RNAome (smRNAome) from somatic and reproductive tissues of stressed plants and their Biological Sciences, University of Lethbridge, University Drive 4401, untreated progeny. We have demonstrated that the highest tissue-specific alterations in Lethbridge, AB, T1K 3M4, Canada the transcriptome and smRNAome profile are detected in tissues that were not directly e-mail: [email protected] exposed to stress, namely, in the endosperm and pollen. Importantly, we have revealed that the progeny of stressed plants exhibit the highest fluctuations at the smRNAome level but not at the transcriptome level. -

Family Group Sheets Surname Index
PASSAIC COUNTY HISTORICAL SOCIETY FAMILY GROUP SHEETS SURNAME INDEX This collection of 660 folders contains over 50,000 family group sheets of families that resided in Passaic and Bergen Counties. These sheets were prepared by volunteers using the Societies various collections of church, ceme tery and bible records as well as city directo ries, county history books, newspaper abstracts and the Mattie Bowman manuscript collection. Example of a typical Family Group Sheet from the collection. PASSAIC COUNTY HISTORICAL SOCIETY FAMILY GROUP SHEETS — SURNAME INDEX A Aldous Anderson Arndt Aartse Aldrich Anderton Arnot Abbott Alenson Andolina Aronsohn Abeel Alesbrook Andreasen Arquhart Abel Alesso Andrews Arrayo Aber Alexander Andriesse (see Anderson) Arrowsmith Abers Alexandra Andruss Arthur Abildgaard Alfano Angell Arthurs Abraham Alje (see Alyea) Anger Aruesman Abrams Aljea (see Alyea) Angland Asbell Abrash Alji (see Alyea) Angle Ash Ack Allabough Anglehart Ashbee Acker Allee Anglin Ashbey Ackerman Allen Angotti Ashe Ackerson Allenan Angus Ashfield Ackert Aller Annan Ashley Acton Allerman Anners Ashman Adair Allibone Anness Ashton Adams Alliegro Annin Ashworth Adamson Allington Anson Asper Adcroft Alliot Anthony Aspinwall Addy Allison Anton Astin Adelman Allman Antoniou Astley Adolf Allmen Apel Astwood Adrian Allyton Appel Atchison Aesben Almgren Apple Ateroft Agar Almond Applebee Atha Ager Alois Applegate Atherly Agnew Alpart Appleton Atherson Ahnert Alper Apsley Atherton Aiken Alsheimer Arbuthnot Atkins Aikman Alterman Archbold Atkinson Aimone -

Alex Harvey and “The Tomahawk Kid”: Mode and Interpretation
Alex Harvey and “The Tomahawk Kid”: Mode and Interpretation David Montgomery Abstract: Alex Harvey and the Sensational Alex Harvey Band achieved only marginal popularity during Harvey’s lifetime. Yet an examination of Harvey’s “The Tomahawk Kid,” based on Robert Louis Stevenson’s Treasure Island, shows an idiosyncratic musical style that combines rock and Scottish Celtic influences, subtle textual interpretation, unique compositional choices, and modal tonalities. Introduction The academic study of popular music oscillates between two preoccupations. On one hand, the dogmas of sub-cultural theory still influence popular music discourse and general cultural theory to a great degree. On the other hand, this discourse cannot escape the parameters of its label— popular. In essence, the two poles may be staked as cultural theory versus popular appreciation; but in a way difficult to describe, the application of critical theory has begun to seem more like an attempt to avoid an aesthetic conundrum— a kind of elevation of the demotic artefact to a height it cannot bear. Ever resourceful, the practitioners of popular music studies have wriggled out of this quandary and into the at least temporarily secure embrace of post feminist studies, world pop, and the ethnography of locale; in other words, into areas where inquiry is either of self-evident importance, exotic, or comfortably esoteric. Even if the locale is no more exotic than Glasgow, Scotland or Montgomery, Alabama, or the object mundane, the conceit of the critical stance has proven sufficient. Things change, canons crumble, time has done its work. The difficult “aesthetics” of popular music studies, the indeterminate nature of its aims, is a nagging problem. -

Geographic Names
GEOGRAPHIC NAMES CORRECT ORTHOGRAPHY OF GEOGRAPHIC NAMES ? REVISED TO JANUARY, 1911 WASHINGTON GOVERNMENT PRINTING OFFICE 1911 PREPARED FOR USE IN THE GOVERNMENT PRINTING OFFICE BY THE UNITED STATES GEOGRAPHIC BOARD WASHINGTON, D. C, JANUARY, 1911 ) CORRECT ORTHOGRAPHY OF GEOGRAPHIC NAMES. The following list of geographic names includes all decisions on spelling rendered by the United States Geographic Board to and including December 7, 1910. Adopted forms are shown by bold-face type, rejected forms by italic, and revisions of previous decisions by an asterisk (*). Aalplaus ; see Alplaus. Acoma; township, McLeod County, Minn. Abagadasset; point, Kennebec River, Saga- (Not Aconia.) dahoc County, Me. (Not Abagadusset. AQores ; see Azores. Abatan; river, southwest part of Bohol, Acquasco; see Aquaseo. discharging into Maribojoc Bay. (Not Acquia; see Aquia. Abalan nor Abalon.) Acworth; railroad station and town, Cobb Aberjona; river, IVIiddlesex County, Mass. County, Ga. (Not Ackworth.) (Not Abbajona.) Adam; island, Chesapeake Bay, Dorchester Abino; point, in Canada, near east end of County, Md. (Not Adam's nor Adams.) Lake Erie. (Not Abineau nor Albino.) Adams; creek, Chatham County, Ga. (Not Aboite; railroad station, Allen County, Adams's.) Ind. (Not Aboit.) Adams; township. Warren County, Ind. AJjoo-shehr ; see Bushire. (Not J. Q. Adams.) Abookeer; AhouJcir; see Abukir. Adam's Creek; see Cunningham. Ahou Hamad; see Abu Hamed. Adams Fall; ledge in New Haven Harbor, Fall.) Abram ; creek in Grant and Mineral Coun- Conn. (Not Adam's ties, W. Va. (Not Abraham.) Adel; see Somali. Abram; see Shimmo. Adelina; town, Calvert County, Md. (Not Abruad ; see Riad. Adalina.) Absaroka; range of mountains in and near Aderhold; ferry over Chattahoochee River, Yellowstone National Park. -

Curriculum Vitae
Curriculum Vitae Personal Information Name: Joshua Morrison Smyth Address: Department of Biobehavioral Health 231 Biobehavioral Health Building Pennsylvania State University University Park, PA 16802, USA Phone: (814) 863-8402 Electronic mail: [email protected] [email protected] Website: sites.psu.edu/shadelab/ Education Ph.D. Health and Social Psychology, concentration in Quantitative Methods, Stony Brook University (1998). Advisor: Arthur Stone M.A. Psychology, Stony Brook University (1994) B.A. Cognitive Science, Vassar College (1991) Professional Experience 2017- Distinguished Professor of Biobehavioral Health and Medicine, Pennsylvania State University and Hershey Medical Center 2015-2017 Academic Director, Survey Research Center, Pennsylvania State University 2015 Acting Co-Director, Clinical and Translational Sciences Institute [CTSI], Pennsylvania State University (01/01/15-06/30/15) 2014- Associate Director, Social Science Research Institute, Pennsylvania State University (Acting Director, 01/01/15-06/30/15) 2014- Associate Director, Children Youth and Family Consortium, Pennsylvania State University (Acting Director, 01/01/15-06/30/15) 2012- Faculty Affiliate, Methodology Center, Pennsylvania State University 2011-2017 Professor of Biobehavioral Health and Medicine, Pennsylvania State University and Hershey Medical Center 2011-2014 Founding Academic Director, Dynamic Real-time Ecological Ambulatory Methodologies [DREAM] Initiative, Pennsylvania State University 2009-2011 Trustee Professor, Department of Psychology, Syracuse University -

Surname First Name Categorisation Abadin Jose Luis Silver Abbelen
2018 DRIVERS' CATEGORISATION LIST Updated on 09/07/2018 Drivers in red : revised categorisation Drivers in blue : new categorisation Surname First name Categorisation Abadin Jose Luis Silver Abbelen Klaus Bronze Abbott Hunter Silver Abbott James Silver Abe Kenji Bronze Abelli Julien Silver Abergel Gabriele Bronze Abkhazava Shota Bronze Abra Richard Silver Abreu Attila Gold Abril Vincent Gold Abt Christian Silver Abt Daniel Gold Accary Thomas Silver Acosta Hinojosa Julio Sebastian Silver Adam Jonathan Platinum Adams Rudi Bronze Adorf Dirk Silver Aeberhard Juerg Silver Afanasiev Sergei Silver Agostini Riccardo Gold Aguas Rui Gold Ahlin-Kottulinsky Mikaela Silver Ahrabian Darius Bronze Ajlani Karim Bronze Akata Emin Bronze Aksenov Stanislas Silver Al Faisal Abdulaziz Silver Al Harthy Ahmad Silver Al Masaood Humaid Bronze Al Qubaisi Khaled Bronze Al-Azhari Karim Bronze Alberico Neil Silver Albers Christijan Platinum Albert Michael Silver Albuquerque Filipe Platinum Alder Brian Silver Aleshin Mikhail Platinum Alesi Giuliano Silver Alessi Diego Silver Alexander Iradj Silver Alfaisal Saud Bronze Alguersuari Jaime Platinum Allegretta Vincent Silver Alleman Cyndie Silver Allemann Daniel Bronze Allen James Silver Allgàuer Egon Bronze Allison Austin Bronze Allmendinger AJ Gold Allos Manhal Bronze Almehairi Saeed Silver Almond Michael Silver Almudhaf Khaled Bronze Alon Robert Silver Alonso Fernando Platinum Altenburg Jeff Bronze Altevogt Peter Bronze Al-Thani Abdulrahman Silver Altoè Giacomo Silver Aluko Kolawole Bronze Alvarez Juan Cruz Silver Alzen -

Links: Michael Schenker Fest
New Release Information uu March MICHAEL SCHENKER FEST Release Date Pre-Order Start Territory: World Resurrection uu 02/03/2018 uu 15/12/2017 Style: Rock uu DIGI and Earbook incl. bonus DVD uu advertising in many important music magazines DEC/JAN 2018 uu album reviews, interviews in all important Metal magazines in Europe’s DEC/JAN 2018 issues uu song placements in European magazine compilations uu spotify playlists in all European territories uu retail marketing campaigns uu instore decoration: flyers, poster A1 uu Facebook, YouTube, Twitter, Google+ organic promotion uu Facebook ads and promoted posts + Google ads in both the search and display networks, bing ads and gmail ads (tbc) uu Banner advertising on more than 60 most important Metal & Rock websites all over Europe uu additional booked ads on Metal Hammer Germany and UK, and in the Fixion network (main- ly Blabbermouth) uu video and pre-roll ads on You tube uu ad campaigns on iPhones for iTunes and Google Play for Androids uu banners, featured items at the shop, header images and a background on nuclearblast.de and nuclearblast.com uu features and banners in newsletters, as well as special mailings to targeted audiences in support of the release Price Code: CD01 uu Tracklists: NB 4173-0 CD+DVD-DIGI (incl. Bonus-DVD) Digi / CD: 01. Heart And Soul 02. Warrior 03. Take Me To The Church 04. Night Moods Price Code: CD04 05. The Girl With The Stars In Her Eyes 06. Everest NB 4173-2 CD 07. Messin’ Around 08. Time Knows When It´s Time 09. -
Surname Given Age Date Page Maiden Note Abdullah Joseph 70 5-Feb A-8 Abercrombie Bert H
Surname Given Age Date Page Maiden Note Abdullah Joseph 70 5-Feb A-8 Abercrombie Bert H. 88 29-Dec B-9 Abernathy Kate 84 22-Nov B-4 Abraham Joseph Ben 86 21-Mar D-2 Acela Michael 73 23-Feb A-4 Achor Arthur A. 58 16-Sep A-11 Adalay Steve 92 6-Jan B-6 Adam Sophia 78 3-Feb B-4 Adamczyk John 85 21-Oct B-7 Adams Edwin B. 81 27-Aug B-4 Adank Cassie R. 75 7-Dec A-4 Adank William F. 76 24-Dec A-8 Adelman Irving D. 59 31-Oct D-10 Adelsperger Elizabeth A. 60 18-Mar A-8 Adelsperger Susanna T. 82 25-Oct A-7 Adoba Michael, Sr. 80 1-Jun A-12 Aeschliman Betty 32 18-Jan B-4 Aguirre Regina Avilla 63 4-Nov A-6 Ahlering Edward 6-Oct C-7 Ahley Lillian 15-Jun A-6 Also spelled Haley see June 16 E-2 Ahmed Hassan 68 13-Aug A-9 Akers Edward W. 66 16-Mar A-7 Aksentijevic Rodney 15 8-Jul 1 Alb Florence 70 1-Jun A-12, C-5 Gives name as Alb Florence on C-5 Albertson Jack R. 59 11-Jun C-2 Alexander Eugene A. 62 7-Jul C-8 Alexander L.C. 58 20-Aug B-3 Allen Cleo D. 66 26-Jan A-6 Allen Frosty 65 2-Dec B-6 Allen Grace 65 9-Nov B-3 Allen James Virgil 55 19-Aug A-4 Allen Weber 62 2-Mar A-4 Alley George Wesley 54 4-Jan A-5 Alonzo Maria 73 15-Oct B-5 Altshuller Nathan D. -

List of "Record of Ancestors" Charts Received by the Society up to October 2013
North of Ireland Family History Society List of "Record of Ancestors" Charts received by the Society up to October 2013 Members of the Society are encouraged to complete a Record of Ancestors Chart and send it to the Society. Record of Ancestors - Blank Form Surname Area Member No. ABBOTT Shane (Meath), Co. Leitrim & Mohill A3175 ABBOTT A2981 ABERNETHY Stewartstown, Arboe & Coalisland A3175 ABRAHAM London A2531 ABRAHAM Pettigo, Co. Donegal & Paisley A2145 ADAIR Gransha (Co. Down) & Ontario A2675 ADAMS Ballymena & Cloughwater B2202 ADAMS Coleraine B1435 ADAMS Rathkeel, Ballynalaird, Carnstroan, Ballyligpatrick B1751 ADAMS Carnmoney A2979 ADAMSON Great Yarmouth A2793 AIKEN A3187 AKENHEAD British Columbia, Canada & Northumberland A2693 ALDINGTEN Moreton Bagot A3314 ALEXANDER Co. Tyrone A2244 ALFORD Dublin South & Drogheda B2258 ALLAN Greenock A1720 ALLEN Belfast A0684 ALLEN Co. Down A3162 ALLEN Ballymena B2192 ALLEN County Wicklow & Carlisle, England B0817 ALLWOOD Birmingham B2281 ALTHOFER New South Wales & Denmark A3422 ANDERSON A3291 ANDERSON B0979 ANDERSON Greenock A1720 ANGUS A2693 ANGUS A3476 APPELBY Hull B1939 APPLEBY Cornwall B0412 ARBUCKLE A1459 ARCHER A0431 ARD Armagh A1579 ARLOW Co. Tyrone & Co. Tipperary A2872 ARMOUR Co. Limerick A1747 ARMSTRONG Belfast & Glasgow A0582 ARMSTRONG Omagh A0696 ARMSTRONG Belfast A1081 ARMSTRONG New Kilpatrick A1396 ARMSTRONG Aghalurcher & Colmon Island B0104 ARMSTRONG B0552 ARMSTRONG B0714 ARMSTRONG Co. Monaghan A1586 ARMSTRONG B1473 Surname Area Member No. ARMSTRONG Magheragall, Lisburn B2210 ARMSTRONG A3275 ARNOLD New York & Ontario A3434 ARNOLD Yorkshire B1939 ARTHUR Kells, Co. Antrim, Sydney Australia, Simla (India) & Glasgow A1389 ARTHUR Croghan and Lifford, Co. Donegal A1458 ARTHURS A1449 ARTHURS B0026 ARTT Cookstown A1773 ASHALL A0020 ASHBROOK Pennsylvania A3372 ASHE Greenhills, Convoy A0237 ATCHESON Donegore, Co. -

THE GARY MOORE DISCOGRAPHY (The GM Bible)
THE GARY MOORE DISCOGRAPHY (The GM Bible) THE COMPLETE RECORDING SESSIONS 1969 - 1994 Compiled by DDGMS 1995 1 IDEX ABOUT GARY MOORE’s CAREER Page 4 ABOUT THE BOOK Page 8 THE GARY MOORE BAND INDEX Page 10 GARY MOORE IN THE CHARTS Page 20 THE COMPLETE RECORDING SESSIONS - THE BEGINNING Page 23 1969 Page 27 1970 Page 29 1971 Page 33 1973 Page 35 1974 Page 37 1975 Page 41 1976 Page 43 1977 Page 45 1978 Page 49 1979 Page 60 1980 Page 70 1981 Page 74 1982 Page 79 1983 Page 85 1984 Page 97 1985 Page 107 1986 Page 118 1987 Page 125 1988 Page 138 1989 Page 141 1990 Page 152 1991 Page 168 1992 Page 172 1993 Page 182 1994 Page 185 1995 Page 189 THE RECORDS Page 192 1969 Page 193 1970 Page 194 1971 Page 196 1973 Page 197 1974 Page 198 1975 Page 199 1976 Page 200 1977 Page 201 1978 Page 202 1979 Page 205 1980 Page 209 1981 Page 211 1982 Page 214 1983 Page 216 1984 Page 221 1985 Page 226 2 1986 Page 231 1987 Page 234 1988 Page 242 1989 Page 245 1990 Page 250 1991 Page 257 1992 Page 261 1993 Page 272 1994 Page 278 1995 Page 284 INDEX OF SONGS Page 287 INDEX OF TOUR DATES Page 336 INDEX OF MUSICIANS Page 357 INDEX TO DISCOGRAPHY – Record “types” in alfabethically order Page 370 3 ABOUT GARY MOORE’s CAREER Full name: Robert William Gary Moore. Born: April 4, 1952 in Belfast, Northern Ireland and sadly died Feb. -

Jacob Gallagher Wsj
Jacob gallagher wsj Continue TVTVNocturnal Animal looks as dark and sexy as you expect. By Justin Fenner September 15, 2016 Watch MoreStyleStyleBy Jake Gallagher On January 2, 9, 2013View MoreStyleStyleBy Jake Gallagher 12 December 2012View MoreStyleBy Jake GallagherAAusgus 8, 2012View MoreStyleStyleBy Jake Gallagher25, 2012View MoreStyleBy Jake Gallagher 3, Jake Gallagher18, 2012View MoreStyleBy 2012View MoreStyleStyleBy Jake GallagherJuly 3, 2012View MoreStyleBy Jake Gallagher27 June 2012View MoreStyleBy Jake Gallagher13, 2012View MoreStyleBy Jake Gallagher 6, 2012View MoreStyleBy Jake GallagherJune 6, 2012View MoreStyleBy Jake Gallagher30, 2012 MoreViewStyleStyleStyleBy Jake Gallagher , 2012Watch MoreStyleStyleBy Jake GallagherMay 17, 2012View MoreStyleStyleBy Jake GallagherMay 9, 2012View MoreStyleStyleBy Jake GallagherMay 2, 2012View MoreStyleBy Jake Gallagher 17 2012View MoreStyleBy Jake Gallagher11 2012View More Skip the main contentIt comes as no surprise that the infamous cantankerous former Oasis frontman has opinions. Here are some of his favorite and least favorite things in life29 June 2011I love Judge Judy. And who the fuck is that black guy with a bald head? Montela. My wife and I love this shit. Also, I like that Celebrity Rehabilitation you have in America, too. I watched it on TV, and then I went out the night after that Marilyn Manson concert, and that guy from Grease with a cane -- what's his fucking name? Did he die a couple of weeks ago? (Jeff Conaway.) He was there and asked me if I wanted a line. I'm like, What the fuck? You're destined to be in fucking rehab. New York is my favorite city in the world. I don't do it downtown much, but I love Central Park.