Keratitis and Hyperopic Refractive Shift Induced by SLT
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

RFT List.Xlsx
RFT/Posters Last updated: May 7, 2019 RFT/Posters Session 2 Abstract Title Outcomes of Voretigene Neparvovec-rzyl for Leber Congenital Aaron Nagiel Amaurosis in Eleven Patients: The CHLA Experience AAV2/4-RS1 gene therapy in the retinoschisin knockout mouse Brittni Scruggs model of X-linked retinoschisis Fluorescence Lifetime Imaging Ophthalmoscopy (FLIO) in X-linked Alexandria Vitale retinoschisis RFT/Posters Session 3 Rajvardhan Azad Modified Staging System for FEVR Optical Coherence Tomography Measurements of Retinal and Nikisha Kothari Choroidal Thickness In Preterm Infants The Clinical course and progression of incontinentia pigmenti Charles Calvo retinopathy in treated and untreated patients RFT/Posters Session 7 Omar Moinuddin Patient Outcomes in Coats'-like Retinitis Pigmentosa Andrew Tsai Coats like response in Retinitis Pigmentosa Surgical Management of Advanced Coats' Disease - From Lauren Wright Beginning to End Effect of anti-VEGF therapy on persistent vascular leakage and Irina de la Huerta neovascularization in familial exudative vitreoretinopathy Rapid fire presentation A ROP Expert Confidence in Determining Plus Disease in Borderline Agnieshka Baumritter Images Mike Gaynon Prethreshold ROP - VEGF Inhibition Without VEGF Inhibitors Pre-treatment vs. Post-Treatment Optical Coherence Tomographic Robert Gunzenhauser Angiography in children with strabismic and anisometropic amblyopia. Progression from Pre-Plus Disease to Plus Disease in the G-ROP Alomi Parikh Study Practice patterns changes in the treatment of retinopathy -

HHS Public Access Author Manuscript
HHS Public Access Author manuscript Author Manuscript Author ManuscriptOphthalmology Author Manuscript. Author Author Manuscript manuscript; available in PMC 2016 December 01. Published in final edited form as: Ophthalmology. 2015 December ; 122(12): 2373–2379. doi:10.1016/j.ophtha.2015.06.013. Ability of bottle cap color to facilitate accurate glaucoma patient- physician communication regarding medication identity Pujan Dave, BA1, Guadalupe Villarreal Jr., MD1, David S. Friedman, MD, PhD1, Malik Y. Kahook, MD2, and Pradeep Y. Ramulu, MD, PhD1 1Wilmer Eye Institute, Johns Hopkins University, Baltimore, Maryland 2Department of Ophthalmology, University of Colorado School of Medicine, Aurora, Colorado Abstract Objective—To determine the accuracy of patient-physician communication regarding topical ophthalmic medication use based on bottle cap color, particularly amongst individuals who may have acquired color vision deficiency from glaucoma. Design—Cross-sectional, clinical study. Participants—Patients ≥ 18 years old with primary open-angle, primary angle-closure, pseudoexfoliation, or pigment dispersion glaucoma, bilateral visual acuity of 20/400 or better, and no concurrent conditions that may affect color vision. Methods—One hundred patients provided color descriptions of 11 distinct medication bottle caps. Patient-produced color descriptors were then presented to three physicians. Each physician matched each color descriptor to the medication they thought the descriptor was describing. Main Outcome Measures—Frequency of patient-physician agreement, occurring when all three physicians accurately matched the patient-produced color descriptor to the correct medication. Multivariate regression models evaluated whether patient-physician agreement decreased with degree of better-eye visual field (VF) damage, color descriptor heterogeneity, and/or color vision deficiency, as determined by Hardy-Rand-Rittler (HRR) score and the Lanthony D15 testing index (D15 CCI). -

Short-Term Changes in the Photopic Negative Response Following Intraocular Pressure Lowering in Glaucoma
Glaucoma Short-Term Changes in the Photopic Negative Response Following Intraocular Pressure Lowering in Glaucoma Jessica Tang,1,2 Flora Hui,1 Xavier Hadoux,1 Bernardo Soares,3 Michael Jamieson,3 Peter van Wijngaarden,1–3 Michael Coote,1–3 and Jonathan G. Crowston1,2,4,5 1Glaucoma Research Unit, Centre for Eye Research Australia, Royal Victorian Eye and Ear Hospital, Melbourne, Australia 2Ophthalmology, Department of Surgery, The University of Melbourne, Melbourne, Australia 3Royal Victorian Eye and Ear Hospital, Melbourne, Australia 4Centre for Vision Research, Duke-NUS Medical School, Singapore, Singapore 5Singapore Eye Research Institute, Singapore National Eye Centre, Singapore, Singapore Correspondence: Jessica Tang, PURPOSE. To evaluate the short-term changes in inner retinal function using the photopic Glaucoma Research Unit, Centre for negative response (PhNR) after intraocular pressure (IOP) reduction in glaucoma. Eye Research Australia, Royal Victorian Eye and Ear Hospital, METHODS. Forty-seven participants with glaucoma who were commencing a new or addi- Level 7, Peter Howson Wing, 32 tional IOP-lowering therapy (treatment group) and 39 participants with stable glau- Gisborne St, East Melbourne, VIC coma (control group) were recruited. IOP, visual field, retinal nerve fiber layer thick- 3002, Australia; ness, and electroretinograms (ERGs) were recorded at baseline and at a follow-up visit [email protected]. (3 ± 2 months). An optimized protocol developed for a portable ERG device was used Received: August 29, 2019 to record the PhNR. The PhNR saturated amplitude (Vmax), Vmax ratio, semi-saturation Accepted: June 16, 2020 constant (K), and slope of the Naka–Rushton function were analyzed. Published: August 7, 2020 RESULTS. -
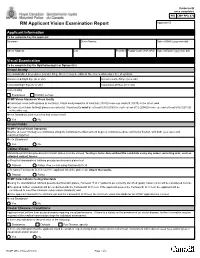
RCMP GRC 2180E (2017-10) Page 1 of 2 Protected B RM Applicant Vision Examination Report Once Completed Applicant ID
Protected B once completed PIB CMP PPU 070 RM Applicant Vision Examination Report Applicant ID Applicant Information To be completed by the applicant Surname Given Names Date of Birth (yyyy-mm-dd) Street Address City Province Postal Code (A9A 9A9) Date of Exam (yyyy-mm-dd) Visual Examination To be completed by the Ophthalmologist or Optometrist Visual Acuity Any standardized procedures (Landoit Ring, Snellen) may be utilized. No error is allowed per line of symbols. Uncorrected Right Eye (6/ or 20/) Uncorrected Left Eye (6/ or 20/) Corrected Right Eye (6/ or 20/) Corrected Left Eye (6/ or 20/) Corrected by Eyeglasses Contact Lenses RCMP Vision Standards Visual Acuity Corrected vision (with glasses or contacts): Visual acuity must be at least 6/6 (20/20) in one eye and 6/9 (20/30) in the other; and Uncorrected vision (without glasses or contacts): Visual acuity must be at least 6/18 (20/60) in each eye or 6/12 (20/40) in one eye and at least 6/30 (20/100) in the other eye. Meets Standards, both corrected and uncorrected? Yes No Visual Fields RCMP Field of Vision Standards Must be at least 150 degrees continuous along the horizontal meridian and 20 degrees continuous above and below fixation, with both eyes open and examined together. Meets Standards? Yes No Colour-Vision Standardized Ishihara pseudo-isochromatic plates must be utilized. Testing is to be done without the candidate using any colour correcting aids, such as coloured contact lenses. a) Result of standardized Ishihara pseudo-isochromatic plates test Passed Failed. If so, re-test using Farnsworth D-15. -

Modern Laser in Situ Keratomileusis Outcomes
REVIEW/UPDATE Modern laser in situ keratomileusis outcomes Helga P. Sandoval, MD, MSCR, Eric D. Donnenfeld, MD, Thomas Kohnen, MD, PhD, FEBO, Richard L. Lindstrom, MD, Richard Potvin, OD, David M. Tremblay, MD, Kerry D. Solomon, MD Laser in situ keratomileusis (LASIK) articles published between 2008 and 2015 that contain clin- ical outcomes data were reviewed and graded for quality, impression, and potential bias. All 97 relevant articles (representing 67 893 eyes) provided a positive or neutral impression of LASIK. Industry bias was not evident. The aggregate loss of 2 or more lines of corrected distance visual acuity was 0.61% (359/58 653). The overall percentage of eyes with uncorrected distance visual acuity better than 20/40 was 99.5% (59 503/59 825). The spherical equivalent refraction was within G1.0 diopter (D) of the target refraction in 98.6% (59 476/60 329) of eyes, with 90.9% (59 954/65 974) within G0.5 D. In studies reporting patient satisfaction, 1.2% (129/9726) of pa- tients were dissatisfied with LASIK. Aggregate outcomes appear better than those reported in summaries of the safety and effectiveness of earlier laser refractive surgery systems approved by the U.S. Food and Drug Administration. Modern results support the safety, efficacy, and patient satisfaction of the procedure. Financial Disclosure: Proprietary or commercial disclosures are listed after the references. J Cataract Refract Surg 2016; 42:1224–1234 Q 2016 ASCRS and ESCRS Laser in situ keratomileusis (LASIK) is one of the most have been performed globally.1 Laser in situ keratomil- commonly performed elective procedures in the United eusis was introduced by Pallikaris et al.2 in 1990. -

Laser Learning Lecture and Lab: YAG Caps, LPI, And
5/9/17 Overview Laser Learning Lecture and Lab: • Why we use lasers YAG caps, LPI, and SLT • YAG capsulotomy • Laser Peripheral Iridotomy (LPI or PI) Aaron McNulty, O.D., F.A.A.O. • Argon Laser Peripheral Iridoplasty (ALPI) Nate Lighthizer, O.D., F.A.A.O. • Argon Laser Trabeculoplasty (ALT) • Selective Laser Trabeculoplasty (SLT) • Other Laser Trabeculoplasty Why do we use lasers? Posterior Capsular Opacification (PCO) • Vision is decreased from PCO following cataract surgery • Lens capsular bag has an anterior and • Narrow angles/angle closure posterior surface • Glaucoma is progressing in a pt on max meds – Anterior surface usually removed w/ capsulorhexis – Something else needs to be done – Surgery not wanted yet • PCO is the formation of a cloudy membrane • Compliance issues on the posterior surface of the capsular bag • Cost issues following ECCE • Convenience issues – AKA: Secondary cataract • Doctor preference PCO YAG Laser • Incidence: • Nd: YAG laser – Most common complication of post ECCE – Neodymium: Yttrium aluminum garnet laser – 10-80% of eyes following cataract surgery – Can form anywhere from a few days to years post surgery • Tissue interaction: Photodisruptive laser – Younger patients higher risk of PCO – High light energy levels cause the tissues to be reduced – IOL’s to plasma, disintegrating the tissue • Silicone > acrylic – A large amount of energy is delivered into very small focal spots in a very brief duration of time • Prevention: • 4 nsec – – Capsulotomy during surgery No thermal reaction/No coagulation when bv’s are hit – Posterior capsular polishing – Pigment independent* 1 5/9/17 YAG Cap Risks, Complications, YAG Cap Pre-op Exam Contraindications • Visual acuity, glare testing, PAM/Heine lambda Contraindications Risks/complications – Vision 20/30 or worse 1. -

Early Postoperative Rotational Stability and Its Related Factors of a Single-Piece Acrylic Toric Intraocular Lens
Eye (2020) 34:474–479 https://doi.org/10.1038/s41433-019-0521-0 ARTICLE Early Postoperative Rotational stability and its related factors of a single-piece acrylic toric intraocular lens 1,2 3 4 5 1 1 1 Shuyi Li ● Xi Li ● Suhong He ● Qianyin Zheng ● Xiang Chen ● Xingdi Wu ● Wen Xu Received: 30 November 2018 / Accepted: 18 June 2019 / Published online: 12 July 2019 © The Author(s) 2019. This article is published with open access Abstract Purpose In the present study, we aimed to evaluate the early postoperative rotational stability of TECNIS toric intraocular lens (IOL) and analyse its correlation with preoperative and intraoperative parameters. Methods A total of 102 eyes from 87 cataract patients who underwent implantation of TECNIS toric IOL during July 2016 to November 2017 were enrolled in this retrospective study. Preoperative parameters including corneal astigmatism, axial length (AL), lens thickness (LT), anterior chamber depth (ACD) and sulcus-to-sulcus (STS), were determined. The area of capsulorhexis was measured with Rhinoceros 5.0 software. The follow-up examinations including the residual astigmatism (RAS) and postoperative toric IOL axis, were performed at 1 month and 3 months after surgery. − − 1234567890();,: 1234567890();,: Results RAS was 0.84 ± 0.88 D at 1 month and 0.81 ± 0.89 D at 3 months after surgery. The rotation of toric IOL at 3 months was 4.83 ± 3.65°. The Pearson’s r of ACD, horizontal and vertical STS, and toric IOL target axis was 0.011, 0.039, 0.045 and 0.082. The toric IOL rotation was positively correlated with the area of capsulorhexis (r = 0.522, P = 0.0003), LT (r = 0.288, P = 0.003) and AL (r = 0.259, P = 0.009). -

Laser Procedures for the Management of Glaucoma and More Handout
4/25/17 Overview Laser Procedures for the Management • Why we use lasers of Glaucoma and More • YAG capsulotomy Nate Lighthizer, O.D., F.A.A.O. • Laser Peripheral Iridotomy (LPI or PI) Assistant Professor, NSUOCO • Argon Laser Peripheral Iridoplasty (ALPI) Assistant Dean, Clinical Care Services • Argon Laser Trabeculoplasty (ALT) Director of CE Chief of Specialty Care Clinics • Selective Laser Trabeculoplasty (SLT) Chief of Electrodiagnostics Clinic • Other Laser Trabeculoplasty [email protected] Why do we use lasers? Posterior Capsular Opacification (PCO) • Vision is decreased from PCO following cataract surgery • Lens capsular bag has an anterior and • Narrow angles/angle closure posterior surface • Glaucoma is progressing in a pt on max meds – Anterior surface usually removed w/ capsulorhexis – Something else needs to be done – Surgery not wanted yet • PCO is the formation of a cloudy membrane • Compliance issues on the posterior surface of the capsular bag • Cost issues following ECCE • Convenience issues – AKA: Secondary cataract • Doctor preference PCO YAG Laser • Incidence: • Nd: YAG laser – Most common complication of post ECCE – Neodymium: Yttrium aluminum garnet laser – 10-80% of eyes following cataract surgery – Can form anywhere from a few days to years post surgery • Tissue interaction: Photodisruptive laser – Younger patients higher risk of PCO – High light energy levels cause the tissues to be reduced – IOL’s to plasma, disintegrating the tissue • Silicone > acrylic – A large amount of energy is delivered into very small focal spots in a very brief duration of time • Prevention: • 4 nsec – – Capsulotomy during surgery No thermal reaction/No coagulation when bv’s are hit – Posterior capsular polishing – Pigment independent* 1 4/25/17 YAG Cap Risks, Complications, YAG Cap Pre-op Exam Contraindications • Visual acuity, glare testing, PAM/Heine lambda Contraindications Risks/complications – Vision 20/30 or worse 1. -

Bjophthalmol-2020-318090 1..2
At a glance Br J Ophthalmol: first published as 10.1136/bjophthalmol-2020-318090 on 26 October 2020. Downloaded from Highlights from this issue doi:10.1136/bjophthalmol-2020-318090 Keith Barton , James Chodosh , Jost B Jonas , Editors in chief Glaucoma in the Northern Ireland Cohort The effect of partial posterior vitreous Comparison of OCT angiography in for the Longitudinal Study of Ageing detachment on spectral-domain optical children with a history of intravitreal (NICOLA): cohort profile, prevalence, coherence tomography retinal nerve fibre injection of ranibizumab vs laser awareness and associations (seepage1492) layer thickness measurements photocoagulation for retinopathy of The crude prevalence of glaucoma in (seepage1524) prematurity (see page 1556) Northern Ireland of 2.83% (95% CI Among glaucoma suspects, eyes with par- In this cross-sectional study, we found that 2.31%, 3.46%) is comparable to other tial posterior vitreous detachments, com- the central foveal vessel length density and European population-based studies. pared to eyes without, were associated perfusion density, the foveal avascular Approximately two thirds of people with with greater average, superior, and inferior zone area and central foveal thicknesses glaucoma were undiagnosed. Associations retinal nerve fibre layer thickness of children who had undergone different with glaucoma were consistent with cur- measurements. treatments, might vary. rent understanding of the disease. Three-year follow-up of choroidal Comparison of central visual sensitivity Selective -

Ophthalmology Abbreviations Alphabetical
COMMON OPHTHALMOLOGY ABBREVIATIONS Listed as one of America’s Illinois Eye and Ear Infi rmary Best Hospitals for Ophthalmology UIC Department of Ophthalmology & Visual Sciences by U.S.News & World Report Commonly Used Ophthalmology Abbreviations Alphabetical A POCKET GUIDE FOR RESIDENTS Compiled by: Bryan Kim, MD COMMON OPHTHALMOLOGY ABBREVIATIONS A/C or AC anterior chamber Anterior chamber Dilators (red top); A1% atropine 1% education The Department of Ophthalmology accepts six residents Drops/Meds to its program each year, making it one of nation’s largest programs. We are anterior cortical changes/ ACC Lens: Diagnoses/findings also one of the most competitive with well over 600 applicants annually, of cataract whom 84 are granted interviews. Our selection standards are among the Glaucoma: Diagnoses/ highest. Our incoming residents graduated from prestigious medical schools ACG angle closure glaucoma including Brown, Northwestern, MIT, Cornell, University of Michigan, and findings University of Southern California. GPA’s are typically 4.0 and board scores anterior chamber intraocular ACIOL Lens are rarely lower than the 95th percentile. Most applicants have research lens experience. In recent years our residents have gone on to prestigious fellowships at UC Davis, University of Chicago, Northwestern, University amount of plus reading of Iowa, Oregon Health Sciences University, Bascom Palmer, Duke, UCSF, Add power (for bifocal/progres- Refraction Emory, Wilmer Eye Institute, and UCLA. Our tradition of excellence in sives) ophthalmologic education is reflected in the leadership positions held by anterior ischemic optic Nerve/Neuro: Diagno- AION our alumni, who serve as chairs of ophthalmology departments, the dean neuropathy ses/findings of a leading medical school, and the director of the National Eye Institute. -

A Review of Selective Laser Trabeculoplasty: Recent Findings and Current Perspectives
Ophthalmol Ther DOI 10.1007/s40123-017-0082-x REVIEW A Review of Selective Laser Trabeculoplasty: Recent Findings and Current Perspectives Yujia Zhou . Ahmad A. Aref Received: January 17, 2017 Ó The Author(s) 2017. This article is published with open access at Springerlink.com ABSTRACT explored, revealing that minor modifications may lead to a more favorable or safer clinical Selective laser trabeculoplasty (SLT) has been outcome. The utilization of postoperative widely used in the clinical management of medications remains controversial based on the glaucoma, both as primary and adjunctive current evidence. A short-term IOP increase treatment. As new evidence continues to arise, may complicate SLT and can also persist in we review the current literature in terms of certain cases such as in exfoliation glaucoma. indications and efficacy, surgical technique, The efficacy and safety of repeat SLT are shown postoperative care, repeatability, and compli- in multiple studies, and the timing of repeat cations of this therapy. SLT has been shown to procedures may affect the success rate. be effective in various glaucomas, including primary open-angle glaucoma (POAG), nor- mal-tension glaucoma (NTG), steroid-induced Keywords: Glaucoma; Intraocular pressure; glaucoma, pseudoexfoliation glaucoma (PXFG), Laser; Selective laser trabeculoplasty and primary angle-closure glaucoma (PACG), as well as other glaucoma subtypes. Relatively high preoperative intraocular pressure (IOP) INTRODUCTION may predict surgical success, while other parameters that have been studied do not seem Intraocular pressure (IOP) reduction is the to affect the outcome. Different techniques for mainstay of therapy for glaucomatous optic performing the procedure have recently been neuropathy. Selective laser trabeculoplasty (SLT) has been widely employed for this pur- Enhanced content To view enhanced content for this pose over the past several years as both a pri- article go to http://www.medengine.com/Redeem/ mary and adjunctive treatment [1]. -

Acquired Colour Vision Defects in Glaucoma—Their Detection and Clinical Significance
1396 Br J Ophthalmol 1999;83:1396–1402 Br J Ophthalmol: first published as 10.1136/bjo.83.12.1396 on 1 December 1999. Downloaded from PERSPECTIVE Acquired colour vision defects in glaucoma—their detection and clinical significance Mireia Pacheco-Cutillas, Arash Sahraie, David F Edgar Colour vision defects associated with ocular disease have The aims of this paper are: been reported since the 17th century. Köllner1 in 1912 + to provide a review of the modern literature on acquired wrote an acute description of the progressive nature of col- colour vision in POAG our vision loss secondary to ocular disease, dividing defects + to diVerentiate the characteristics of congenital and into “blue-yellow” and “progressive red-green blindness”.2 acquired defects, in order to understand the type of This classification has become known as Köllner’s rule, colour vision defect associated with glaucomatous although it is often imprecisely stated as “patients with damage retinal disease develop blue-yellow discrimination loss, + to compare classic clinical and modern methodologies whereas optic nerve disease causes red-green discrimina- (including modern computerised techniques) for tion loss”. Exceptions to Köllner’s rule34 include some assessing visual function mediated through chromatic optic nerve diseases, notably glaucoma, which are prima- mechanisms rily associated with blue-yellow defects, and also some reti- + to assess the eVects of acquired colour vision defects on nal disorders such as central cone degeneration which may quality of life in patients with POAG. result in red-green defects. Indeed, in some cases, there might be a non-specific chromatic loss. Comparing congenital and acquired colour vision Colour vision defects in glaucoma have been described defects since 18835 and although many early investigations Congenital colour vision deficiencies result from inherited indicated that red-green defects accompanied glaucoma- cone photopigment abnormalities.