Vitreoretinal Surgery for Macular Hole After Laser Assisted in Situ
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
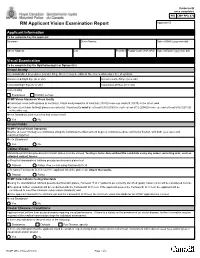
RCMP GRC 2180E (2017-10) Page 1 of 2 Protected B RM Applicant Vision Examination Report Once Completed Applicant ID
Protected B once completed PIB CMP PPU 070 RM Applicant Vision Examination Report Applicant ID Applicant Information To be completed by the applicant Surname Given Names Date of Birth (yyyy-mm-dd) Street Address City Province Postal Code (A9A 9A9) Date of Exam (yyyy-mm-dd) Visual Examination To be completed by the Ophthalmologist or Optometrist Visual Acuity Any standardized procedures (Landoit Ring, Snellen) may be utilized. No error is allowed per line of symbols. Uncorrected Right Eye (6/ or 20/) Uncorrected Left Eye (6/ or 20/) Corrected Right Eye (6/ or 20/) Corrected Left Eye (6/ or 20/) Corrected by Eyeglasses Contact Lenses RCMP Vision Standards Visual Acuity Corrected vision (with glasses or contacts): Visual acuity must be at least 6/6 (20/20) in one eye and 6/9 (20/30) in the other; and Uncorrected vision (without glasses or contacts): Visual acuity must be at least 6/18 (20/60) in each eye or 6/12 (20/40) in one eye and at least 6/30 (20/100) in the other eye. Meets Standards, both corrected and uncorrected? Yes No Visual Fields RCMP Field of Vision Standards Must be at least 150 degrees continuous along the horizontal meridian and 20 degrees continuous above and below fixation, with both eyes open and examined together. Meets Standards? Yes No Colour-Vision Standardized Ishihara pseudo-isochromatic plates must be utilized. Testing is to be done without the candidate using any colour correcting aids, such as coloured contact lenses. a) Result of standardized Ishihara pseudo-isochromatic plates test Passed Failed. If so, re-test using Farnsworth D-15. -

Modern Laser in Situ Keratomileusis Outcomes
REVIEW/UPDATE Modern laser in situ keratomileusis outcomes Helga P. Sandoval, MD, MSCR, Eric D. Donnenfeld, MD, Thomas Kohnen, MD, PhD, FEBO, Richard L. Lindstrom, MD, Richard Potvin, OD, David M. Tremblay, MD, Kerry D. Solomon, MD Laser in situ keratomileusis (LASIK) articles published between 2008 and 2015 that contain clin- ical outcomes data were reviewed and graded for quality, impression, and potential bias. All 97 relevant articles (representing 67 893 eyes) provided a positive or neutral impression of LASIK. Industry bias was not evident. The aggregate loss of 2 or more lines of corrected distance visual acuity was 0.61% (359/58 653). The overall percentage of eyes with uncorrected distance visual acuity better than 20/40 was 99.5% (59 503/59 825). The spherical equivalent refraction was within G1.0 diopter (D) of the target refraction in 98.6% (59 476/60 329) of eyes, with 90.9% (59 954/65 974) within G0.5 D. In studies reporting patient satisfaction, 1.2% (129/9726) of pa- tients were dissatisfied with LASIK. Aggregate outcomes appear better than those reported in summaries of the safety and effectiveness of earlier laser refractive surgery systems approved by the U.S. Food and Drug Administration. Modern results support the safety, efficacy, and patient satisfaction of the procedure. Financial Disclosure: Proprietary or commercial disclosures are listed after the references. J Cataract Refract Surg 2016; 42:1224–1234 Q 2016 ASCRS and ESCRS Laser in situ keratomileusis (LASIK) is one of the most have been performed globally.1 Laser in situ keratomil- commonly performed elective procedures in the United eusis was introduced by Pallikaris et al.2 in 1990. -

Early Postoperative Rotational Stability and Its Related Factors of a Single-Piece Acrylic Toric Intraocular Lens
Eye (2020) 34:474–479 https://doi.org/10.1038/s41433-019-0521-0 ARTICLE Early Postoperative Rotational stability and its related factors of a single-piece acrylic toric intraocular lens 1,2 3 4 5 1 1 1 Shuyi Li ● Xi Li ● Suhong He ● Qianyin Zheng ● Xiang Chen ● Xingdi Wu ● Wen Xu Received: 30 November 2018 / Accepted: 18 June 2019 / Published online: 12 July 2019 © The Author(s) 2019. This article is published with open access Abstract Purpose In the present study, we aimed to evaluate the early postoperative rotational stability of TECNIS toric intraocular lens (IOL) and analyse its correlation with preoperative and intraoperative parameters. Methods A total of 102 eyes from 87 cataract patients who underwent implantation of TECNIS toric IOL during July 2016 to November 2017 were enrolled in this retrospective study. Preoperative parameters including corneal astigmatism, axial length (AL), lens thickness (LT), anterior chamber depth (ACD) and sulcus-to-sulcus (STS), were determined. The area of capsulorhexis was measured with Rhinoceros 5.0 software. The follow-up examinations including the residual astigmatism (RAS) and postoperative toric IOL axis, were performed at 1 month and 3 months after surgery. − − 1234567890();,: 1234567890();,: Results RAS was 0.84 ± 0.88 D at 1 month and 0.81 ± 0.89 D at 3 months after surgery. The rotation of toric IOL at 3 months was 4.83 ± 3.65°. The Pearson’s r of ACD, horizontal and vertical STS, and toric IOL target axis was 0.011, 0.039, 0.045 and 0.082. The toric IOL rotation was positively correlated with the area of capsulorhexis (r = 0.522, P = 0.0003), LT (r = 0.288, P = 0.003) and AL (r = 0.259, P = 0.009). -

Ophthalmology Abbreviations Alphabetical
COMMON OPHTHALMOLOGY ABBREVIATIONS Listed as one of America’s Illinois Eye and Ear Infi rmary Best Hospitals for Ophthalmology UIC Department of Ophthalmology & Visual Sciences by U.S.News & World Report Commonly Used Ophthalmology Abbreviations Alphabetical A POCKET GUIDE FOR RESIDENTS Compiled by: Bryan Kim, MD COMMON OPHTHALMOLOGY ABBREVIATIONS A/C or AC anterior chamber Anterior chamber Dilators (red top); A1% atropine 1% education The Department of Ophthalmology accepts six residents Drops/Meds to its program each year, making it one of nation’s largest programs. We are anterior cortical changes/ ACC Lens: Diagnoses/findings also one of the most competitive with well over 600 applicants annually, of cataract whom 84 are granted interviews. Our selection standards are among the Glaucoma: Diagnoses/ highest. Our incoming residents graduated from prestigious medical schools ACG angle closure glaucoma including Brown, Northwestern, MIT, Cornell, University of Michigan, and findings University of Southern California. GPA’s are typically 4.0 and board scores anterior chamber intraocular ACIOL Lens are rarely lower than the 95th percentile. Most applicants have research lens experience. In recent years our residents have gone on to prestigious fellowships at UC Davis, University of Chicago, Northwestern, University amount of plus reading of Iowa, Oregon Health Sciences University, Bascom Palmer, Duke, UCSF, Add power (for bifocal/progres- Refraction Emory, Wilmer Eye Institute, and UCLA. Our tradition of excellence in sives) ophthalmologic education is reflected in the leadership positions held by anterior ischemic optic Nerve/Neuro: Diagno- AION our alumni, who serve as chairs of ophthalmology departments, the dean neuropathy ses/findings of a leading medical school, and the director of the National Eye Institute. -

Diagnosis and Treatment of Neurotrophic Keratopathy
An Evidence-based Approach to the Diagnosis and Treatment of Neurotrophic Keratopathy ACTIVITY DIRECTOR A CME MONOGRAPH Esen K. Akpek, MD This monograph was published by Johns Hopkins School of Medicine in partnership Wilmer Eye Institute with Catalyst Medical Education, LLC. It is Johns Hopkins School of Medicine not affiliated with JAMA medical research Baltimore, Maryland publishing. Visit catalystmeded.com/NK for online testing to earn your CME credit. FACULTY Natalie Afshari, MD Mina Massaro-Giordano, MD Shiley Eye Institute University of Pennsylvania School of Medicine University of California, San Diego Philadelphia, Pennsylvania La Jolla, California Nakul Shekhawat, MD, MPH Sumayya Ahmad, MD Wilmer Eye Institute Mount Sinai School of Medicine Johns Hopkins School of Medicine New York, New York Baltimore, Maryland Pedram Hamrah, MD, FRCS, FARVO Christopher E. Starr, MD Tufts University School of Medicine Weill Cornell Medical College Boston, Massachusetts New York, New York ACTIVITY DIRECTOR FACULTY Esen K. Akpek, MD Natalie Afshari, MD Mina Massaro-Giordano, MD Professor of Ophthalmology Professor of Ophthalmology Professor of Clinical Ophthalmology Director, Ocular Surface Diseases Chief of Cornea and Refractive Surgery University of Pennsylvania School and Dry Eye Clinic Vice Chair of Education of Medicine Wilmer Eye Institute Fellowship Program Director of Cornea Philadelphia, Pennsylvania Johns Hopkins School of Medicine and Refractive Surgery Baltimore, Maryland Shiley Eye Institute Nakul Shekhawat, MD, MPH University of California, -

Endoscopic Vitreoretinal Surgery: Principles, Applications and New Directions Radwan S
Ajlan et al. Int J Retin Vitr (2019) 5:15 International Journal https://doi.org/10.1186/s40942-019-0165-z of Retina and Vitreous REVIEW Open Access Endoscopic vitreoretinal surgery: principles, applications and new directions Radwan S. Ajlan1*, Aarsh A. Desai2 and Martin A. Mainster1 Abstract Purpose: To analyze endoscopic vitreoretinal surgery principles, applications, challenges and potential technological advances. Background: Microendoscopic imaging permits vitreoretinal surgery for tissues that are not visible using operat- ing microscopy ophthalmoscopy. Evolving instrumentation may overcome some limitations of current endoscopic technology. Analysis: Transfer of the fine detail in endoscopic vitreoretinal images to extraocular video cameras is constrained currently by the caliber limitations of intraocular probes in ophthalmic surgery. Gradient index and Hopkins rod lenses provide high resolution ophthalmoscopy but restrict surgical manipulation. Fiberoptic coherent image guides offer surgical maneuverability but reduce imaging resolution. Coaxial endoscopic illumination can highlight delicate vitreo- retinal structures difficult to image in chandelier or endoilluminator diffuse, side-scattered lighting. Microendoscopy’s ultra-high magnification video monitor images can reveal microscopic tissue details blurred partly by ocular media aberrations in contemporary surgical microscope ophthalmoscopy, thereby providing a lower resolution, invasive alternative to confocal fundus imaging. Endoscopic surgery is particularly useful when ocular -

Visual Outcome of Pars Plana Vitrectomy Following Endophthalmitis – a Vitreo-Retinal Surgeon's Experience
Medical Journal of Zambia, Vol. 47 (1): 33 - 38 (2020) Original Article Visual outcome of Pars Plana Vitrectomy following Endophthalmitis – A Vitreo-retinal Surgeon's Experience Sanjoy K. Das1 ,Osayem J. Otabor-Olubor2, Situma P Wanyama1 1Ispahani Islamia Eye Institute and Hospital (IIEIH), Dhaka, Bangladesh 2Ispahani Islamia Eye Institute and Hospital (IIEIH), Dhaka, Bangladesh1 and University of Benin Teaching Hospital (UBTH), Benin City, Nigeria. ABSTRACT (p-value = 0.007). There was an association (although not strong) between age range and post- Purpose: To determine the visual outcome of pars operative visual improvement (p-value = 0.639). plana vitrectomy following endophthalmitis. Conclusion: Pars plana vitrectomy helps to prevent Methods: A retrospective hospital-based study of 20 or minimize ophthalmic complications from eyes of consecutive patients who had pars plana endophthalmitis, thus making it a necessary line of vitrectomy by a particular surgeon following treatment endophthalmitis. Pars plana vitrectomy is endophthalmitis in the Ispahani Islamia Eye therefore a safe and desirable definitive treatment Institute and Hospital, Dhaka, Bangladesh from for endophthalmitis, and it confers a good chance of August – December 2017. Using the Snellen's visual visual improvement. acuity chart, post-operative distant visual acuity improvement was graded 0– 9, with 0 meaning no INTRODUCTION improvement in visual acuity, and 9 meaning nine Pars plana vitrectomy (the intricate surgical removal lines of improvement in visual acuity from of vitreous gel from the vitreous cavity) has seen presenting best corrected visual acuity. remarkable progress in surgical technique and post- Results: Pre-operative corrected distant visual operative outcome in ophthalmic practices all over acuity (CDVA) ranged from perception of light to the world. -

Medical Treatment of Operative Corneal Perforation Caused By
CASE REPORTS AND SMALL CASE SERIES and clinical course of a patient with the stromal bed was thin; in the left Medical Treatment a LASIK-induced corneal perfora- eye, the corneal flap was very edema- of Operative Corneal tion that affected the final visual acu- tous and a space was visible between Perforation Caused ity. We believe that this report on the the corneal flap and the stromal bed treatment and recovery of the cor- (Figure 1, left). The anterior cham- by Laser In Situ neal perforation will be valuable in- ber was very shallow, and aqueous Keratomileusis formation for refractive surgeons. humor was observed to leak onto the ocular surface with blinking (Figure Laser in situ keratomileusis (LASIK) Report of a Case. A 33-year-old man 1, right). A round, 0.25-mm diam- is an effective procedure to treat a was referred to us with a complaint eter perforation site was observed in wide range of myopia.1 The advan- of decreased visual acuity in the left the center of the stromal bed by slit- tages of LASIK over photorefrac- eye after bilateral simultaneous lamp examination. tive keratectomy (PRK) are rapid vi- LASIK performed 3 days previ- We treated the corneal perfo- sual recovery, lower risk of corneal ously at a different facility. A cor- ration by applying a therapeutic soft haze, greater regression of myopia, neal perforation was noticed in the contact lens with topical antibiot- and less postoperative pain.1-3 How- left eye during LASIK laser abla- ics, oral carbonic anhydrase inhibi- ever, LASIK requires more skillful tion in this eye. -

Visual Field Changes After Vitrectomy with Internal Limiting Membrane Peeling for Epiretinal Membrane Or Macular Hole in Glaucomatous Eyes
RESEARCH ARTICLE Visual field changes after vitrectomy with internal limiting membrane peeling for epiretinal membrane or macular hole in glaucomatous eyes Shunsuke Tsuchiya, Tomomi Higashide*, Kazuhisa Sugiyama Department of Ophthalmology, Kanazawa University Graduate School of Medical Science, Kanazawa, Japan * [email protected] a1111111111 a1111111111 a1111111111 Abstract a1111111111 a1111111111 Purpose To investigate visual field changes after vitrectomy for macular diseases in glaucomatous eyes. OPEN ACCESS Citation: Tsuchiya S, Higashide T, Sugiyama K Methods (2017) Visual field changes after vitrectomy with internal limiting membrane peeling for epiretinal A retrospective review of 54 eyes from 54 patients with glaucoma, who underwent vitrectomy membrane or macular hole in glaucomatous eyes. for epiretinal membrane (ERM; 42 eyes) or macular hole (MH; 12 eyes). Standard automated PLoS ONE 12(5): e0177526. https://doi.org/ perimetry (Humphrey visual field 24±2 program) was performed and analyzed preoperatively 10.1371/journal.pone.0177526 and twice postoperatively (1st and 2nd sessions; 4.7 ± 2.5, 10.3 ± 3.7 months after surgery, Editor: Demetrios G. Vavvas, Massachusetts Eye & respectively). Postoperative visual field sensitivity at each test point was compared with the Ear Infirmary, Harvard Medical School, UNITED STATES preoperative value. Longitudinal changes in mean visual field sensitivity (MVFS) of the 12 test points within 10Ê eccentricity (center) and the remaining test points (periphery), best-cor- Received: October 29, 2016 rected visual acuity (BCVA), intraocular pressure (IOP), and ganglion cell complex (GCC) Accepted: April 29, 2017 thickness, and the association of factors with changes in central or peripheral MVFS over Published: May 18, 2017 time were analyzed using linear mixed-effects models. -

Comprehensive Strategies for Unplanned Vitrectomy for the Anterior Segment Surgeon
Supplement to January 2012 When the Room Gets Quiet Comprehensive strategies for unplanned vitrectomy for the anterior segment surgeon. A monograph and DVD based on the live surgery course given by Lisa B. Arbisser, MD. PLUS: A DVD OF SURGICAL VIDEOS AND A DIGITAL VERSION AVAILABLE AT EYETUBE.NET When the Room Gets Quiet An Ounce of Prevention All ophthalmic surgeons must have a comprehensive strategy for managing surgical complications. Many opinions and recommendations exist for handling complicated cataract surgeries. This monograph contains mine. I was trained as a comprehensive ophthalmologist, and for many years I performed scleral buckles, tra- beculectomy, and penetrating keratoplasty before con- centrating on cataract surgery and anterior segment reconstruction. The strategies I have developed for man- aging complex and complicated cataracts over decades of practice are enhanced by close collaboration with retinal surgeons as well as laboratory exploration. I hope this information will help you to organize your thoughts and have a cogent strategy at hand for ‘when the room gets quiet.’ An unplanned vitrectomy. —Lisa B. Arbisser, MD To view a digital version of this monograph with the videos from the accompanying DVD as well as additional materials, visit http://www.Eyetube.net/unplanned-vitrectomy. Table of Contents 3 Preoperative Evaluation of Problematic Eyes 11 Rationale for a Pars Plana Incision 3 Preventing Complications 12 Vitrectomy Goals and Parameters 5 Early Stages of Complications 13 Getting Started 6 Stages of Complications -

Early Retinal Flow Changes After Vitreoretinal Surgery Optical
Journal of Clinical Medicine Article Early Retinal Flow Changes after Vitreoretinal Surgery in Idiopathic Epiretinal Membrane Using Swept Source Optical Coherence Tomography Angiography 1,2, 3, , 3 4 Rodolfo Mastropasqua y, Rossella D’Aloisio * y, Pasquale Viggiano , Enrico Borrelli , Carla Iafigliola 3, Marta Di Nicola 5, Agbéanda Aharrh-Gnama 3, Guido Di Marzio 3, Lisa Toto 3 , Cesare Mariotti 1 and Paolo Carpineto 3 1 Eye Clinic, Polytechnic University of Marche, 60126 Ancona, Italy; [email protected] (R.M.); [email protected] (C.M.) 2 Institute of Ophthalmology, University of Modena and Reggio Emilia, 41121 Modena, Italy 3 Ophthalmology Clinic, Department of Medicine and Science of Ageing, University G. d’Annunzio Chieti-Pescara, 66100 Chieti, Italy; [email protected] (P.V.); carlaiafi[email protected] (C.I.); [email protected] (A.A.-G.); [email protected] (G.D.M.); [email protected] (L.T.); [email protected] (P.C.) 4 Department of Ophthalmology, University Vita Salute, IRCCS Ospedale San Raffaele, 20132 Milan, Italy; [email protected] 5 Laboratory of Biostatistics, Department of Medical, Oral and Biotechnological Sciences, University G. d’Annunzio Chieti-Pescara, 66100 Chieti, Italy; [email protected] * Correspondence: [email protected] These authors contributed equally to this work and should be considered as co-first authors. y Received: 2 October 2019; Accepted: 18 November 2019; Published: 24 November 2019 Abstract: (1) Background: The aim of this observational cross-sectional work was to investigate early retinal vascular changes in patients undergoing idiopathic epiretinal membrane (iERM) surgery using swept source optical coherence tomography angiography (SS-OCTA); (2) Methods: 24 eyes of 24 patients who underwent vitrectomy with internal limiting membrane (ILM) peeling were evaluated pre- and postoperatively using SS-OCTA system (PLEX Elite 9000, Carl Zeiss Meditec Inc., Dublin, CA, USA). -

Evaluating the Relation of Refractive Surgery and Glaucoma
Editorial Remedy Open Access Published: 25 Jul, 2017 Evaluating the Relation of Refractive Surgery and Glaucoma Kozobolis V*, Kostantinidis A and Labiris G Department of Ophthalmology, University of Thrace, Greece Editorial Laser-assisted refractive corrections constitute a large part of the ophthalmic surgeries that take place every year. It is estimated that about 4 million refractive procedures were performed in 2014 throughout the world. On the other hand, glaucoma is an optic neuropathy, the incidence of which is increasing steadily over time. Given the frequency of refractive surgeries and the incidence of glaucoma in the general population it becomes necessary for the ophthalmologist to assess the risks of a refractive surgery in a glaucoma patient or a patient at a risk of developing glaucoma in the future. The factors to take into consideration are: the family history of glaucoma, intraocular pressure (IOP), myopia, high vertical cup-to-disc ratio, central corneal thickness, and race, other ophthalmic diseases, hypermetropia, previous antiglaucoma procedure, visual fields and modern imaging modalities. The advantages of these modalities include objective and reproducible measurements that can be compared with future measurements. The disadvantage is that their databases (although constantly enriched) include limited number of people, while "unusual" discs (tilted, high ametropias) are excluded from the databases. Unfortunately many candidates for refractive surgery have optic discs with “unusual” appearance that cannot be meaningfully compared with the “normal” optic discs of the databases. In these cases the digital photographing of the optic disc and the comparison with future photos will give valuable information about the changes of both the optic nerve and retinal nerve fibers.