Sub-Bowman's Keratomileusis
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
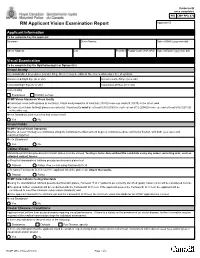
RCMP GRC 2180E (2017-10) Page 1 of 2 Protected B RM Applicant Vision Examination Report Once Completed Applicant ID
Protected B once completed PIB CMP PPU 070 RM Applicant Vision Examination Report Applicant ID Applicant Information To be completed by the applicant Surname Given Names Date of Birth (yyyy-mm-dd) Street Address City Province Postal Code (A9A 9A9) Date of Exam (yyyy-mm-dd) Visual Examination To be completed by the Ophthalmologist or Optometrist Visual Acuity Any standardized procedures (Landoit Ring, Snellen) may be utilized. No error is allowed per line of symbols. Uncorrected Right Eye (6/ or 20/) Uncorrected Left Eye (6/ or 20/) Corrected Right Eye (6/ or 20/) Corrected Left Eye (6/ or 20/) Corrected by Eyeglasses Contact Lenses RCMP Vision Standards Visual Acuity Corrected vision (with glasses or contacts): Visual acuity must be at least 6/6 (20/20) in one eye and 6/9 (20/30) in the other; and Uncorrected vision (without glasses or contacts): Visual acuity must be at least 6/18 (20/60) in each eye or 6/12 (20/40) in one eye and at least 6/30 (20/100) in the other eye. Meets Standards, both corrected and uncorrected? Yes No Visual Fields RCMP Field of Vision Standards Must be at least 150 degrees continuous along the horizontal meridian and 20 degrees continuous above and below fixation, with both eyes open and examined together. Meets Standards? Yes No Colour-Vision Standardized Ishihara pseudo-isochromatic plates must be utilized. Testing is to be done without the candidate using any colour correcting aids, such as coloured contact lenses. a) Result of standardized Ishihara pseudo-isochromatic plates test Passed Failed. If so, re-test using Farnsworth D-15. -

Modern Laser in Situ Keratomileusis Outcomes
REVIEW/UPDATE Modern laser in situ keratomileusis outcomes Helga P. Sandoval, MD, MSCR, Eric D. Donnenfeld, MD, Thomas Kohnen, MD, PhD, FEBO, Richard L. Lindstrom, MD, Richard Potvin, OD, David M. Tremblay, MD, Kerry D. Solomon, MD Laser in situ keratomileusis (LASIK) articles published between 2008 and 2015 that contain clin- ical outcomes data were reviewed and graded for quality, impression, and potential bias. All 97 relevant articles (representing 67 893 eyes) provided a positive or neutral impression of LASIK. Industry bias was not evident. The aggregate loss of 2 or more lines of corrected distance visual acuity was 0.61% (359/58 653). The overall percentage of eyes with uncorrected distance visual acuity better than 20/40 was 99.5% (59 503/59 825). The spherical equivalent refraction was within G1.0 diopter (D) of the target refraction in 98.6% (59 476/60 329) of eyes, with 90.9% (59 954/65 974) within G0.5 D. In studies reporting patient satisfaction, 1.2% (129/9726) of pa- tients were dissatisfied with LASIK. Aggregate outcomes appear better than those reported in summaries of the safety and effectiveness of earlier laser refractive surgery systems approved by the U.S. Food and Drug Administration. Modern results support the safety, efficacy, and patient satisfaction of the procedure. Financial Disclosure: Proprietary or commercial disclosures are listed after the references. J Cataract Refract Surg 2016; 42:1224–1234 Q 2016 ASCRS and ESCRS Laser in situ keratomileusis (LASIK) is one of the most have been performed globally.1 Laser in situ keratomil- commonly performed elective procedures in the United eusis was introduced by Pallikaris et al.2 in 1990. -

Early Postoperative Rotational Stability and Its Related Factors of a Single-Piece Acrylic Toric Intraocular Lens
Eye (2020) 34:474–479 https://doi.org/10.1038/s41433-019-0521-0 ARTICLE Early Postoperative Rotational stability and its related factors of a single-piece acrylic toric intraocular lens 1,2 3 4 5 1 1 1 Shuyi Li ● Xi Li ● Suhong He ● Qianyin Zheng ● Xiang Chen ● Xingdi Wu ● Wen Xu Received: 30 November 2018 / Accepted: 18 June 2019 / Published online: 12 July 2019 © The Author(s) 2019. This article is published with open access Abstract Purpose In the present study, we aimed to evaluate the early postoperative rotational stability of TECNIS toric intraocular lens (IOL) and analyse its correlation with preoperative and intraoperative parameters. Methods A total of 102 eyes from 87 cataract patients who underwent implantation of TECNIS toric IOL during July 2016 to November 2017 were enrolled in this retrospective study. Preoperative parameters including corneal astigmatism, axial length (AL), lens thickness (LT), anterior chamber depth (ACD) and sulcus-to-sulcus (STS), were determined. The area of capsulorhexis was measured with Rhinoceros 5.0 software. The follow-up examinations including the residual astigmatism (RAS) and postoperative toric IOL axis, were performed at 1 month and 3 months after surgery. − − 1234567890();,: 1234567890();,: Results RAS was 0.84 ± 0.88 D at 1 month and 0.81 ± 0.89 D at 3 months after surgery. The rotation of toric IOL at 3 months was 4.83 ± 3.65°. The Pearson’s r of ACD, horizontal and vertical STS, and toric IOL target axis was 0.011, 0.039, 0.045 and 0.082. The toric IOL rotation was positively correlated with the area of capsulorhexis (r = 0.522, P = 0.0003), LT (r = 0.288, P = 0.003) and AL (r = 0.259, P = 0.009). -

Ophthalmology Abbreviations Alphabetical
COMMON OPHTHALMOLOGY ABBREVIATIONS Listed as one of America’s Illinois Eye and Ear Infi rmary Best Hospitals for Ophthalmology UIC Department of Ophthalmology & Visual Sciences by U.S.News & World Report Commonly Used Ophthalmology Abbreviations Alphabetical A POCKET GUIDE FOR RESIDENTS Compiled by: Bryan Kim, MD COMMON OPHTHALMOLOGY ABBREVIATIONS A/C or AC anterior chamber Anterior chamber Dilators (red top); A1% atropine 1% education The Department of Ophthalmology accepts six residents Drops/Meds to its program each year, making it one of nation’s largest programs. We are anterior cortical changes/ ACC Lens: Diagnoses/findings also one of the most competitive with well over 600 applicants annually, of cataract whom 84 are granted interviews. Our selection standards are among the Glaucoma: Diagnoses/ highest. Our incoming residents graduated from prestigious medical schools ACG angle closure glaucoma including Brown, Northwestern, MIT, Cornell, University of Michigan, and findings University of Southern California. GPA’s are typically 4.0 and board scores anterior chamber intraocular ACIOL Lens are rarely lower than the 95th percentile. Most applicants have research lens experience. In recent years our residents have gone on to prestigious fellowships at UC Davis, University of Chicago, Northwestern, University amount of plus reading of Iowa, Oregon Health Sciences University, Bascom Palmer, Duke, UCSF, Add power (for bifocal/progres- Refraction Emory, Wilmer Eye Institute, and UCLA. Our tradition of excellence in sives) ophthalmologic education is reflected in the leadership positions held by anterior ischemic optic Nerve/Neuro: Diagno- AION our alumni, who serve as chairs of ophthalmology departments, the dean neuropathy ses/findings of a leading medical school, and the director of the National Eye Institute. -

Medical Treatment of Operative Corneal Perforation Caused By
CASE REPORTS AND SMALL CASE SERIES and clinical course of a patient with the stromal bed was thin; in the left Medical Treatment a LASIK-induced corneal perfora- eye, the corneal flap was very edema- of Operative Corneal tion that affected the final visual acu- tous and a space was visible between Perforation Caused ity. We believe that this report on the the corneal flap and the stromal bed treatment and recovery of the cor- (Figure 1, left). The anterior cham- by Laser In Situ neal perforation will be valuable in- ber was very shallow, and aqueous Keratomileusis formation for refractive surgeons. humor was observed to leak onto the ocular surface with blinking (Figure Laser in situ keratomileusis (LASIK) Report of a Case. A 33-year-old man 1, right). A round, 0.25-mm diam- is an effective procedure to treat a was referred to us with a complaint eter perforation site was observed in wide range of myopia.1 The advan- of decreased visual acuity in the left the center of the stromal bed by slit- tages of LASIK over photorefrac- eye after bilateral simultaneous lamp examination. tive keratectomy (PRK) are rapid vi- LASIK performed 3 days previ- We treated the corneal perfo- sual recovery, lower risk of corneal ously at a different facility. A cor- ration by applying a therapeutic soft haze, greater regression of myopia, neal perforation was noticed in the contact lens with topical antibiot- and less postoperative pain.1-3 How- left eye during LASIK laser abla- ics, oral carbonic anhydrase inhibi- ever, LASIK requires more skillful tion in this eye. -

Evaluating the Relation of Refractive Surgery and Glaucoma
Editorial Remedy Open Access Published: 25 Jul, 2017 Evaluating the Relation of Refractive Surgery and Glaucoma Kozobolis V*, Kostantinidis A and Labiris G Department of Ophthalmology, University of Thrace, Greece Editorial Laser-assisted refractive corrections constitute a large part of the ophthalmic surgeries that take place every year. It is estimated that about 4 million refractive procedures were performed in 2014 throughout the world. On the other hand, glaucoma is an optic neuropathy, the incidence of which is increasing steadily over time. Given the frequency of refractive surgeries and the incidence of glaucoma in the general population it becomes necessary for the ophthalmologist to assess the risks of a refractive surgery in a glaucoma patient or a patient at a risk of developing glaucoma in the future. The factors to take into consideration are: the family history of glaucoma, intraocular pressure (IOP), myopia, high vertical cup-to-disc ratio, central corneal thickness, and race, other ophthalmic diseases, hypermetropia, previous antiglaucoma procedure, visual fields and modern imaging modalities. The advantages of these modalities include objective and reproducible measurements that can be compared with future measurements. The disadvantage is that their databases (although constantly enriched) include limited number of people, while "unusual" discs (tilted, high ametropias) are excluded from the databases. Unfortunately many candidates for refractive surgery have optic discs with “unusual” appearance that cannot be meaningfully compared with the “normal” optic discs of the databases. In these cases the digital photographing of the optic disc and the comparison with future photos will give valuable information about the changes of both the optic nerve and retinal nerve fibers. -

Vitreoretinal Surgery for Macular Hole After Laser Assisted in Situ
1423 Br J Ophthalmol: first published as 10.1136/bjo.2005.074542 on 18 October 2005. Downloaded from SCIENTIFIC REPORT Vitreoretinal surgery for macular hole after laser assisted in situ keratomileusis for the correction of myopia J F Arevalo, F J Rodriguez, J L Rosales-Meneses, A Dessouki, C K Chan, R A Mittra, J M Ruiz- Moreno ............................................................................................................................... Br J Ophthalmol 2005;89:1423–1426. doi: 10.1136/bjo.2005.074542 macular hole between March 1996 and March 2003 at seven Ams: To describe the characteristics and surgical outcomes institutions in Venezuela, Colombia, Spain, and the United of full thickness macular hole surgery after laser assisted in States. Preoperative examination including a thorough situ keratomileusis (LASIK) for the correction of myopia. dilated funduscopy with indirect ophthalmoscopy, and slit Methods: 13 patients (14 eyes) who developed a macular lamp biomicroscopy was performed by a retina specialist and/ hole after bilateral LASIK for the correction of myopia or a refractive surgeon. Patients were female in 60.7% of participated in the study. cases, and underwent surgical correction of myopia ranging Results: Macular hole formed 1–83 months after LASIK from 20.75 to 229.00 dioptres (D) (mean 26.19 D). Patients (mean 13 months). 11 out of 13 (84.6%) patients were were followed for a mean of 65 months after LASIK (range female. Mean age was 45.5 years old (25–65). All eyes 6–84 months). Patients who underwent vitreoretinal surgery were myopic (range 20.50 to 219.75 dioptres (D); mean to repair the macular hole were included in the study 28.4 D). -

Patient-Reported Outcomes 5 Years After Laser in Situ Keratomileusis
ARTICLE Patient-reported outcomes 5 years after laser in situ keratomileusis Steven C. Schallhorn, MD, Jan A. Venter, MD, David Teenan, MD, Stephen J. Hannan, OD, Keith A. Hettinger, MS, Martina Pelouskova, MSc, Julie M. Schallhorn, MD PURPOSE: To assess vision-related, quality-of-life outcomes 5 years after laser in situ keratomileusis (LASIK) and determine factors predictive of patient satisfaction. SETTING: Optical Express, Glasgow, Scotland. DESIGN: Retrospective case series. METHODS: Data from patients who had attended a clinical examination 5 years after LASIK were analyzed. All treatments were performed using the Visx Star S4 IR excimer laser. Patient- reported satisfaction, the effect of eyesight on various activities, visual phenomena, and ocular discomfort were evaluated 5 years postoperatively. Multivariate regression analysis was performed to determine factors affecting patient satisfaction. RESULTS: The study comprised 2530 patients (4937 eyes) who had LASIK. The mean age at the time of surgery was 42.4 years G 12.5 (SD), and the preoperative manifest spherical equivalent ranged from À11.0 diopters (D) to C4.88 D. Five years postoperatively, 79.3% of eyes were within G0.50 D of emmetropia and 77.7% of eyes achieved monocular uncorrected distance visual acuity (UDVA) and 90.6% of eyes achieved binocular UDVA of 20/20 or better. Of the patients, 91.0% said they were satisfied with their vision and 94.9% did not wear distance correction. Less than 2.0% of patients noticed visual phenomena, even with spectacle correction. Major predictors of patient satisfaction 5 years postoperatively were postoperative binocular UDVA (37.6% variance explained by regression model), visual phenomena (relative contribution of 15.0%), preoperative and postop- erative sphere and their interactions (11.6%), and eyesight-related difficulties with various activities such as night driving, outdoor activities, and reading (10.2%). -

Eleven-Year Follow-Up of Laser in Situ Keratomileusis
J CATARACT REFRACT SURG - VOL 33, FEBRUARY 2007 ARTICLES Eleven-year follow-up of laser in situ keratomileusis George D. Kymionis, MD, PhD, Nikolaos S. Tsiklis, MD, Nikolaos Astyrakakis, OD, Aristofanis I. Pallikaris, PhD, Sophia I. Panagopoulou, PhD, Ioannis G. Pallikaris, MD, PhD PURPOSE: To report the long-term (11-year) outcomes (stability and complications) of laser in situ ker- atomileusis (LASIK) in patients with high myopia. SETTING: University refractive surgery center. METHODS: Seven patients (4 with bilateral treatment and 3 with unilateral treatment) who had my- opic LASIK and completed 11 years of follow-up were included in the study. RESULTS: The mean age of the 2 men and 5 women was 41.7 years G 6.5 (SD) (range 34 to 50 years). The mean follow-up was 140.18 G 6.70 months (range 132 to 150 months). At 11 years, the spherical equivalent error was statistically significantly reduced, from a mean of À12.96 G 3.17 diopters (D) (range À19.00 to À10.00 D) before LASIK to a mean of À1.14 G 1.67 D (range À4.25 to 1.00 D) after (P<.001). Predictability of postoperative refraction 6 months and 11 years after LASIK showed that 6 eyes (55%) were within G1.00 D of intended correction. No late postoperative complications occurred. Five patients (8 eyes, 73%) were satisfied with the final outcome. CONCLUSIONS: Laser in situ keratomileusis was moderately predictable in the correction of high de- grees of myopia. After the sixth postoperative month, refractive and topographic stability were ob- tained. -

Irregular Astigmatism After Corneal Transplantation—Efficacy And
CLINICAL SCIENCE Irregular Astigmatism After Corneal Transplantation—Efficacy and Safety of Topography-Guided Treatment Inês Laíns, MD, MSc,*† Andreia M. Rosa, MD,*† Marta Guerra, MD, MSc,* Cristina Tavares, MD,* Conceição Lobo, MD, PhD,*† Maria F. L. Silva, PhD,‡ Maria J. Quadrado, MD, PhD,*† and Joaquim N. Murta, MD, PhD*† Key Words: astigmatism, corneal topography, corneal transplanta- Purpose: fi To analyze the ef cacy and safety of topography-guided tion, excimer, photorefractive keratectomy photorefractive keratectomy (TG-PRK) to treat irregular astigmatism after corneal transplantation. (Cornea 2016;35:30–36) Methods: This was a retrospective observational case series. Eyes with irregular astigmatism after penetrating keratoplasty treated with orneal transplantation (CT) is one of the most commonly TG-PRK (Allegretto Wave Eye-Q) with the topography-guided Cperformed transplant procedures throughout the world.1 customized ablation treatment protocol were included. All treatments Although it is generally successful, patients frequently present had been planned to correct the topographic irregularities, as well as with high irregular postoperative astigmatism, which pre- to reduce the refractive error after neutralizing the induced refractive cludes them from achieving satisfactory visual acuity.2 It can change. Clinical records, treatment plan, and the examinations affect up to 40% of the eyes3 and remains a challenge even for performed were reviewed and the following data were collected: experienced cornea specialists, as spectacles and rigid contact corrected and uncorrected distance visual acuities; manifest refrac- lenses often represent an unsuccessful option for visual tion; topographic parameters, and corneal endothelial cell count. rehabilitation.4 Results: We included 31 eyes [30 patients; mean age 45.0 6 13.4 In recent decades, excimer laser treatment has emerged 5 (SD) years]. -

Nd:YAG Laser for Epithelial Ingrowth After Laser in Situ Keratomileusis
Int Ophthalmol (2019) 39:1225–1230 https://doi.org/10.1007/s10792-018-0923-1 ORIGINAL PAPER Nd:YAG laser for epithelial ingrowth after laser in situ keratomileusis Osama Ali Mohammed . Amr Mounir . Amin Aboali Hassan . Alahmady Hamad Alsmman . Engy Mohamed Mostafa Received: 28 November 2017 / Accepted: 13 April 2018 / Published online: 4 May 2018 Ó Springer Science+Business Media B.V., part of Springer Nature 2018 Abstract Results Epithelial ingrowth was treated successfully Purpose To evaluate the efficacy of neodymium:yt- in all 41 eyes. The uncorrected visual acuities were trium–aluminum–garnet (Nd:YAG) laser for treat- 20/20, and there was no evidence of recurrent ment of epithelial ingrowth after laser in situ epithelial ingrowth after 6 months with no complica- keratomileusis (LASIK). tions reported. Patients and methods Fifty-eight patients with Conclusion YAG laser is a simple, effective outpa- epithelial ingrowth presented to Sohag refractive tient procedure for the management of epithelial center, Sohag, Egypt, between January 2015 and ingrowth after LASIK. March 2017. Only 41 patients (18 females and 23 males, mean age: 33.4 years) involving 41 eyes were Keywords Nd:YAG Á Epithelial ingrowth Á Laser indicated for treatment by Nd:YAG laser as the rest of in situ keratomileusis the eyes were only under observation. Patients with epithelial ingrowth were recognized at a mean of 6 months after primary LASIK procedure (range: 2–16 months). Four eyes had undergone previous Introduction LASIK enhancements. Four eyes had the epithelial ingrowth removed by flap lift and scrapping. The mean Flap-related complications after laser in situ ker- intensity of the spots used was 0.8 mJ with variable atomileusis (LASIK) are not uncommon [1]. -

Icd-9-Cm (2010)
ICD-9-CM (2010) PROCEDURE CODE LONG DESCRIPTION SHORT DESCRIPTION 0001 Therapeutic ultrasound of vessels of head and neck Ther ult head & neck ves 0002 Therapeutic ultrasound of heart Ther ultrasound of heart 0003 Therapeutic ultrasound of peripheral vascular vessels Ther ult peripheral ves 0009 Other therapeutic ultrasound Other therapeutic ultsnd 0010 Implantation of chemotherapeutic agent Implant chemothera agent 0011 Infusion of drotrecogin alfa (activated) Infus drotrecogin alfa 0012 Administration of inhaled nitric oxide Adm inhal nitric oxide 0013 Injection or infusion of nesiritide Inject/infus nesiritide 0014 Injection or infusion of oxazolidinone class of antibiotics Injection oxazolidinone 0015 High-dose infusion interleukin-2 [IL-2] High-dose infusion IL-2 0016 Pressurized treatment of venous bypass graft [conduit] with pharmaceutical substance Pressurized treat graft 0017 Infusion of vasopressor agent Infusion of vasopressor 0018 Infusion of immunosuppressive antibody therapy Infus immunosup antibody 0019 Disruption of blood brain barrier via infusion [BBBD] BBBD via infusion 0021 Intravascular imaging of extracranial cerebral vessels IVUS extracran cereb ves 0022 Intravascular imaging of intrathoracic vessels IVUS intrathoracic ves 0023 Intravascular imaging of peripheral vessels IVUS peripheral vessels 0024 Intravascular imaging of coronary vessels IVUS coronary vessels 0025 Intravascular imaging of renal vessels IVUS renal vessels 0028 Intravascular imaging, other specified vessel(s) Intravascul imaging NEC 0029 Intravascular